Unsafe abortion

An unsafe abortion is the termination of a pregnancy by people lacking the necessary skills, or in an environment lacking minimal medical standards, or both. An unsafe abortion is a life-threatening procedure. It includes self-induced abortions, abortions in unhygienic conditions, and abortions performed by a medical practitioner who does not provide appropriate post-abortion attention. About 25 million unsafe abortions occur a year, of which most occur in the developing world.
Quotes
[edit]- Kawana Ashley, an unwed, pregnant teenager, had reasons for wanting to terminate her pregnancy. Unfortunately for Ashely, she was twenty-five weeks pregnant and could no longer obtain a legal abortion because the fetus was viable. So, on March 27, 1994, she obtained a gun and shot herself across the abdomen in an attempt to terminate her pregnancy. Ashely was rushed to the hospital and survived her self-inflicted gunshot wound. Her fetus, however, had been struck by the bullet and died fifteen days later. Ashley was prosecuted for manslaughter and third-degree murder, but the Florida Supreme Court held that a pregnant woman cannot be charged with these crimes for self-aborting. The court held that, under Florida law, Ashley could self-abort at any time during her pregnancy, even when the fetus was viable.
- Alford, Suzanne M. (2003). "Is Self-Abortion a Fundamental Right?". Duke Law Journal. 52 (5): 1011–29. JSTOR 1373127. PMID 12964572. Archived from the original on January 22, 2019. Retrieved January 21, 2007.
- Where therapeutic abortion has not been available, women have used a variety of ineffective but often-life endangering agents to try to end a pregnancy. Among them are concentrated soap solution used as a douche, the insertion of suppositories of potassium permanganate and the ingestion of quinine pills, or of castor oil or other strong laxatives. None of these is an effective abortifacient.
- Christine Ammer; JoAnn E. Manson (February 2009). “The Encyclopedia of Women's Health”. Infobase Publishing. pp.1-2
- Women who are considering abortion should remember that the earlier it is performed, the safer it is. Many of the facilities (clinics) and physicians performing abortions offer a limited range of services, so it is important to investigate what is available. Such research can be done through local health departments, women’s health centers and clinics, and local Planned Parenthood associations, which usually have a referral list for their locality. Factors to consider in choosing a physician or service include preferences as to general or local anesthesia (general anesthesia is advisable only in a hospital), private or clinic care, impatient or outpatient care, the type of procedure desired, the availability of emergency care should it be needed and aftercare should complications develop.
- Christine Ammer; JoAnn E. Manson (February 2009). “The Encyclopedia of Women's Health”. Infobase Publishing. p.7
- Since the passing of the groundbreaking Choice on Termination of Pregnancy Act in 1996 maternal mortality and morbidity related to unsafe abortion have been reduced by 91% and 50%, respectively, while recorded terminations of pregnancy (TOPs) increased by 67%.
TOPs at designated facilities rose steadily from 26 401 in 1997 (the year after the law was introduced) to 81 900 last year (67%).
These figures come from the national Department of Health and the Medical Research Council (Jewkes, et al.) as emphasis in the once hotly debated and much-ventilated topic shifts towards whether sufficient counselling is being offered to these women, 9.7% of whom are minors.
According to the latest Health Systems Trust data, the percentage of designated TOP facilities actually functioning rose from 31.5% in 2000 to 61.8% in 2003.
Izindaba enquiries showed the fault lines to have remained the same: ‘pro-lifers’ (such as Doctors for Life (DFL)) versus organisations like the Reproductive Rights Alliance (formed to promote the legislation) – arguing a shameful paucity versus a mostly pragmatic sufficiency of counselling.- Bateman C (December 2007). "Maternal mortalities 90% down as legal TOPs more than triple". South African Medical Journal = Suid-Afrikaanse Tydskrif vir Geneeskunde. 97 (12): 1238–1242. PMID 18264602. p.1238
- ‘Our view is that if more people can come together and help a province provide this service, it’s one way of cutting down on backstreet abortions and helping often desperate women.’
Theron said he was aware of complaints about the lack of counselling at over-stretched public clinics – which made such public/private TOP partnerships all the more valuable.
Marie Stopes clinics were ‘coping comfortably’ with the extra work and maintained public awareness by visiting midwives at state clinics and reminding them of the free referral facility wherever it existed.
Even where a public-private partnership did not exist, provincial TOP facilities sometimes referred patients to them. ‘Those that can afford to use us under 12 weeks get help immediately – we can go up to 20 weeks, after which we refer to a private gynae.’
He had come across ‘dilemmas’ of women who could not be helped timeously at state facilities. By the time they could be seen to, they were ‘too far advanced’, making termination illegal.
Trueman said one of the more worrying complaints among midwives involved the cavalier prescribing or dispensing of misoprostol (Cytotec) (a cervical ripening agent) by persons who had no relationship with any designated TOP facility. ‘These cases get treated as incomplete abortions in hospital and they end up going for a D and C – in most provinces you’ll find midwives very uptight about this,’ she added.
These women were often not afforded counselling to the same extent as they would be if they were helped at TOP facilities, she said. Professor Denise White, deputy chairperson of the South African Medical Association, advised GPs to refer patients to the appropriate facilities, adding that any doctors behaving as alleged would be putting themselves and their patients at ‘huge risk’.
‘We’re living in an enlightened era where legitimate resources are available. This is an ethical and medico-legal issue and we don’t want to hark back to the era of backstreet abortions.’
White said no substantive evidence had emerged that doctors were prescribing the ripening agents without providing referral or further support and it would be ‘very concerning if non-registered charlatans’ were behind the phenomenon, as suggested by Ruschebaum.- Bateman C (December 2007). "Maternal mortalities 90% down as legal TOPs more than triple". South African Medical Journal = Suid-Afrikaanse Tydskrif vir Geneeskunde. 97 (12): 1238–1242. PMID 18264602. pp.1240-1241
- Unsafe abortion and associated morbidity and mortality in women are completely avoidable. This paper reports on an analysis of the association between legal grounds for abortion in national laws and unsafe abortion, drawing on an unpublished study and using estimates of the incidence of and mortality from unsafe abortion using information from the sources used to estimate the incidence of unsafe abortion and associated mortality in 2000. Although legal grounds alone may not reflect the way in which the law is applied, nor the quality of services offered, a clear pattern was found in more than 160 countries indicating that where legislation allows abortion on broad indications, there is a lower incidence of unsafe abortion and much lower mortality from unsafe abortions, as compared to legislation that greatly restricts abortion. The data also show that most abortions become safe mainly or only where women's reasons for abortion, and the legal grounds for abortion coincide. This is a compelling public health argument for making abortion legal on the broadest possible grounds. A wide range of actions have formed part of national campaigns for safe, legal abortion over the past century, covering law reform, provision of safe services, ensuring quality of care, training for providers and information and support for women. Safe abortion is an essential health service for women, as essential for sexual and reproductive health as safe contraception, and safe pregnancy and delivery care. In spite of sometimes powerful opposition and terrible setbacks, the public health imperative is gaining ground in many parts of the globe.
- Berer M (November 2004). "National laws and unsafe abortion: the parameters of change". Reproductive Health Matters. 12 (24 Suppl): 1–8. doi:10.1016/S0968-8080(04)24024-1. PMID 15938152. S2CID 33795725.
- Twenty-five states have enacted Targeted Restrictions on Abortion Providers —or TRAP — laws imposing strict requirements on abortion clinics and providers that the Guttmacher Institute, a reproductive rights research group, says "go beyond what is necessary to ensure patients’ safety." Reproductive rights activists also call them "clinic shutdown laws," because they say the laws are often written with the intent of closing abortion clinics in the state.
- Business Insider, (February 10, 2017). "Here's how many abortion clinics are in each state"
- A TRAP law was at the heart of a major case decided by the Supreme Court in 2015, Whole Woman's Health v. Hellerstedt. The law in question required abortion clinics in Texas to meet strict standards, from the exact size of the examination rooms to admission privileges doctors had to secure for admitting patients to local hospitals.
In June, SCOTUS ruled in a 5-3 decision that the law "provides few, if any, health benefits for women, poses a substantial obstacle to women seeking abortions, and constitutes an 'undue burden' on their constitutional right to do so."
But similar laws are still on the books in half of the states in the country, and can cause clinics to close, forcing women who need abortions to travel farther in order to get the care they need. After Texas' law went into effect in 2013, the number of clinics providing abortions in the state dropped in half, from 41 to 22.- Business Insider, (February 10, 2017). "Here's how many abortion clinics are in each state"
- Death from illegal abortion was once common in the United States. In the 1940s, more than 1,0000 women died each year of complications from abortion. In 1972, 24 women died of complication of legal abortion and 39 died from known illegal abortions. In 2000, the last year for which complete data are available, there were 11 deaths from legally induced abortion, and no deaths from illegal abortion (abortion induced by a nonprofessional) in the entire United States. The American Medical Associations Council on Scientific affairs has reviewed the impact of legal abortion and attributes the decline in deaths during the country to the introduction of antibiotics to treat sepsis; the widespread use of effective contraception beginning in the 1960s, which reduced the number of unwanted pregnancies; and, more recently, the shift from illegal to legal abortion. The United States has a serious problem with teenage pregnancy. Without legal abortion, there would be almost twice as many teenage births each year.
- Sacheen Carr-Ellis, Nathalie Kapp; "10. Family Planning". In Berek, Jonathan S. (ed.). "Novak's Gynecology” (14 ed.). (2007) Lippincott Williams & Wilkins. pp.295-296
- It is the number of maternal injuries and deaths, not abortions, that is most affected by restrictive legal codes. Abortions performed outside the law have a higher rate of complications and deaths, the majority of which are entirely preventable. Worldwide, more than one third of the estimated 50 million annual abortions are illegal abortions, occurring mainly in the developing world. Researchers estimate that 70,000 to 200,000 women a year around the world die from illegal and unsafe abortions. Doing away with such purposeless human suffering has been one of the main motives behind the movement to liberalize abortion laws the world over.
At present almost two thirds of the world’s women live in countries where abortion may be legally obtained for a broad range of social, economic or personal reasons. When abortion is made legal, available and safe, women’s reproductive health improves. Abortion-related mortality is reduced by at least 25% and related illness by far more. Where abortions are safe and affordable, by far the largest percentage of women terminate their pregnancies within the first trimester.
