Miscarriage
Miscarriage, also known in medical terms as a spontaneous abortion and pregnancy loss, is the natural death of an embryo or fetus before it is able to survive in-dependently.
Quotes
[edit]- It is important to note once again that the prohibition of murder and abortion must be appreciated in a therapeutic, not a juridical or punitive light, with which such offenses are often regarded in most Western moral, philosophical, and theological systems: the goal is not to subject the sinner to just punishment, but to bring the sinner through repentance and God’s grace to holiness.
Because of this perspective the Orthodox Church never endorsed a doctrine of double effect, such as developed in the West, which allowed Roman Catholicism to approve of indirect abortions. The doctrine of double effects holds that when an action produces two effects, one good and one evil, one may nevertheless act, as long as the act is not evil in itself, the good effect is not produced by the bad effect, the evil effect is not intended,, and there is a proportionate reason (more good will be produced than evil). According to the doctrine of double effect, when these conditions are fulfilled, one is held to be juridically innocent In contrast, the Orthodox Church recognizes that close causal involvement in the death of another, whether a guilty or an innocent person, may harm one’s spiritual life. Orthodox Christianity recognizes harms from both involuntary and “justifiable” homicide, including homicide in a just war, both of which incur excommunication not as punishment, but as spiritual therapy (Basil, 1983, Canon 13, pp. 801-802).
It is in this spiritually therapeutic context that one should understand the absolution of women who miscarry. The absolution expresses the Orthodox Christian healing approach to the involuntary loss of life.- H. Trisram Engelhardt, Jr. Orthodox, “Christian Bioethics: Medical Morality in the Mind of the Fathers”, in "Religious Perspectives on Bioethics". Taylor & Francis. Mark Cherry; John F. Peppin (2013). pp.27-28
- The woman who has suffered a miscarriage is not held to be guilty in a juridical sense, but in need of God’s loving grace. It is within this therapeutic perspective that the Orthodox Church approaches decisions made by women to engage in operations that will also incidentally lead to the abortion of a child (e.g., the removal of a cancerous uterus containing an unborn child), which in Roman Catholic terms would not count as an abortion. In such cases, the spiritual father must help the patient through repentance and love to repair the spiritual damage from the serious evil of involvement in the death of another person.
- H. Trisram Engelhardt, Jr., “Orthodox Christian Bioethics: Medical Morality in the Mind of the Fathers”, in "Religious Perspectives on Bioethics". Taylor & Francis. Mark Cherry; John F. Peppin (2013), p. 28
- Because spontaneous miscarriage and self-managed abortion are medically indistinguishable in most cases, prohibitions on abortion will predictably lead to the investigation and detention of many women experiencing miscarriages as well as those self-managing abortions.
- Foley Hoag LLP on behalf of the Global Justice Center, Amnesty International USA, Human Rights Watch, National Birth Equity Collaborative, Physicians for Human Rights, Pregnancy Justice, “UN Special Procedures Letter US Abortion Rights”, (March 2, 2023), pp.18-19
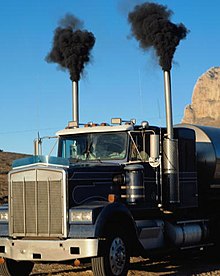
However, the latest study is the first to assess the impact of short-term exposure to air pollution. It found that raised levels of nitrogen dioxide (NO2) pollution that are commonplace around the world increased the risk of losing a pregnancy by 16%.
“It’s pretty profound,” said Dr Matthew Fuller, at the University of Utah’s department of emergency medicine and one of the research team. “If you compare that increase in risk to other studies on environmental effects on the foetus, it’s akin to tobacco smoke in first trimester pregnancy loss.” NO2 is produced by fuel burning, particularly in diesel vehicles. ~ Matthew Fuller
- The effect of long-term exposure to dirty air on the risk of miscarriage has been analysed previously. Studies from Brazil to Italy to Mongolia found a link, but others failed to do so.
However, the latest study is the first to assess the impact of short-term exposure to air pollution. It found that raised levels of nitrogen dioxide (NO2) pollution that are commonplace around the world increased the risk of losing a pregnancy by 16%.