When women can avoid births which are unwanted, mistimed, or too numerous, their children are more likely to survive and be healthy. The incidence of infanticide and child abandonment typically go down when abortion is legalized.
Even in countries where the abortion law seems “liberal”, it cannot be assumed that every woman has an equal chance of getting an early, safe abortion if she needs one. Lack of medical facilities or personnel, women’s low status in society, cultural taboos, restrictive regulations and financial roadblocks can effectively curtail access to legal abortion and contraception, especially for disadvantaged and young, unmarried women. Changes in laws, while necessary, are not themselves sufficient for widespread access to family planning and safe abortion services.- "Abortion Law, History & Religion". Childbirth By Choice Trust. Archived from the original on 12 January 2013. Retrieved 23 March 2008.
- The latest World Health Organization data estimate that the total number of unsafe abortions globally has increased to 21.6 million in 2008. There is increasing recognition by the international community of the importance of the contribution of unsafe abortion to maternal mortality. However, the barriers to delivery of safe abortion services are many. In 68 countries, home to 26% of the world's population, abortion is prohibited altogether or only permitted to save a woman's life. Even in countries with more liberal abortion legal frameworks, additional social, economic, and health systems barriers and the stigma surrounding abortion prevent adequate access to safe abortion services and postabortion care. While much has been achieved to reduce the barriers to comprehensive abortion care, much remains to be done. Only through the concerted action of public, private, and civil society partners can we ensure that women have access to services that are safe, affordable, confidential, and stigma free.
- Culwell, Kelly R.; Hurwitz, Manuelle (May 2013). "Addressing barriers to safe abortion". International Journal of Gynecology & Obstetrics. 121: S16–S19. doi:10.1016/j.ijgo.2013.02.003. PMID 23477700. S2CID 22430819.
- Unsafe abortion accounts for a significant proportion of maternal deaths, yet it is often forgotten in discussions around reducing maternal mortality. Prevention of unsafe abortion starts with prevention of unwanted pregnancies, most effectively through contraception. When unwanted pregnancies occur, provision of safe, legal abortion services can further prevent unsafe abortions. If complications arise from unsafe abortion, emergency treatment must be available.
- Culwell KR, Vekemans M, de Silva U, Hurwitz M (July 2010). "Critical gaps in universal access to reproductive health: Contraception and prevention of unsafe abortion". International Journal of Gynecology & Obstetrics. 110: S13–16. doi:10.1016/j.ijgo.2010.04.003. PMID 20451196. S2CID 40586023.
- Unsafe abortion is one of the most neglected public health challenges in the Middle East and North Africa (MENA) region, where an estimated one in four pregnancies are unintended—wanting to have a child later or wanting no more children. Many women with unintended pregnancies resort to clandestine abortions that are not safe. According to the World Health Organization (WHO), around 1.5 million abortions in MENA in 2003 were performed in unsanitary settings, by unskilled providers, or both. Complications from those abortions accounted for 11 percent of maternal deaths in the region.
- Dabash, Rasha; Roudi-Fahimi, Farzaneh (2008). "Abortion in the Middle East and North Africa" (PDF). Population Research Bureau. Archived (PDF) from the original on 6 October 2011. p.1
- The fact of the matter is that the distinction that the anti-choice movement seeks to make, between “life-saving” abortions and merely “health-saving” ones, is empirically impossible to determine: medical risks in pregnancy escalate quickly and unpredictably, meaning that a medical emergency can become life-or-death with little warning. It is unclear whether this fictional distinction is one the court will enshrine in law. But in another sense, the anti-choice movement has already won: the abortion debate now is being waged not on questions of women’s equality, dignity, and self-determination – these have already been sacrificed by the law as supposedly incompatible with the status of pregnancy.
What is at stake now – what was being debated in court on Wednesday – is how much women can be forced to suffer, how much danger they can be placed in. The anti-choice movement, and its allies on the bench, have shown once again that there is no amount that will satisfy them.- Moira Donegan, “The US supreme court heard one of the most sadistic, extreme anti-abortion cases yet”, The Guardian, (25 April, 2024)
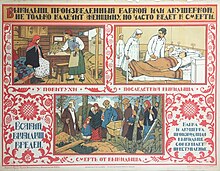
- In colonial times, surgical abortions were so dangerous, women almost never survived them. But many substances to bring about abortions were known. Depending on the amount used, these could accidentally kill both the mother and the fetus, kill only the fetus, or fail to work at all.
- Farrell, Courtney (2008). “Abortion Debate”. ABDO Publishing Company. Abortion From Past to Present, p.20
- Illegal abortion is responsible for up to half of maternal deaths and consumes a large proportion of health resources in many developing countries, particularly in Africa and Latin America. The legal situation of abortion in a country does not influence the abortion rate, but illegality is associated with a much greater risk of complications and death. To make abortion legal is not enough. Access to safe abortion strongly depends on the capacity and willingness of physicians and the health system to provide safe services, which sometimes are made available in spite of restrictive laws. The abortion rate will drop and the safety of the procedure will improve, parallel to the position women occupy in a given society, and to the level of recognition of their sexual and reproductive rights. The medical profession, and FIGO in particular, has a great role to play in implementing initiatives that will reduce the consequences of illegal abortion for women and society.
- A Faúndes, E Hardy; “Illegal abortion: consequences for women's health and the health care system”, Int J Gynaecol Obstet. 1997 Jul;58(1):77-83.
- Unsafe abortion is preventable, but it remains a major global health issue causing unnecessary threats to women’s health and burdens on the health system. Globally, an estimated 25 million abortions (45% of the total 55.7 million) that occur every year are unsafe, with most (97%; 24 million) occurring in low‐resource settings where countries that highly restrict abortion are concentrated. Unsafe abortion results in an estimated 47,000 maternal deaths a year, and an additional 6.9 million women are estimated to suffer morbidities from complications due to unsafe abortion. The World Health Organization (WHO) defines unsafe abortion as a procedure for terminating an unintended pregnancy carried out by either a person lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both. Since 2000, with the advent and ubiquitous access to medical abortion drugs, safe abortion has increased, and abortion‐related morbidity and mortality have improved.
- Gambir, Katherine; Kim, Caron; Necastro, Kelly Ann; Ganatra, Bela; Ngo, Thoai D. (9 March 2020). "Self-administered versus provider-administered medical abortion". The Cochrane Database of Systematic Reviews. 3: CD013181. doi:10.1002/14651858.CD013181.pub2. ISSN 1469-493X. PMC 7062143. PMID 32150279.
- In 1881 the Michigan Board of Health estimated one hundred thousand abortions a year in the United States, with just six thousand deaths, or a 6 percent mortality rate. There is some misunderstanding about abortion safety today because the campaign for legalized abortion has understandably emphasized the dangers of illegal abortion. In fact, illegal abortions in this country have an impressive safety record. The Kinsey investigators, for example, were impressed with the safety and skill of the abortion they surveyed. Studies of maternal mortality in the late 1920s and early 1930s found that 13-14 percent resulted from illegal abortion (meaning, of course, that 86-87 percent resulted from child-birth). Legal abortion had made that ratio even more uneven today in the United States, when eleven times more women die in childbirth than from abortions.
This does not mean that abortions were pleasant. They were painful and frightening, and anxiety was worse because they were “gotten in sin” and, often, in isolation. The physical risk was heightened by the illegality, just as it is today.- Gordon, Linda (2002). “The Moral Property of Women”. University of Illinois Press. ISBN 0-252-02764-7. “Ch.2 The Criminals” p.25
- When the medical establishment undertook a campaign against abortion in the second half of the nineteenth century, its very vehemence served as a further indication of the prevalence of illegal abortions. In 1857 the American Medical Association (AMA) initiated a formal investigation of the frequency of abortion. Seven years later the AMA offered a prize for the best popular antiabortion tract. Medical attacks on abortion grew in number and virulence until, by the 1870s, both professional and popular journals were virtually saturated with the issue. Physicians bemoaned the widespread lay acceptance of abortion before quickening; in order to break that sympathy, they adopted a new vocabulary that described abortion in terms designed to shock and repel, such as “antenatal infanticide.” Physicians attempted to frighten women away from abortion by emphasizing its dangers. Their common assertion that there was “no” safe abortion may have betrayed ignorance, but more likely it was an exaggeration justified by what they believed was a higher moral purpose. Yet occasionally even antiabortion doctors allowed the truth to slip out, revealing despite themselves why their campaign remained ineffective. It is such a simple and comparatively safe matter for a skillful and aseptic operator to interrupt an undesirable pregnancy at an early date,” wrote Dr. A. L. Benedict of Buffalo, New York, an opponent of abortion, “That the natural temptation is to comply with the request.
- Gordon, Linda (2002). “The Moral Property of Women”. University of Illinois Press. ISBN 0-252-02764-7. “Ch.2 The Criminals” p.30
- It is estimated that in 2000 27 million legal and 19 million illegal abortions were performed worldwide. Up to 95% of illegal abortions (unsafe abortions) were performed in developing countries and 99% of deaths from these abortions also occurred in those countries. Access to safe abortion is limited in many developing countries because of legal restrictions, administrative barriers to access legal abortion services, financial barriers and lack of adequately trained providers, In Latin America, rural women with limited financial resources disproportionately suffer from complications of illegal abortion.
- Grossman D (3 September 2004). "Medical methods for first trimester abortion: RHL commentary". Reproductive Health Library. Geneva: World Health Organization. Archived from the original on 28 October 2011. Retrieved 22 November 2011.
- Although abortion is legal in every state, it is not easily accessible everywhere. Anti-abortion activists and legislators have managed to drive some abortion clinics out of business, a strategy that effectively functions as a state-level ban in places with few abortion providers. Mississippi is a case in point; in 2012, the state nearly lost its only abortion clinic due to a law requiring abortion providers to be "certified obstetrician/gynecologists with privileges at local hospitals." At the time, just one doctor at Jackson Women's Health Organization had these privileges.
Seven years after Mississippi's sole abortion clinic fought to stay open, the fate of Missouri's only such clinic hung in the balance because of a licensing dispute. In early 2019, Missouri's health department failed to renew the clinic’s license, arguing that the facility was out of compliance. Planned Parenthood opposed this decision, but the clinic's future remained uncertain and tied up in the courts, as of fall 2019. In addition to Missouri and Mississippi, four other states—Kentucky, West Virginia, North Dakota, and South Dakota—have just one abortion clinic.