“It’s pretty profound,” said Dr Matthew Fuller, at the University of Utah’s department of emergency medicine and one of the research team. “If you compare that increase in risk to other studies on environmental effects on the foetus, it’s akin to tobacco smoke in first trimester pregnancy loss.” NO2 is produced by fuel burning, particularly in diesel vehicles.- Matthew Fuller in “Air pollution 'as bad as smoking in increasing risk of miscarriage'”, by Damian Carrington, The Guardian, (11 Jan 2019)
- Few studies on job stress relative to pregnancy have been carried out, but both animal and epidemiological studies have shown effect of exposure to stressful conditions during pregnancy and adverse effects on the offspring.
- Larsen AD, “The effect of maternal exposure to psychosocial job strain on pregnancy outcomes and child development”, Dan Med J. 2015 Feb;62(2):B5015.
- Obesity has become a major health problem across the world. In the UK, obesity affects one‐fifth of the female population ( Anonymous, 2001 ). Maternal obesity has been reported as a risk factor for adulthood obesity in offspring ( Parsons et al ., 2001 ). Obesity may also lead to a poor pregnancy out-come, such as sudden and unexplained intrauterine death ( Froen et al ., 2001 ), and in women with polycystic ovary syndrome (PCOS) receiving infertility treatment is associated with an increased risk of miscarriage ( Hamilton‐Fairley et al ., 1992 ; Wang et al ., 2000 ). However, in the general population there is less evidence for a link between obesity and spontaneous miscarriage ( Risch et al ., 1990 ).
- H Lashen, K Fear, D W Sturdee, “Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study “, Hum Reprod. 2004 Jul;19(7):1644-6.
- Spontaneous miscarriage affects 12–15% of all pregnancies ( Zinman et al ., 1996 ). Eighty percent of miscarriages occur before 12 weeks of gestation, and the majority are due to chromosomal abnormalities (Harlap et al ., 1980). Our figures from this study population are consistent with previously published data.
The risk of miscarriage after the detection of a fetal heart on ultrasound scan is reduced to 5%, except in patients who have had recurrent miscarriages ( van Leeuwen et al ., 1993 ).
Many factors have been described to increase the risk of spontaneous miscarriage; however, obesity was not found to be a risk factor by Risch et al . (1990) . Recent evidence indicated that obese women undergoing infertility treatment were at increased risk of spontaneous miscarriage ( Hamilton‐Fairley et al ., 1992 ; Wang et al ., 2000 ). However, this point has also been controversial (Lashen et al ., 1999 ; Roth et al., 2003 ).- H Lashen, K Fear, D W Sturdee, “Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study“, Hum Reprod. 2004 Jul;19(7)
- From a medical perspective, there is no physically significant difference between a medication abortion and a spontaneously occurring miscarriage. For example, the medicines used in medication abortion are used to help safely manage an incomplete miscarriage.
- NWHN Staff, “Consumer Health Info: Medication Abortion and Miscarriage” (updated 15 Aug. 2019),
- Overweight women are more likely to miscarry a healthy baby, according to research involving 204 women who had suffered a miscarriage.
The researchers said the findings back up advice that obese women should lose weight before trying to conceive.
"The excess miscarriage rate in overweight and obese women is due to the loss of chromosomally normal embryos," said Dr Inna Landres of Stanford University School of Medicine. "It's important to identify elevated BMI [body mass index] as a risk factor for miscarriage and counsel those women who are affected on the importance of lifestyle modification- James Randerson, “Overweight women are more likely to miscarry healthy fetuses” , The Guardian, (13 Nov 2008)
- Occupational studies included in this review found that several occupational and non-occupational factors influenced reproductive outcomes. Occupational factors involved were standing, lifting and exposure to chemicals—usually persons who were exposed to noise were exposed to other occupational factors. Important non-occupational factors were mother’s age, mothers weight and height, mother’s weight gain during pregnancy, smoking, education, race and socioeconomic status. Gravidity and parity, and chronic diseases of the mother were also important factors for examination of spontaneous abortion or preterm labour.
- Gordana Ristovska, Helga Elvira Laszlo, and Anna L. Hansell; “Reproductive Outcomes Associated with Noise Exposure — A Systematic Review of the Literature”, Int J Environ Res Public Health. 2014 Aug; 11(8): 7931–7952.