The reasons several states have just one abortion clinic stems from Targeted Regulation of Abortion Providers (TRAP) laws. This legislation limits abortion clinics through complex and medically unnecessary building requirements or by requiring providers to have admitting privileges at local hospitals—the case in Mississippi in 2012. Other laws, specifically those that require ultrasounds, waiting periods, or pre-abortion counseling, pressure women to reconsider ending their pregnancies.- Tom Head, “Is Abortion Legal in Every State?”, Thoughtco, (October 27, 2019)
- Until the late 19th century, abortion was legal in the United States before “quickening,” the point at which a woman could first feel movements of the fetus, typically around the fourth month of pregnancy.
Some of the early regulations related to abortion were enacted in the 1820s and 1830s and dealt with the sale of dangerous drugs that women used to induce abortions. Despite these regulations and the fact that the drugs sometimes proved fatal to women, they continued to be advertised and sold.- History.com Editors, "Roe v. Wade". HISTORY. (Updated: May 15, 2019 Original: Mar 27, 2018)
- While American women with the financial means could obtain abortions by traveling to other countries where the procedure was safe and legal, or pay a large fee to a U.S. doctor willing to secretly perform an abortion, those options were out of reach to McCorvey and many other women.
As a result, some women resorted to illegal, dangerous, “back-alley” abortions or self-induced abortions. In the 1950s and 1960s, the estimated number of illegal abortions in the United States ranged from 200,000 to 1.2 million per year, according to the Guttmacher Institute.- History.com Editors, "Roe v. Wade". HISTORY. (Updated: May 15, 2019 Original: Mar 27, 2018)
- Overall, there was a significant increase in the proportion of cases with no signs of infection on admission (from 79.5% to 90.1%) and a significant decrease in evidence of interference on evacuation (4.5% to 0.6%) between 1994 and 2000. Substantial age differentials were seen. Women over 30 were significantly less likely than those 21-30 years or under 21 to be low severity (65.5% vs 75.2% vs 76.4%, P= 0.0087) and more likely to have offensive products (16.3% vs 6.0% vs 6.4%, P= 0.01) than the younger women.
Conclusions: Legalisation of abortion had an immediate positive impact on morbidity, especially in younger women. This is an important change as teenagers had the highest morbidity in 1994. The trend is supported by evidence from the 1999-2001 Confidential Enquiry into Maternal Deaths, which further suggested that abortion mortality dropped by more than 90% since 1994.- Jewkes R, Rees H, Dickson K, Brown H, Levin J (March 2005). "The impact of age on the epidemiology of incomplete abortions in South Africa after legislative change". BJOG. 112 (3): 355–359. doi:10.1111/j.1471-0528.2004.00422.x. PMID 15713153. S2CID 41663939.
- Under the WHPA, prohibiting a state regulation requires nothing more than a “reasonable likelihood” that it might “indirectly” deter “some patients” from getting an abortion. Defending that regulation, however, requires “clear and convincing evidence” that the regulation “significantly advances the safety of abortion services” and that this goal “cannot be advanced by a less restrictive alternative measure or action.” How’s that for heads-the-pregnant-person-wins-tails-the baby-loses?
- Jipping, Thomas (February 28, 2022). "Women's Health Protection Act: Unconstitutional and More Radical Than Roe v. Wade". The Heritage Foundation. Archived
- Unsafe abortion has been identified as one of the most easily preventable causes of maternal ill-health and death, yet it continues to threaten the health and lives of women globally. This has led some commentators to declare that ‘ending the silent pandemic of unsafe abortion is an urgent public-health and human-rights imperative’ (Grimes et al 2006). In response to the issues and challenges raised by this situation, the WHO (2004, 2007b) has deemed ‘preventing unsafe abortion’ a strategic priority underpinned by the following two goals:
in circumstances where abortion is not against the law, to ensure that abortion is safe and accessible
in all cases, women should have access to quality services for the management of complications arising from abortion.- Johnstone, Megan-Jane (2009). “Bioethics a nursing perspective”. Confederation of Australian Critical Care Nurses Journal. 3 (5th ed.). Sydney, NSW: Churchill Livingstone/Elsevier. p.228. ISBN 978-0-7295-7873-8. PMID 2129925. Archived from the original on 6 September 2017.
- Although modern induced abortion is one off the safest medical procedures available, it is regulated like no other area of medicine in the USA. The procedure is currently subject to a multitude of federal and state laws and regulations. This situation was not always the case. From the country’s inception up through the first half of the 19th century, abortion prior to “quickening” was legal and largely unregulated in the USA.
- Bonnie Scott Jones, Jennifer Dalven, “Abortion law and policy in the USA” Ch.4 in Paul M, Lichtenberg ES Borgatta L Grimes DA Stubblefield P Creinin (eds) “Management of unintended and abnormal pregnancy: comprehensive abortion care”. (April 27, 2009) Oxford: Wiley-Blackwell.
- Nearly 8% of maternal deaths worldwide are abortion-related and 99.5% of these occurring in developing regions. There is strong evidence linking unsafe abortions with increased maternal morbidity and mortality and most abortion-related maternal deaths are due to unsafe and illegal abortions. Although the overall abortion rate has declined, the proportion of unsafe abortions is increasing, especially in developing regions. Unsafe abortions are most common in countries with restrictive abortion laws. This suggests that improving abortion law reform could reduce maternal mortality, however, we do not have a rigorous evidence-base on which to support this premise.
- Latt, Su Mon; Milner, Allison; Kavanagh, Anne (5 January 2019). "Abortion laws reform may reduce maternal mortality: an ecological study in 162 countries". BMC Women's Health. 19 (1): 1. doi:10.1186/s12905-018-0705-y. ISSN 1472-6874. PMC 6321671. PMID 30611257.
- On the 'health risks' of abortion....
*The Royal College of Obstetricians and Gynaecologists guideline, The Care of Women Requesting Induced Abortion, provides evidence based on systematic literature reviews to show that abortion cannot be considered a serious risk to women's physical or mental health.
*Claims by opponents of abortion that abortion leads to breast cancer, future infertility, or mental ill-health can be understood as a political strategy, not an objective evaluation of the likely effects of abortion for a woman's health.- Lee, Ellie; Ann Furedi (February 2002). "Abortion issues today – a position paper" (PDF). Legal Issues for Pro-Choice Opinion – Abortion Law in Practice. University of Kent, Canterbury, CT2 7NY, UK. pp.2-3 Archived from the original (PDF) on 26 September 2007. Retrieved 24 May 2007.
- Notwithstanding involvement on the part of Catholic and Protestant clergy and others, physicians were the leading force in the campaign to criminalize abortion in the USA. The American Medical Association (AMA), founded in 1847, argued that abortion was both immoral and dangerous, given the incompetence of many practitioners at that time. According to a number of scholars, the AMA’s drive against abortion formed part of a larger and ultimately successful strategy that sought to put “regular” or university-trained physicians in a position of professional dominance over the wide range of “irregular” clinicians who practiced freely during the first half of the 19th century.
What followed was a “century of criminalization” characterized by a widespread culture of illegal abortion provision. Thousands of women died or sustained serious injuries at the hands of the infamous “back alley butchers” of that period, and encountering these victims in hospital emergency rooms became a nearly universal experience for US medical residents. However, safe abortions were available to some women, performed by highly skilled laypersons and physicians with successful mainstream practices who were motivated primarily by the desperate situations of their patients. These “physicians of conscience” were instrumental in convincing their medical colleagues of the necessity to decriminalize abortion. By 1970, the AMA reversed its earlier stance and called for the legalization of abortion.- Paul, M; Lichtenberg, ES; Borgatta, L; Grimes, DA; Stubblefield, PG; Creinin, MD; Joffe, Carole (2009). "1. Abortion and medicine: A sociopolitical history" (PDF). Management of Unintended and Abnormal Pregnancy (1st ed.). Oxford: John Wiley & Sons. ISBN 978-1-4443-1293-5. OL 15895486W. Archived (PDF) from the original on 19 January 2012. p.2
- Abortion legislation is another issue of primary concern in promoting reproductive health. Globally there are around 33 million legal abortions performed annually. It is estimated that illegal abortions contribute further to make a total of between 40 and 60 million. This means that for every known pregnancy there are between 24 and 32 induced abortions. It was estimated that in 2000 unsafe abortion accounted for a death toll of 68,000. Based on the 2000 figures it is estimated that 19 million unsafe abortions take place every year and that 1 in 270 such abortions result in maternal death.
- Maclean, Gaynor (2005). "XI. Dimension, Dynamics and Diversity: A 3D Approach to Appraising Global Maternal and Neonatal Health Initiatives". In Balin, Randell E. (ed.). Trends in Midwifery Research. Nova Publishers. p. 299. ISBN 978-1-59454-477-4. Archived from the original on 15 March 2015.
- Unsafe abortion continues to be a major public health problem in many countries. A woman dies every eighth minute somewhere in a developing country due to complications arising from unsafe abortion. She was likely to have had little or no money to procure safe services, was young – perhaps in her teens – living in rural areas and had little social support to deal with her unplanned pregnancy. She might have been raped or she might have experienced an accidental pregnancy due to the failure of her contraceptive method she was using or the incorrect or inconsistent way she used it. She probably first attempted to self-induce the termination and after that failed, she turned to an unskilled, but relatively inexpensive, provider. This is a real life story of so many women in developing countries in spite of the major advancements in technologies and in public health.
- Halfdan Mahler, (25 September 2007); "Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (PDF). Preface, World Health Organization. (2007).
- One of the most easily preventable causes of maternal death and ill-health is unsafe abortion, which causes approximately 13% of all deaths and approximately 20% of the overall burden of maternal death and long-term sexual and reproductive ill-health.and reproductive ill-health.
- Halfdan Mahler, (25 September 2007); "Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (PDF). Preface, World Health Organization. (2007).
- Every year nearly 42 million women faced with an unplanned pregnancy decide to have an abortion, and about 20 million of them are forced to resort to unsafe abortion. These approximately 20 million women often self-induce abortions or obtain a clandestine and unsafe abortion carried out by untrained persons under poor hygienic conditions. Abortion induced by a skilled provider in situations where it is legal is one of the safest procedures in contemporary medical practice and the recourse to manual vacuum aspiration (MVA) and medical (non-surgical) abortion have reduced abortion-related complications to very low levels.