- New multi-disciplinary research on brain–body interactions triggered by stress in early pregnancy has shown that maternal biological responses, including localized inflammation in uterine tissue and sustained depression of progesterone production, challenge the endocrine-immune steady state during pregnancy, leading to serious consequences for the fetal environment. Recent basic science findings and new theoretical development around a ‘pregnancy stress syndrome’ associated with over-activation of the HPA axis warrant a new look at the epidemiological evidence around the age-old question of whether or not stress can actually cause human reproductive failure.
- Gordana Ristovska, Helga Elvira Laszlo, and Anna L. Hansell; “Reproductive Outcomes Associated with Noise Exposure — A Systematic Review of the Literature”, Int J Environ Res Public Health. 2014 Aug; 11(8): 7931–7952.
- Dr Sarah Stock, at the University of Edinburgh and not part of the research team, said: “Air pollution is clearly detrimental to the health of millions of mothers, babies and children worldwide. Measures to reduce the impact of air pollution are crucial to ensure the health of future generations.”
- Sarah Stock in “Air pollution 'as bad as smoking in increasing risk of miscarriage'”, by Damian Carrington, The Guardian, (11 Jan 2019)
- We always write stories of tragedies because that's how we reach our human depth. How we get to the other side of it. We look at the cruelty, the darkness and horrific events that happened in our life whether it be a miscarriage or a husband who is not faithful. Then you find this ability to transcend. And that is called the passion, like the passion of Christ. You could call this the passion of Frida Kahlo, in a way.
When I talk about passion, and I'm not a religious person, but I absolutely am drawn and attracted to the power of religious art because it gets at that most extreme emotion of the human experience.- Julie Taymor, "Bill Moyers Interviews Julie Taymor" at PBS (25 October 2002).
- Fetus death risk reduction is included in the United Nations Sustainable Development Goals. However, little is known about how missed abortion in the first trimester (MAFT) is related to maternal air pollution exposure. We quantify the link between air pollution exposure and MAFT in Beijing, China, a region with severe MAFT and air quality problems. We analyse the records of 255,668 pregnant women from 2009 to 2017 and contrast them with maternal exposure to air pollutants (particulate matter PM2.5, SO2, O3 and CO). We adjust for confounding factors such as sociodemographic characteristics, spatial autocorrelation and ambient temperature. We find that, for all four pollutants, an increased risk of MAFT is associated with rises in pollutant concentrations and the adjusted odds ratios (ORs) of these associations increase with higher concentrations. For example, the adjusted OR of MAFT risk for a 10.0 μg m−3 increase in SO2 exposure is between 1.29 and 1.41 at concentrations of 7.1–19.5 μg m−3; it drops to 1.17 below this range and rises to 1.52 above it at higher SO2 concentrations. This means that the risk increase is not linear but becomes more severe the higher the pollutant concentration. The findings provide evidence linking fetus disease burden and maternal air pollution exposure.
- Liqiang Zhang, Weiwei Liu, Kun Hou, Jintai Lin, Chenghu Zhou, Xiaohua Tong, Ziye Wang, Yuebin Wang, Yanxiao Jiang, Ziwei Wang, Yibo Zheng, Yonglian Lan, Suhong Liu, Ruijing Ni, Mengyao Liu & Panpan Zhu; “Air pollution-induced missed abortion risk for pregnancies”, Nature Sustainability, volume 2, (14 October 2019)
"Leisure time physical exercise during pregnancy and the risk of miscarriage: a study within the Danish National Birth Cohort” (2007)
[edit]M Madsen, T Jørgensen, ML Jensen, M Juhl,a J Olsen, PK Andersen, A-M Nybo Andersen; "Leisure time physical exercise during pregnancy and the risk of miscarriage: a study within the Danish National Birth Cohort”, BJOG. 2007 Nov 1; 114(11): 1419–1426, (2007 Sep 18).
- In the existing body of literature, exercise during pregnancy has generally not been associated with miscarriage,17–19 and one case–control study has even reported a protective effect of exercise during pregnancy.20 In contrast, Hjollund et al.21 found an increased risk of early miscarriage among women who reported a high physical strain around the time of implantation of the embryo.
Furthermore, lay people have tried to use excessive physical exercise as abortificant, and older literature mentions physical activity (e.g. jumping, running, and horseback riding) as a cause of miscarriage.
Considering the relatively sparse literature and the somewhat inconsistent results, we wanted to examine the association between exercise during pregnancy and miscarriage in a large population-based cohort. - The main results based on the total data material showed that an increasing amount of time spent on exercise was associated with a greater risk of miscarriage compared with nonexercisers. Exercising 1–44 minutes/week was not associated with an increased risk of miscarriage.
- In this study based on data from nearly 93 000 women, a dose-response relation was seen for the association between amount of weekly exercise and the risk of miscarriage early in pregnancy. Certain types of exercise, and particularly high impact types of exercise, were found to be associated with a higher risk of miscarriage. In the analyses based only on prospectively collected exposure data, the association did, however, attenuate, indicating a certain degree of recall bias. An alternative explanation to recall bias may be that exercise only in the early stages of pregnancy has an adverse effect on pregnancy outcome. In this case, the difference in the HRs between the analyses based on the total data material and the subcohort of only prospectively collected data is not as much a result of the mode of data collection as a reflection of the fact that the total data material encompasses the very early miscarriages. Even within the subperiods of gestational age the miscarriages occur earlier for the pregnancies with retrospectively collected exposure information than for pregnancies with a first pregnancy interview (Figure 2). In addition, we did see a positive trend in the association between exercise and the risk of miscarriages in the earliest period of pregnancy (gestational weeks 11–14) in the subcohort using prospectively collected data only.
- It is difficult to investigate very early miscarriages using prospectively collected exposure information, since the time period, in which collection of exposure information must take place, that is the time from detection of pregnancy to the occurrence of an early miscarriage, is short.
- Only few previous studies have investigated the association between exercise and miscarriage. The only study, which clearly supports our findings, is a cohort study, which concluded that self-reported physical strain around the time of implantation (days 6–9 after ovulation) was associated with an in-creased risk of miscarriage (HR 2.5, 95% CI = 1.3–4.6). In contrast, Latka et al found a reduced risk of miscarriage with no chromosome defect in women who exercised compared with those who did not (OR = 0.5, 95% CI = 0.3–1.0). The case–control design was, however, based on a hypothesis that exercise cannot lead to chromosome aberrations in the fetus, as the control group consisted of women with miscarriages with chromosome aberrations. This assumption may be questioned since mode of action is unknown. In a small prospective study, Clapp found no statistically significant difference in risk of miscarriage between recreational runners (n = 49), aerobic dancers (n = 39) and a control group of active women, who had stopped exercising before the time of conception (n = 29). The study population was in excellent condition and had been exercising for years prior to the pregnancy, and the results may not be representative of the population at large. Two other studies have only investigated late miscarriages.
“Superfertility is more prevalent in obese women with recurrent early pregnancy miscarriage“ (2015)
[edit]HM Bhandari, BK Tan, S Quenby; [1]ry.wiley.com/doi/full/10.1111/1471-0528.13806 “Superfertility is more prevalent in obese women with recurrent early pregnancy miscarriage“], BJOG, Volume 123, Issue 2, (29 December 2015)
- Miscarriage remains the most common complication of pregnancy despite many advances in the understanding of early pregnancy. Loss of three or more consecutive pregnancies before 24 weeks of gestation is the most acceptable definition for recurrent miscarriage (RMC) in Europe, but has recently been defined by the American Society for Reproductive Medicine as a disease with two or more failed pregnancies. Despite best efforts to identify the underlying causes for RMC, it remains ‘unexplained’ in the majority of cases. Chromosomal errors appear to be common in the pre-implantation developing embryos6, 7 which predispose to increased risk of pregnancy losses. High rates of chromosomally abnormal cells within human embryos mean that the reproductive success is dependent on the endometrial ability to distinguish between normal and abnormal embryos. In vitro studies have provided convincing evidence that perturbation in the bio‐sensor function of the decidualised endometrium is an important mechanism underpinning RMC.
- Our study findings are supportive of the concept that increased female BMI may have a negative in-fluence on the early pregnancy outcome. We found a significant positive correlation between the BMI and first trimester pregnancy losses and anembryonic miscarriages. There were also significantly more first trimester miscarriages in obese women than in normal weight or overweight women with recurrent miscarriage.
- A study that examined miscarriage type and fetal karyotypes in RMC women found that very early pregnancy losses (anembryonic and embryonic loss with embryo <3 mm) are more likely to be karyotypically normal and embryonic miscarriage (with embryo ≥3 mm) and fetal demise to be karyotypically more likely abnormal.36 It is possible to speculate from our study findings that obesity is likely to be associated with an increased risk of first trimester miscarriages and, in particular, increases the risk of miscarriage of anembryonic pregnancies, which are likely to be karyotypically normal. However, it re-mains uncertain whether BMI may have any significant effect on the embryo loss pattern, and further well‐controlled studies are required to analyse their association.