- Halfdan Mahler, (25 September 2007); "Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (PDF). Preface, World Health Organization. (2007).
- The interventions to prevent unsafe abortion include expanding access to modern contraceptive services, providing safe abortion to the full extent of the law, and tackling the legal and programmatic barriers to the access to safe abortion. An informed and objective discourse continues to be much needed for developing interventions to prevent unsafe abortion and its devastating consequences for the survival, health and well-being of women, families and societies. By providing an objective assessment of the incidence of unsafe abortion and its related mortality, this report goes a long way in raising awareness of this major, but often neglected, public health problem.
- Halfdan Mahler, (25 September 2007); "Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (PDF). Preface, World Health Organization. (2007).
- Two folk medical conditions, "delayed" (atrasada) and "suspended" (suspendida) menstruation, are described as perceived by poor Brazilian women in Northeast Brazil. Culturally prescribed methods to "regulate" these conditions and provoke menstrual bleeding are also described, including ingesting herbal remedies, patent drugs, and modern pharmaceuticals. The ingestion of such self-administered remedies is facilitated by the cognitive ambiguity, euphemisms, folklore, etc., which surround conception and gestation. The authors argue that the ethnomedical conditions of "delayed" and "suspended" menstruation and subsequent menstrual regulation are part of the "hidden reproductive transcript" of poor and powerless Brazilian women. Through popular culture, they voice their collective dissent to the official, public opinion about the illegality and immorality of induced abortion and the chronic lack of family planning services in Northeast Brazil. While many health professionals consider women's explanations of menstrual regulation as a "cover-up" for self-induced abortions, such popular justifications may represent either an unconscious or artful manipulation of hegemonic, anti-abortion ideology expressed in prudent, unobtrusive and veiled ways. The development of safer abortion alternatives should consider women's hidden reproductive transcripts.
- Nations MK, Misago C, Fonseca W, Correia LL, Campbell OM (June 1997). "Women's hidden transcripts about abortion in Brazil". Social Science & Medicine. 44 (12): 1833–1845. doi:10.1016/s0277-9536(96)00293-6. PMID 9194245.
- Reagan's discussion of "dying declarations" makes particularly chilling reading: because the words of the dying are legally admissible in court, women on their deathbeds were informed by police or doctors of their imminent demise and harassed until they admitted to their abortions and named the people connected with them—including, if the woman was unwed, the man responsible for the pregnancy, who could be arrested and even sent to prison. In 1902 the editors of the Journal of the American Medical Association endorsed the by then common policy of denying a woman suffering from abortion complications medical care until she "confessed"—a practice that, Reagan shows, kept women from seeking timely treatment, sometimes with fatal results. In the late 1920s some 15,000 women a year died from abortions.
- Katha Pollitt, "Abortion in American History", Atlantic Monthly. (May 1997).
- The American Medical Association endorsed legalized abortion in 1967. Medical professionals reported that each year they were treating thousands of women who had obtained illegal abortions and had been injured as a consequence. Believing that abortions were inevitable in American society, they argued that legalizing the practice would allow trained medical staffs to perform safe procedures in medical facilities.
- Claire E. Ramussen, “Abortion”; in Chapman, Roger. “Culture wars: an encyclopedia of issues, viewpoints, and voices", M.E. Sharpe. Inc, (2010) pp.1-2
- Since TRAP laws surfaced in 2010, more than 50 safe abortion clinics have closed.
- Rankin, Lauren, "The Seven Most Common Lies About Abortion", Rolling Stone, (February 26, 2014).
- Access to safe abortion services is an urgent need in the developing world as well, particularly in countries throughout Asia, Africa, and Latin America, where an estimated 68,000 deaths occur each year due to unsafe abortion procedures. Many more women (20 to 50% of those undergoing unsafe abortion) suffer from life-threatening complications. All too often those who survive are permanently scarred by these procedures that take place in hazardous and unsanitary conditions.
- Allan Rosenfield, “Introduction” In Paul M, Lichtenberg ES Borgatta L Grimes DA Stubblefield P Creinin (eds) “Management of unintended and abnormal pregnancy: comprehensive abortion care”. Oxford: Wiley-Blackwell. ISBN 978-1-4051-7696-5. p.35
- Unsafe abortions cause 50,000 to 100,000 deaths each year. In some countries complications of unsafe abortion cause the majority of maternal deaths, and in a few they are the leading cause of death for women of reproductive age. The World Health Organization estimates that as many as 20 million abortions each year are unsafe and that 10% to 50% of women who undergo unsafe abortion need medical care for complications. Also, many women need care after spontaneous abortion (miscarriage). In one country, for example, at 86 hospitals an estimated 28,000 women seek care for complications of unsafe or spontaneous abortion each month.
The five main causes of maternal mortality are hemorrhage, obstructed labor, infection, pregnancy-induced hypertension, and complications of unsafe abortion. Many countries are undertaking programs to reduce deaths from the other four causes, but few provide adequate emergency medical care that would reduce maternal deaths from abortion complications. Even fewer provide family planning services and counseling to women treated for abortion complications.- Salter, C.; Johnson, H.B.; Hengen, N. (1997). "Care for Postabortion Complications: Saving Women's Lives". Population Reports. Johns Hopkins School of Public Health. 25 (1). Archived from the original on 7 December 2009.
- Only a small proportion of deaths are estimated to result from abortion in eastern Asia (0•8%, 0•2–2•0), where access to abortion is generally less restricted. Latin America and the Caribbean, and sub-Saharan Africa have a higher proportion of deaths in this category than the global average; 9•9% (8•1–13•0) and 9•6% (5•1–17•2), respectively. Another direct cause, embolism, accounted for more deaths than its global average in southeastern Asia (12•1%, 3•2–33•4) and eastern Asia (11•5%, 1•6–40•6).
The proportion of deaths due to indirect causes was highest in southern Asia (29•3%, 12•2–55•1), followed by sub-Saharan Africa (28•6%, 19•9–40•3). Indirect causes also accounted for nearly a quarter of deaths in the developed regions. The overall proportion of HIV maternal deaths is highest in sub-Saharan Africa, 6•4% (4•6–8•8%). The appendix shows estimates for country-specific cause of death distributions.- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. (June 2014). "Global causes of maternal death: a WHO systematic analysis". The Lancet. Global Health. 2 (6): e323–e333. doi:10.1016/S2214-109X(14)70227-X. PMID 25103301.
- Background: Information on incidence of induced abortion is crucial for identifying policy and programmatic needs aimed at reducing unintended pregnancy. Because unsafe abortion is a cause of maternal morbidity and mortality, measures of its incidence are also important for monitoring progress towards Millennium Development Goal 5. We present new worldwide estimates of abortion rates and trends and discuss their implications for policies and programmes to reduce unintended pregnancy and unsafe abortion and to increase access to safe abortion.
Methods: The worldwide and regional incidences of safe abortions in 2003 were calculated by use of reports from official national reporting systems, nationally representative surveys, and published studies. Unsafe abortion rates in 2003 were estimated from hospital data, surveys, and other published studies. Demographic techniques were applied to estimate numbers of abortions and to calculate rates and ratios for 2003. UN estimates of female populations and livebirths were the source for denominators for rates and ratios, respectively. Regions are defined according to UN classifications. Trends in abortion rates and incidences between 1995 and 2003 are presented.
Findings: An estimated 42 million abortions were induced in 2003, compared with 46 million in 1995. The induced abortion rate in 2003 was 29 per 1000 women aged 15-44 years, down from 35 in 1995. Abortion rates were lowest in western Europe (12 per 1000 women). Rates were 17 per 1000 women in northern Europe, 18 per 1000 women in southern Europe, and 21 per 1000 women in northern America (USA and Canada). In 2003, 48% of all abortions worldwide were unsafe, and more than 97% of all unsafe abortions were in developing countries. There were 31 abortions for every 100 livebirths worldwide in 2003, and this ratio was highest in eastern Europe (105 for every 100 livebirths).
Interpretation: Overall abortion rates are similar in the developing and developed world, but unsafe abortion is concentrated in developing countries. Ensuring that the need for contraception is met and that all abortions are safe will reduce maternal mortality substantially and protect maternal health.- Sedgh G, Henshaw S, Singh S, Ahman E, Shah IH (October 2007). "Induced abortion: estimated rates and trends worldwide". Lancet. 370 (9595): 1338–1345. CiteSeerX 10.1.1.454.4197. doi:10.1016/S0140-6736(07)61575-X. PMID 17933648. S2CID 28458527.
- Results: Each year 42 million abortions are estimated to take place, 22 million safely and 20 million unsafely. Unsafe abortion accounts for 70,000 maternal deaths each year and causes a further 5 million women to suffer temporary or permanent disability. Maternal mortality ratios (number of maternal deaths per 100,000 live births) due to complications of unsafe abortion are higher in regions with restricted abortion laws than in regions with no or few restrictions on access to safe and legal abortion.
Conclusion: Legal restrictions on safe abortion do not reduce the incidence of abortion. A woman's likelihood to have an abortion is about the same whether she lives in a region where abortion is available on request or where it is highly restricted. While legal and safe abortions have declined recently, unsafe abortions show no decline in numbers and rates despite their being entirely preventable. Providing information and services for modern contraception is the primary prevention strategy to eliminate unplanned pregnancy. Providing safe abortion will prevent unsafe abortion. In all cases, women should have access to post-abortion care, including services for family planning. The Millennium Development Goal to improve maternal health is unlikely to be achieved without addressing unsafe abortion and associated mortality and morbidity.- Iqbal Shah, Elisabeth Ahman; “Unsafe abortion: global and regional incidence, trends, consequences, and challenges”, J Obstet Gynaecol Can. 2009 Dec;31(12):1149-58.
- Today, abortion practitioner in the United States are targeted and reviled by the radical right and isolated by their communities. Many wear bulletproof vests in public, and almost all have unlisted home telephone numbers. The need for such precautions is relatively recent. During the illegal era (from the mid-nineteenth century until 1973), abortion practitioners operated with varying degrees of secrecy, but they did not fear for their lives. In fact, a number of abortionists I the illegal era provided their services for years-twenty, thirty, forty years, and more-completely unimpeded by the law. In many communities, the local abortion practitioner’s name and address were well known, not only to women who might require the service but also to police and politicians, who generally regarded the presence of a good abortionist a public health asset. For decades after the American Medical Association worked with state legislatures in the nineteenth century to outlaw abortion, abortion prosecutions were rare relative to the number of abortions performed. In most communities an unwritten agreement prevailed between law enforcement and practitioners: no death, no prosecution.
But after World War II the old agreement was rather suddenly canceled, and practitioners-chiefly the female ones (presumed by law enforcement to be unskilled, untrained, and unprotected in comparison to their male counterparts, and therefore more likely to be convicted)-were arrested, convicted, and sent to jail in unprecedented numbers, even when there was no evidence of a botched abortion. Many of these practitioners were highly skilled and experienced, having performed twenty some abortions a day, year after year.- Solinger, Rickie (1998), "Introduction", in Solinger, Rickie (ed.), “Abortion Wars: A Half Century of Struggle, 1950–2000”, University of California Press', pp.17-18
- Prior to scientific understanding of germ theory and antisepsis, any surgical intervention was likely to be fatal.
- Clyde Spillenger, Jane E. Larson and Sylvia A. Law; "Brief of 281 American Historians as Amici Curiae Supporting Appellees", "The Public Historian", Vol. 12, No. 3 (Summer, 1990), University of California Press, supra note 6, at 68.
- Various methods of unsafe abortion have been reported. In the pre-penicillin era, instrumentation or introductions of fluid into the uterus caused fatalities. These methods still prevail, with women attempting instrumentation into the uterus per vagina and rarely, per abdomen. There are also a number of reported cases where quinine, misoprostol, over-the-counter medicines, livestock droppings, detergent and herbal medicines have been used as abortifacients. Unsafe abortion can lead to morbidity and mortality. Complications range from minor infections to death; the more common being bleeding, infection, uterine perforation and peritonitis.
- Thapa, S.R.; Rimal, D.; Preston, J. (2006). "Self induction of abortion with instrumentation". Australian Family Physician. 35 (9): 697–98. PMID 16969439. Archived from the original on 8 January 2009. p.697
- A lack of awareness of the associated complications and psychosocial state may be reasons why women choose unsafe methods of abortion. It is a difficult task to identify which women fall into such categories, however an effort should be made to avoid the implications of unsafe abortion at the primary health care setting where women approach for contraception and/or counselling on abortion. Therefore, the importance lies in educating and making women aware not only of the safe legal methods of termination of pregnancy, but also of the complications that could follow unsafe procedures.
- Thapa, S.R.; Rimal, D.; Preston, J. (2006). "Self induction of abortion with instrumentation". Australian Family Physician. 35 (9): 697–98. PMID 16969439. Archived from the original on 8 January 2009. p.697-698
- Benefits and potential impact Has the potential to prevent nearly all deaths (70,000) and disabilities (5 million) from unsafe abortion annually.
*Saves an estimated.
US$680 million in health-system costs for treating serious complications due to unsafe abortion.
US$6 billion to treat post abortion infertility from unsafe abortion.
US$930 million to society and individuals in lost income due to death or disability resulting from unsafe abortion.
* Allows women and families to address consequences of contraceptive method failure.
- UNICEF; UNFPA; WHO; World Bank (2010). "Packages of interventions: Family planning, safe abortion care, maternal, newborn and child health". Archived from the original on 9 November 2010. Retrieved 31 December 2010. p.7
- ”All Governments and relevant intergovernmental and non-governmental organizations are urged to strengthen their commitment to women’s health, to deal with the health impact of unsafe abortion as a major public health concern and to reduce the recourse to abortion through expanded and improved family planning services.”
- September, 1994 U.N. International Conference on Population and Development (ICPD) in Cairo
- The theory that abortion can cause harm to women's mental health has also been refuted by the National Academies of Science, Engineering and Medicine, and the American Psychological Association. But in determining that the medical associations had the right to sue based on what's known as third-party standing, Kacsmaryk also pointed to a 2011 meta-analysis by Priscilla Coleman that purported to show a link between abortion and mental health outcomes.
Dr. Ushma Upadhyay, a professor at the University of California, San Francisco, and an expert in abortion access and safety in the U.S., criticized Coleman's methodology and said she compared wanted and unwanted pregnancies without accounting for the reasons that may contribute to whether a patient wants to get pregnant.
"Her work doesn't account for differences between groups when she looks at people who have had abortions and people who haven't," Upadhyay said. "It's so important because she will attribute the differences in mental health status to the abortion when it's clear as day that the differences in mental health status are due to a variety of life circumstances between the groups."- Melissa Quinn quoting Ushma Upadhyay, ”ACLU warns Supreme Court that lower court abortion pill decisions relied on "patently unreliable witnesses"”. CBS News, updated on: January 30, 2024
"Quantifying the global burden of morbidity due to unsafe abortion: magnitude in hospital-based studies and methodological issues" (September 2012)
[edit]Adler Alma J, Filippi Veronique, Thomas Sara L, Ronsmans Carine (September 2012). "Quantifying the global burden of morbidity due to unsafe abortion: magnitude in hospital-based studies and methodological issues". International Journal of Gynaecology and Obstetrics. 118 (Suppl 2): S65–S77. doi:10.1016/S0020-7292(12)60003-4. PMID 22920625. S2CID 43126015.
- The global burden of complications from unsafe abortion is thought to be high, but difficult to measure. A systematic review was conducted to describe the prevalence and type of complications of abortion among women hospitalized for treatment of abortion complications in settings where abortion is generally considered unsafe. There were 43 hospital-based studies reporting on severity and type of complications of abortions, but definitions varied substantially. The proportion of women treated in facilities for severe complications ranged from a median of 1.6% (range, 0.1%-10.8%) for renal failure to 7.2% (range, 0.1%-43.9%) for severe trauma. Heterogeneity of study designs and definitions makes comparisons difficult. Therefore, it is recommended that standardized designs and definitions are used in future studies of abortion complications.
- Unsafe abortion is thought to be widespread at the global level, although the exact burden is unknown. The World Health Organization (WHO) defines unsafe abortion as “a procedure for terminating an unintended pregnancy either by individuals without the necessary skills or in an environment that does not conform to minimum medical standards, or both”. According to this definition, the word unsafe refers to the standard of medical care rather than to complications resulting from unsafe procedures. Standards of medical care in relation to abortion procedures have not been clearly defined, however, and distinguishing between safe and unsafe environments remains difficult.
Many studies have attempted to quantify the numbers of women presenting at hospitals with complications of abortion. Such studies suggest that in developing countries, 5 million women may be admitted to hospitals each year as a result of an unsafe abortion. Few studies have examined the nature or severity of abortion complications, however, and it is difficult to interpret the magnitude of or variation in this reported burden. Some investigators have developed a systematic definition of severity of complications due to unsafe abortions, and it has been applied in a few countries. This definition has been recommended as a standard for future studies of severity of complications; however, relatively few studies have so far used this definition, and it is unclear whether there is a consensus on its use.
The objective of the present study was to review the literature to examine how the severity of abortion complications is defined in regions of the world where abortion is generally considered to be unsafe, and to synthesize what is known about the prevalence of severe abortion complications in women treated in facilities in these regions. A systematic review was conducted to determine the types and frequencies of complications reported to be associated with abortion, and methodological strengths and weaknesses of the available evidence are discussed. - Results
The search identified 14 475 citations. After titles and abstracts were screened, the full text for 1069 articles was obtained (Fig. 1). Forty-two studies provided information on specific complications of abortion in regions where abortion is generally considered unsafe. An additional study was obtained from an outside source, giving a total of 43 studies. Three studies reported two different study populations in their results, and these are reported separately in the tables. - Discussion
A total of 43 hospital-based studies were identified describing postabortion complications in regions where abortion is generally considered unsafe. Very few studies provided sufficiently detailed criteria to define complications, and definitions were particularly poor for hemorrhage and infections.
"Abortion among adolescents in Africa: A review of practices, consequences, and control strategies" (October 2019)
[edit]Shallon Atuhaire (October 2019). "Abortion among adolescents in Africa: A review of practices, consequences, and control strategies" (PDF). The International Journal of Health Planning and Management. 34 (4): e1378–e1386. doi:10.1002/hpm.2842. PMID 31290183. S2CID 195871358. Archived from the original (PDF) on 2022-05-30.
- Background: Developing countries register 98% of unsafe abortion annually, 41% of which occur among women aged between 15 and 25 years. Additionally, 70% of hospitalizations due to unsafe abortion are among girls below 20 years of age.
Purpose: This study unveils abortion practices in Africa, its consequences, and control strategies among adolescents.- p.1
- Findings: These studies indicated that abortion is a neglected problem in health care in developing countries, and yet decreasingly safe abortion practices dominate those settings. Adolescents who have unintended pregnancies may resort to unsafe abortion practices due to socio-economic factors and the cultural implications of being pregnant before marriage and the legal status of abortion. Adolescents clandestinely use self-prescribed drugs or beverages, insert sharps in the genitals, and most often consult traditional service providers. Abortion results in morbidities such as sepsis, severe anaemia, disabilities, and, in some instances, infertility and death. Such events can be controlled by the widening availability of and accessibility to contraceptives among adolescents, advocacy, and comprehensive sexuality education and counselling.
Conclusion: Adolescents are more likely to use clandestine methods of abortion whose consequences are devastating, lifelong, or even fatal. Awareness and utilization of youth-friendly services would minimize the problem.- pp.1-2
- Approximately 56 million women of reproductive age undergo induced abortion annually, and of those, 22 to 25 million are unsafe2, contributing to 13% of maternal mortality cases worldwide. Developing countries register 98% of unsafe abortions annually, 41% of which occur among women aged between 15 and 25 years, and the highest ranking regions are Africa and Latin America.6 In Nigeria, over one-thirds of adolescents procure abortions, in Ghana, abortion is more prevalent among women ranging from 20 to 24 years, while this prevalence level is seen among women aged 20 to 29 years in other African countries. However, in Asia and Europe, women older than those in African countries undergo abortions.7 In Africa, an increasing rate of early sexual initiation and sexual coercion has been reported.8,9 More than one in three adolescents or young adults in Uganda between 15 and 24 years of age who are not married and who have never been married have had sexual contact. Another study conducted in Uganda indicated that 46% of adolescents had ever had sex, and 80% were not married. Because pregnancy carries different socio-cultural implications for unmarried adolescents than married women generally, those who unintentionally become pregnant may resort to unsafe methods of inducing abortion. Adolescents generally suffer a greater impact because they are vulnerable, have inadequate sexual and reproductive health information, and are unable to make firm choices. As such, a study by the International Planned Parenthood Federation (IPPF)11 noted that 70% of hospitalizations due to unsafe abortion complications were among women under 20 years of age. This finding makes this study worthwhile for the sake of documenting adolescent abortion practices, their consequences, and control strategies to inform stakeholders about the prevailing situation and to provide a basis for the necessary steps to improve adolescent health.