- It is likely that an alternate mechanism exists in obesity that may be responsible for ‘biological super-fertility’ in obese women. Teklenburg et al.40 elegantly showed that the endometrial stromal cells transform into biological sensors of embryo quality upon decidualisation. There is a good body of evidence, from in vitro studies, to suggest that inability of the peri‐implantation endometrium to mount an adequate decidual response, impairs embryo recognition and selection upon implantation,34, 40, 41, 43 which leads to shorter TTP intervals and predisposes to RMC. This abnormal phenotype results in an extended window of implantation, which reduces the endometrial ability to be ‘selective’ in response to embryo quality.8 This concept is consistent with the previously reported association of late implantation of embryos with an increased risk of early miscarriage.44 The findings from our study may suggest that an obesogenic environment might have a negative influence on the peri‐implantation endometrium, which would predispose women to RMC.
- Our study findings support the concept of ‘biological superfertility’ in women with RMC and present a unique finding that superfertility may be more prevalent in obese women with a history of RMC. Further prospective studies in women with idiopathic RMC are required to confirm the association of BMI, RMC and superfertility. If confirmed, further investigation is required to understand why obesity predisposes to superfertility. It is likely that superfertility may be linked to impaired endometrial development in the peri‐implantation period; further research to describe the peri‐implantation endometrium in obese women and to study the exact mechanism by which obesity affects the endometrium is required. Clinical trials with therapeutic targets to improve decidualisation and thus reproductive outcome in obese women could hold significant clinical potential.
"Miscarriage misconceptions boost feelings of guilt and shame, study says" (2015)
[edit]Haroon Sadique, "Miscarriage misconceptions boost feelings of guilt and shame, study says", The Guardian, (11 May 2015)
- A significant number of the respondents were under misapprehensions as to what caused the loss of the pregnancy. Three-quarters believed that a stressful event could bring about a miscarriage, 64% thought that lifting a heavy object could be a cause, and a fifth that previous use of oral contraceptives could induce pregnancy loss.
- Of those who took part 15% said they or their partner had suffered a miscarriage, but the majority of respondents (55%) believed that miscarriages are uncommon (defined as less than 6% of all pregnancies). The truth is that miscarriages end one in four pregnancies and are by far the most common pregnancy complication, the paper says.
A fifth of people incorrectly believed that lifestyle choices during pregnancy, such as smoking or using drugs or alcohol, were the single most common cause of miscarriage, more common than genetic or medical causes. In reality, 60% of miscarriages are caused by a genetic problem. - The authors concluded: “Patients who have experienced miscarriage may benefit from further counseling by healthcare providers, identification of the cause, and revelations from friends and celebrities. Healthcare providers have an important role in assessing and educating all pregnant patients about known prenatal risk factors, diminishing concerns about unsubstantiated but prevalent myths and, among those who experience a miscarriage, acknowledging and dissuading feelings of guilt and shame.”
Dialogue
[edit]- Q: The moment in your special that really made me gasp out loud is when you joke about how you suffered a miscarriage before, and how you were secretly relieved because they were twins. Do you think that joke only works because the audience could see that you got pregnant again so there is redemption to the loss?
- Ali Wong: I think that’s part of it, for sure. But it really helped me when I had a miscarriage to talk to other women and hear that they’d been through it, too. It’s one thing to hear the statistics but it’s another to put faces to the numbers so you stop feeling like it’s your fault. I think that’s one of the reasons women don’t tell people when they’ve had a miscarriage – they think it’s their fault. I remember I worried what my in-laws would think, which is so crazy. I thought they’d think their son had married a terrible person. Also, because I made the mistake of telling people as soon as I got pregnant, I then had to tell them the bad news and then I felt like I was burdening them. So being able to joke about it was such a relief.
Comedy only works when it comes from an honest place and the relief that I’d miscarried twins was real!
- Ali Wong in "Ali Wong: 'Being able to joke about my miscarriage was a relief'", by Hadley Freeman, The Guardian, (9 Jun, 2016).