- p.2
- Abortion is generally defined as the expulsion of the conceptus before 28 weeks of gestation or before it weighs 500 g. Induced abortion could be safe or unsafe depending on the procedure taken, the environment in which it is carried out and the service provider. Therefore, safe abortion is one that is carried out by a trained provider following WHO recommended methods suitable for the gestational age. Unsafe abortion, on the other hand, is often carried out to terminate unintended or unwanted pregnancies by unskilled individuals and in an environment that does not meet minimum medical standards. Unsafe abortion is categorized by WHO into less safe and least safe. It is less safe when performed using old-fashioned means such as sharp curettage methods, even if by trained personnel, and/or if the individual performing the abortion has limited information regarding the methods and limited access to a skilled medical officer if required. It is least safe when it involves the ingestion of caustic substances, the use of harmful traditional inventions or the insertion of foreign bodies by untrained individuals.
- p.2
- Legal and safe abortion is 14 times safer than childbirth; however, until now, only three African countries have no restrictions regarding abortion, while 41 countries allow abortion to save the mother's life and maintain her physical and mental health, as well as for socio-economic aids. The law also permits induced safe abortion when the foetus is impaired or when the pregnancy was caused by defilement, rape, or incest; however, abortion is completely illegal in 10 African countries
- pp.2-3
- Abortions induced by oneself or by traditional healers, result in complications, with infections in 81.8% of women and haemorrhage in 68.2% of women, and in some instances, the process results in incomplete abortion. There are higher odds of such complications among unmarried adolescents and non-adolescents than among married women in both categories. Adolescents, especially students, are aware of safe abortion services but may not use them due to costs and associated stigma. Women who boldly seek safe abortion are highly stigmatized, as are the clinicians offering it. In fact, any discussion about the topic in developing countries is disrupted owing to its legal status, religious and moral values. Surprisingly, even health workers abuse, mistreat and stigmatize women who seek post-abortion care. Therefore, it is still a neglected problem in health care with inadequate information, and yet least safe and less safe abortion practices dominate these settings.
Mothers who unintentionally become pregnant opt for unsafe abortions due to the insufficiency and inaccessibility of safe abortion services, restrictive laws, high costs, and diligent objections by health care providers who observe the professional ethic of do not harm and due to insufficient knowledge of eligibility for safe abortion care. Nonetheless, in Asia and Europe, older women procure abortion mainly to limit or space births. Adolescents from African countries may particularly pursue abortions because of probable consequences such as stigmatization. It is often procured through clandestine measures and in unhygienic hidden places, offered by untrained practitioners. These abortions are generally unsafe, accounting for 21% of the maternal deaths that occur annually, making it an issue of public health importance in the region. Unveiling abortion practices, its consequences, and control strategies among adolescents is of great significance to policymakers, programme planners, and advocates. If the information provided is well utilized, it could lessen the incidence of unintended pregnancies, unsafe abortions, and maternal and child mortality and morbidity, thus leading to a general increase in the number of healthy women.- p.3
- Africa has the highest rates of both intended and unintended pregnancies, standing at 136 and 86 per 1000 women of reproductive age, respectively. Central and East Africa registered the highest number of unintended pregnancies in 2010. Women who have unplanned pregnancies may opt for an abortion. In fact, one of every five of these women opts for abortion. In 2018, the Southern African region registered the highest abortion rate at 24%, followed by Northern Africa, Eastern Africa, Central Africa, and Western Africa at 23%, 14%, 13%, and 12%, respectively. However, in all regions, adolescents who are sexually active are more vulnerable than women older than 20 years of age with respect to their experiences and needs for and access to safe abortion care. First, they have a higher risk of unintended pregnancy and are unable to recognize it early compared to older women. Second, they are most likely to delay seeking an abortion for socio-economic and cultural reasons5 and, in some instances, due to policy-related and religious factors.
- p.3
- Abortion is generally more prevalent among women in urban centres globally than those in rural areas. However, rural residents in all age groups are more likely to use traditional methods than are urban residents. Unsafe abortions are also common among poorer, younger, and unmarried women with low socio-economic status than those who are married and/or well-off. Although adolescents undergo a substantial fraction of abortions, they are most frequently performed among women aged 20 to 29 years. Nonetheless, women below 20 years constitute more of those hospitalized for complications. A study conducted by Rasch and Kipingili in rural Tanzania also indicated that women who had an unsafe induced abortion were single, primigravida, and younger than 24 years of age. Women who procure unsafe abortions often use clandestine methods aided by unskilled attendants who may be a friend, a close relative or a traditional service provider. A study performed in Cote d'Ivoire in 2017 among high school students indicated that 70% of them first used a self-prescription, and in case it failed, 56.4% proceeded to use traditional service providers and whenever self-prescription and traditional methods were unsuccessful, approximately 85.7% of them consulted skilled health care providers as the last option. The students cited over-the-counter drugs, herbs, roots, beverages, and in some instances, the insertion of sharps in their genital tract as commonly used procedures. The use of pharmaceutical drugs, catheters, and roots has been cited by several other studies.
Some girls use battery acid, crushed bottles, pain medication, sedatives, anaesthesia, antibiotics, chlorine, white quinine, cassava-cyanide, aloe vera, castor oil, ashes, ground tobacco, saltwater, sugar solutions, washing powder/soap, and methylated spirits, which are very unsafe.
According to Varga, the commonly used methods of abortion among adolescents in South Africa are backstreet measures, which is attributable to women's inadequate knowledge of their legal status and eligibility for a safe abortion and a complex decision-making process. Another study on abortion among adolescents in developing countries states the same factors. Additional factors include gender inequality, an unmet need for contraceptive use, sexual education, high cost, and restrictive abortion laws.7,24 The issue of stigma is a serious issue, as highlighted by many other studies.- p.4
- Almost all ill health and mortality following unsafe abortion is preventable, and adolescents who are mostly in secondary schools are aware of illegal abortion practices and their consequences, which range from physical, psycho-social to economic in nature. The consequences are borne not only by women who acquire unsafe abortion but also by their families and the health care system. Both adolescents and non-adolescents suffer the consequences of abortion, but the impact is greater among adolescents.
Adolescents present with morbidities such as haemorrhage, severe anaemia, trauma, foreign body, sepsis, or mortality. These are frequently associated with the procedure used, for instance, women who use herbs to induce abortion are less likely to present with trauma, foreign body, or sepsis than are women who use surgical abortion, roots, or catheters. Similarly, women who use herbs are less likely to obtain blood transfusions than those who use any other method.
Haemorrhage is primarily the reason for admission among women who are having or have had an unsafe abortion. In a study by Ouattara et al, among 111 women who had an unsafe abortion, 75% suffered severe haemorrhage, 11% suffered endometritis, 5% suffered anaemia, and 5% suffered hepatonephritis, while six women died. Others may suffer from infection and infertility. Other effects are lifelong and devastating, such as psychosocial trauma, permanent disability, and infertility, a condition that upends their lives entirely.- p.5
- As many as 41 African countries have liberalized abortion laws, and three countries have legalized abortion entirely. Still much action is desired to ensure safe abortion and to address the impact of unsafe abortion. There is an urgent need for alternatives to abortion through expanded and enhanced family planning services, and if unintended pregnancy has already occurred for a woman who qualifies for safe legal abortion, then safety should be guaranteed. Additionally, the research agenda needs to be defined and advocacy strategies identified to curb the incidence of unsafe abortion (Table).
- p.5
- Most abortions follow unintended pregnancies, and adolescents are more vulnerable mainly due to socio-economic and cultural connotations, in addition to the harsh social stigma adolescents suffer in cases of premarital pregnancy. Therefore, societal norms, economic and legal obstacles have a profound influence on women's decision to have an abortion, especially unsafe abortion.6 The role of partners in influencing the decision to terminate pregnancy cannot be underrated in addition to whether he supplies funds for an abortion. When partners are supportive, women stand a better chance of retaining pregnancy, and if they should abort, the chance of having a safe abortion is significantly improved. Abortion practices differ by geographical region and range from traditional to modern methods, with rural teenagers more involved in the use of the former than urban-dwelling teenagers. However, modern methods are self-prescribed and are procured over the counter. Herbs and roots are commonly used to induce abortion in 42% of rural and 54% of urban women.30 Nonetheless, the use of roots is more associated with complications than herbs.
- p.5
- Unsafe backstreet methods include clandestine, self-prescribed pharmaceuticals, battery acid, crushed bottles, pain medication, sedatives, anaesthesia, antibiotics, chlorine, white Quinine, roots (cassava- cyanide), aloevera, castor oil, ashes, ground tobacco, salt water & sugar solutions, parsley oil, laxative, brandy, hot pepper salt, physical removal (with cassava root), chilli, or pawpaw, physical charms, boiled beer, tea, fanta, coca cola, washing powder/soap, and methylated spirit, physical exercises, inserting objects in the vagina, receiving a heavy massage, receiving an injection, taking oxytocin, inserting a catheter, taking a tablet, taking home remedies, an herbal concoction, or an herbal enema.
Safe methods include dilation and curettage (D&C), manual vacuum aspiration (MVA), and taking Cytotec.- Table 1, p.6
- Following unsafe abortion, 68 000 women die each year globally, while 5.3 million suffer disabilities that may be temporary or permanent6 and that are more common among women beyond 12 weeks of gestation. The public health burden of abortion remains the highest in developing countries with restrictive laws on abortion that compel women to resort to unsafe abortion, leading to injuries and, in some instances, maternal mortality.
The consequences are not only faced by women and their families but also by service providers. Physicians in countries where abortion is restricted may be surrounded by compromising terms and eventually suffer formidable penalties.- p.6
- Control strategies to abortion should strive to prevent unintended pregnancies, unsafe abortions, and related complications. By all means, unintended pregnancies must be prevented, and if they occur, measures should be taken to prevent victims from procuring an unsafe abortion.
These goals can be achieved by providing sexuality education, increasing access to contraception, meeting the family planning needs of individuals, offering and increasing access to safe legal induced abortion, and providing timely care for complications. These actions should be taken across various age groups, although special focus should be afforded to those below 25 years of age, given their greater vulnerability. There is also a need to create awareness of the risks associated with unplanned pregnancies and induced abortions mostly by unskilled providers. Understanding the factors behind the persistence of unsafe abortion mostly in developing countries and finding sustainable solutions are equally vital. Women willing to share their stories concerning unwanted or unplanned pregnancies and abortion should be given forums and be protected to facilitate their emotional healing and to enable others to learn from their stories.- pp.6-7
- Although adolescents and non-adolescents alike suffer similar abortion complications, adolescent-specific reproductive health policies, and particularly their implementation, are critically desired. Targets should be both in-school and out-of-school adolescents. Additionally, policies concerning the respect and protection of women and other vulnerable groups need to be implemented. Adolescents themselves report the need for adequate information concerning reproductive health issues because in most cases, they are provided with information that is too superficial to help them when confronted with sexual and reproductive health challenges. For example, they have information regarding condom use29 but do not know how to use them correctly and consistently. Adolescents and young adults need varying levels of protection and safety to aid them in making autonomous decisions and to be able to learn and grow. In the case of pregnancy, they need sufficient information, counselling, parental involvement, and contraceptive options.
Additionally, identifying key areas of research and advocacy are equally important to control strategies.- p.7
- In conclusion, adolescents are mostly likely to use clandestine methods of abortion, the consequences of which are devastating, lifelong, or even fatal. Awareness and the effective utilization of adolescent- and youth-friendly services would minimize the problem. Social and emotional support in the event of unintended pregnancy is necessary. Awareness of who qualifies for a legal safe abortion and where it can be accessed is still low; hence, it should be included in health education if positive adolescent health outcomes should be realized.
- p.7
"Making abortions safe: a matter of good public health policy and practice" (2000)
[edit]Berer M (2000). "Making abortions safe: a matter of good public health policy and practice". Bulletin of the World Health Organization. 78 (5): 580–592. PMC 2560758. PMID 10859852.
- Globally, abortion mortality accounts for at least 13% of all maternal mortality. Unsafe abortion procedures, untrained abortion providers, restrictive abortion laws and high mortality and morbidity from abortion tend to occur together. Preventing mortality and morbidity from abortion in countries where these remain high is a matter of good public health policy and medical practice, and constitutes an important part of safe motherhood initiatives. This article examines the changes in policy and health service provision required to make abortions safe. It is based on a wide-ranging review of published and unpublished sources. In order to be effective, public health measures must take into account the reasons why women have abortions, the kind of abortion services required and at what stages of pregnancy, the types of abortion service providers needed, and training, cost and counselling issues. The transition from unsafe to safe abortions demands the following: changes at national policy level; abortion training for service providers and the provision of services at the appropriate primary level health service delivery points; and ensuring that women access these services instead of those of untrained providers. Public awareness that abortion services are available is a crucial element of this transition, particularly among adolescent and single women, who tend to have less access to reproductive health services generally.
- p.580
- WHO estimates that about 25% of all pregnancies worldwide end in an induced abortion, approximately 50 million each year. Of these abortions, 20 million are being performed under dangerous conditions, either by untrained providers or using unsafe procedures, or both. Deaths as a result of unsafe abortions in developing countries are estimated at 80 000 annually, i.e. 400 deaths per 100 000 abortions. This figure hides substantial regional variation, however, with unsafe abortions in Africa being at least 700 times more likely to lead to death than safe abortions in developed countries. Although over the past 10 years there have been improvements in the safety of the abortion procedures used and access to treatment for complications for some women in developing countries, the number of women requiring treatment for serious complications of unsafe abortion remains very high and many women never receive care at all.
Unsafe abortion procedures, untrained abortion providers, restrictive abortion laws and high mortality and morbidity from abortion tend to occur in one and the same countries. This article outlines ways in which good public health policy and good quality medical practice can make abortions safe. It is based on a review of published and unpublished sources identified in MEDLINE and POPLINE searched, as well as articles in a range of journals, newsletters, books and other publications in the field.- p.580
- A range of positive steps has been taken to reduce deaths and morbidity from abortion in a growing number of countries over the past 15 years. Since 1980, abortion laws have been liberalized in some form in Albania, Algeria, Barbados, Belgium, Botswana, Bulgaria, Burkina Faso, Cambodia, Canada, China (Province of Taiwan), Czechoslovakia, Spain, Ghana, Greece, Guyana, Hungary, Indonesia, Malaysia, Mongolia, Pakistan, Romania, South Africa, Spain, and Turkey. In other countries there have been attempts to change highly restrictive abortion laws and/or major national debates on abortion. In Brazil, for example, Congress considered 46 bills on abortion between 1946 and 1995 ; 13 of 16 bills over the period 1991±95 were favourable towards making abortion legal under some circumstances.
Even in the absence of legal change, it has become easier for women to obtain treatment for abortion complications in large hospitals, at least in urban areas. The high cost and poor quality of care available in many developing country public hospitals is also being addressed. Manual vacuum aspiration techniques are finally beginning to replace dilatation and curettage as the standard of care for incomplete abortion; which in itself reduces complications. Furthermore, there are more abortion providers who have received some training and have greater awareness of safer procedures and practices so that, for example, in Bangladesh there are fewer serious complications and deaths than there were 10 years ago.
In some countries, women themselves are starting to use safer methods for self-induced abortions, in particular, intravaginal application of the prostaglandin misoprostol, resulting in fewer complications and shorter hospital stays. This has been well documented in Brazil and is thought to be common elsewhere in the region. Such changes have succeeded in reducing at least some of the more appalling examples of morbidity and mortality arising from the insertion of sticks, roots and sharp instruments into the uterus.- p.581
- Making abortion legal is an essential prerequisite to making it safe. In this respect, changing the law does matter and assertions to the contrary are ill conceived and unsupported in practice. Although, in many countries, trends towards safer abortion have often occurred prior to or in the absence of changes in the law, legal changes need to take place if safety is to be sustained for all women.
Safety is not only a question of safe medical procedures being used by individual providers. It is also about removing the risk of exposure and the fear of imprisonment and other punitive measures for both women and providers, even where illegal abortion is tolerated. Health professionals providing safe but clandestine abortion in urban Latin America have described a lack of medical support, the need for secrecy, as well as threats of violence, extortion and prosecution. In Bolivia and Chile, the interrogation of women seeking treatment for abortion complications in public hospitals is or has been routine. In Nigeria, illegal abortion carries a sentence of up to 14 years imprisonment except where the life of the woman is at risk. Moreover, although illegal abortion has been tolerated in a number of countries over the past 10 years, arrests have been made without warning.
Safety is also about making sure that abortions will not be carried out by clandestine and unskilled providers who operate in situations that endanger women's lives, even if they have the best of intentions. A woman has little or no recourse when abortion is illegal, even if she is seriously injured, badly treated, refused pain relief, sent home in a poor condition, charged a large amount of money, or suffers any other form of negligence or malpractice. Continuing pregnancies following attempts at self-induced abortion are not uncommon and women may need follow-up care for other reasons, but they may be impossible to contact because they have given a false address.- p.582
- Both the content of the law and the policy that defines how the law will be implemented matter. It is often in the details that service delivery is facilitated or blocked. Zambia and India are often erroneously cited as examples of why changing the law does not matter, as both are classified as countries where abortion is legal but where abortion mortality remains high. However, the term legal does not necessarily mean that the law is appropriate for the circumstances in which it must be implemented. Abortion mortality remains high in Zambia and India because of obstacles to putting the law into practice, including provider unwillingness, lack of training for providers, failure to authorize providers and facilities, and a lack of resources for and commitment to delivering good services at the primary care level. In Zambia, the law requires several doctors' signatures for an abortion when in most places there are few or no doctors and lack of resources is an important issue. One study found that legal abortion services were inaccessible or unacceptable to schoolgirls, among whom more than half of abortion deaths were occurring, because providers did not respect confidentiality. The young women were apparently required to reveal who made them pregnant, which they were unwilling to do, and feared being expelled from school. Abortion was legalized in India for broad social and medical reasons in 1972, when experience in providing safe abortions was more limited. Today, many of the annual 6.7 million abortions performed in the country are still carried out by untrained providers in unapproved sites. Approved abortion clinics are concentrated in the cities, and are unevenly distributed. A total of 32% of approved primary health centres in four states have never offered abortions since they lack trained providers and functioning equipment. In one state, acceptance of sterilization following abortion has been required, although this is not stipulated in law. Furthermore, women are often expected to attend without an appointment, and if the clinic is too busy they are told to come back another day, again without an appointment. Women may also be charged for an abortion according to the numbers of weeks of pregnancy, although the procedure is supposed to be free (T.K. Sundari Ravindran, personal communication, 1997). Thus, women may be discouraged or prevented from seeking bona fide services in ways never intended by the law.
- p.582
- To make abortion safe, restrictive laws need to be annulled, amended or replaced; traditional and, in some cases, religious laws may also require attention when legal change is being contemplated. Countries have taken three main routes to this end: liberalizing the existing law within the penal or criminal code; partially or fully legalizing abortion through a positive law or a court ruling; and decriminalizing abortion by taking it out of the law altogether. These changes have already occurred in almost all industrialized countries and are happening in a growing number of developing countries as well.
- pp.582-583
- The earlier in pregnancy that an abortion takes place, the safer it is for the woman's health and the less complicated for the provider. Hence, on public health grounds, regulations that tend to delay the procedure should be avoided. Such regulations include putting the abortion decision into the hands of people other than the woman herself, weighting conscientious objection clauses in favour of providers who want to opt out, or requiring a waiting period between obtaining permission for and having an abortion.
- p.583
- In countries where safe abortions are the norm, more than 90% of women have abortions in the first trimester of pregnancy. Western European laws commonly allow abortion upon the woman's request in the first trimester of pregnancy, while in the second trimester the permission of one or more doctors or a designated medical committee is required and/or more restricted grounds pertain. Laws of this type were passed some 20±30 years ago, and along with good service delivery, have reduced abortion mortality and morbidity to a rarity. One of the unintended consequences, however, is the creation of a minority of excluded women who have difficulty obtaining second trimester abortions and may have to travel to another country for this. Moreover, fewer clinics offer second trimester procedures. Thus, obstacles and delays in obtaining abortions after 12 weeks often contribute to making the procedure later and more complicated than necessary.
Women who need abortions after the first trimester of pregnancy include the following: those who are not aware that they are pregnant or who deny the pregnancy until it begins to show (most often young women); those who think they are too old to get pregnant; those whose personal circumstances change dramatically during the pregnancy (e.g. the husband leaves or dies); those who develop medical reasons for abortion; and those who find out that the fetus is seriously damaged. Where abortion has previously been illegal and clandestine, women needing second trimester abortions also include those who are unaware that the law has changed, those living far from facilities, those who need more time to find out where to obtain a safe abortion, and those who have attempted self-induced abortion unsuccessfully and who have a continuing pregnancy.- pp.583-584
- Where abortion is clandestine and unsafe, women (or their partners or families) are buying drugs and other means of self-induced abortion and/or paying clandestine providers, while public health services and women are paying for the treatment of abortion complications, often in tertiary level hospitals, where costs are highest. Costs (economic and social) incurred for unsafe abortions include not only acute care, however, but also the longer-term complications of damage to reproductive organs, pelvic inflammatory disease, and secondary infertility. Moreover, the need for blood transfusions to deal with haemorrhage and other complications of unsafe abortion should be considered against a background of increasing HIV seroprevalence in many developing countries. Costs for families, especially for a woman's existing children, also include those that result from a maternal death.
Unsafe abortion situations are characterized by a lack of equity in cost, safety and quality of care. In some Bolivian hospitals, women who present with signs of induced abortion are charged higher fees for treatment of complications than women who appear to have miscarried, which contributes to delays in obtaining care. In Egypt, as elsewhere, the price for a clandestine abortion increases in proportion to the level of safety provided.
Most authors agree that treating abortion complications in sub-Saharan Africa consumes a disproportionate amount of hospital resources, while in Bangladesh, up to 50% of hospital gynaecology beds are reported to be taken up with abortion complications. Women tend to wait until complications become severe before seeking help, increasing both the cost and complexity of treatment. Furthermore, women attending untrained providers have been found to make more visits for care and spend more overall than women attending trained providers in the first place. A study in United Republic of Tanzania estimated that the cost per day of treating abortion complications, including the costs of drugs, meals, staying costs and surgical procedures, was more than seven times the Ministry of Health's annual per capita budget. Only 3 of 455 women were treated and discharged on the same day; 25% needed one day, almost 50% needed 2 days and the remainder needed 3±5 days to recover. In Guyana, about 25% of the blood available at the main public hospital was used to treat abortion complications before the law was changed. Covering the cost of safe abortions in public health services is therefore not about incurring entirely new costs, but about shifting expenditure away from complicated cases in tertiary level hospitals to safe, simple procedures that can be provided in primary clinics. Women may or may not be charged a fee at the point of service, but safety should mean affordability for the poorest of women as well as for those who can pay, with one high standard of care for all.- p.585
- Along with safe methods and trained providers, programmes require locally accessible services in both rural and urban areas. In Zambia, gynaecologists were found to be a major obstacle to the setting up of safe abortion services. The ambivalence of doctors was also found to have hampered the implementation of a revised abortion law in Indonesia. In Bangladesh and India, untrained providers, who are often more easily accessible in rural areas, have never actively been stopped from practising. In South Africa, in contrast, as cases have arisen where unlicensed providers have continued to offer services despite the changed legal status of abortion, criminal charges have been pressed against them. A nationally coordinated programme aims to ensure that throughout the country, primary and secondary care facilities are prepared to perform abortions. All nine provinces in South Africa have developed provincial plans, each in collaboration with a medical school or a tertiary training hospital. A national advisory group has been set up to coordinate and monitor implementation of the new law, including health service managers, representatives from medical schools, academics and specialists, the nursing council, researchers and the nongovernmental sector. This group plans to meet every 4±6 months and make recommendations to government on relevant issues.
- p.586
- Bringing abortion services out into the open is a precondition for ensuring quality of care, accessibility, availability and affordability, especially for the poorest women. This encourages health professionals to provide a defensible service. In Guyana, for example, although most clandestine abortion providers were medical professionals before the law was changed in 1995, septic abortion was the third highest cause (19%) of hospital admissions. After the law changed, this same group of providers organized themselves and voluntarily began to give prophylactic antibiotics. Admissions to the main public hospital for septic and incomplete abortions fell by 41% within 6 months of this decision.
Public visibility in service provision means that women will have a more open choice of providers and can take action if their rights are violated or care is substandard; legalization also ensures that providers who attempt to sexually molest clients, anecdotally a not uncommon problem for women seeking clandestine abortions, can be prosecuted. Sympathetic treatment on the part of service providers is important. Uncaring treatment and verbal abuse on the part of health care staff towards women seeking treatment for complications of clandestine abortion has been well documented in Latin America. Indeed, lack of sympathy is a problem in many countries, even those with safe abortion services such as Great Britain and the USA, where abortion has been legal for 30 years. South Africa is trying to confront this problem through workshops for service providers, to clarify values and increase empathy and respect for women with unwanted pregnancies.
Other ways to monitor and ensure quality of care in developing and developed countries alike include the following: oversight by an independent national advisory body, decisions as to whether or not the procedure will be covered by national health insurance, the standards that approved institutions must meet, regulation of fees for services and requirements for record-keeping, and the collection of data. In Guyana, data collection includes relevant demographic information about the woman, length of pregnancy, reasons for abortion, type of procedure, any complications and whether and what kind of contraceptive method was provided. Where deaths from dangerous abortions were previously high, and to ensure that the mortality rate declines towards zero, the collection of baseline data and regular audit of all reported abortion-related deaths, as part of broader maternal mortality audits, will reveal continuing risks, allowing discussion and action to reduce these.
Guidelines for health service professionals are valuable for ensuring equity of access and quality of care. The United Kingdom Royal College of Obstetricians and Gynaecologists is currently preparing evidence-based guidelines that cover organization of services, information for women, pre-abortion assessment, abortion procedures, management of complications and after-care.- pp.586-587
- Although abortion has been legal in India since 1972, interviews with 67 women in rural Maharashtra in 1997 found that only 18% knew that this was the case, while 64% thought it was not, and the remainder were unsure. Even those who knew it was legal sometimes had inadequate or incorrect information about whether husbands' consent was needed eligibility for abortion, and the time limits within which abortion is permitted.
In Puerto Rico, although abortion has been legal for 20 years (a consequence of its commonwealth status with the USA), there is still a widespread perception that abortion remains illegal. Public information on where women can get an abortion is very limited, and clinics still use euphemisms to suggest that abortion services are provided. Medical students also know very little about what is permitted.
In Mozambique, although abortion has not been legalized as such, safe terminations have been available at the main hospital in Maputo since 1981 in order to reduce mortality from unsafe abortions. However, a study reported in 1997 found that young women who had recently migrated to the city, who did not have a steady partner, who were from poorer socioeconomic groups, who did not use contraception and who had no previous abortions were less likely to know that they could obtain a safe abortion at that hospital. They were more likely to seek clandestine abortions and experience complications, for which they went to that same hospital. Thus, the women who were most at risk were also those who had the least information.
Hence, widespread public awareness is an important component in making abortion safe where it has previously been unsafe; women need to know that safe abortions are not only permitted but available.- p.587
- Much can be done despite the difficulties of changing national abortion laws. Women's health groups and other advocates, parliamentarians and health professionals, can work together to support the right of women not to die from unsafe abortions and to ensure that they receive treatment for complications. They can urge hospitals not to report women and legitimate service providers to the police, as well as advocate for the decriminalization of abortion. In countries where the letter of the law is not a primary obstacle, they can also campaign for a choice of safe abortion methods, improvements in regulations governing the registration of providers and facilities, and for better training for providers. Additionally, they can monitor accessibility, affordability, and quality of care in these services.
Even where legal change has not taken place or is not likely to happen quickly, improvements in the abortion methods used and in the responsiveness of providers to the demand for safer abortions can improve the situation to some extent. Committed doctors can make an important difference by providing treatment for abortion complications, interpreting the law in a liberal way and providing safe services where these are legal, and training providers in the safest techniques to reduce mortality and morbidity. Furthermore, courts can pass judgements that result in shorter prison sentences and fewer prosecutions of women for having abortions, and help to open the way to law reform. This occurred in Nepal in the 1990s as it did in countries such as Spain in the 1970s.- pp.587-588
- Abortion law reform is a necessary condition for making abortion safe, though it is not sufficient in itself. Women remain vulnerable where safe abortion is not legally sanctioned because quality of care cannot be assured, abuses cannot be challenged and both women and providers remain at risk of prosecution, blackmail, and social and professional stigma. The dedication of individuals to providing treatment for abortion complications or safe abortions in a context of clandestinity, important as it is, cannot make up for the absence of a legal framework and national programmes. In the long run, abortion needs to be decriminalized in order for it to be made safe.
Although law, policy and women's rights are central to this issue, making abortions safe is above all a public health responsibility of governments. Moreover, reducing maternal mortality by making abortions safe is also an important part of the international commitment made in Cairo in 1994 at the UN International Conference on Population and Development (ICPD) and re-affirmed at the Cairo+5 meeting in 1999. The practical steps to bring about the changes outlined in this article could be achieved by most countries in a few short years once they have committed themselves to making abortion safe.- p.587
“Practice Of Fertility Control: A Comprehensive Manual” (2007)
[edit]Chaudhuri SK (2007). “Practice Of Fertility Control: A Comprehensive Manual” (7th ed.). India: Elsevier.
- It has also been found that abortion rates are not lower in areas where abortion is generally restricted by law (where many abortions are performed under unsafe conditions with high morbidity and mortality rates) than in areas where abortion is legally permitted (Henshaw et al., 1999).
- Incidence, pp.238-239
- The WHO defined ‘unsafe abortion’ as ‘a procedure for terminating an unwanted pregnancy either by persons lacking the necessary skills or in an environment lacking the minimum medical standards or both’ (IPPF, 2004).
An estimated 46 million pregnancied end in induced abortion globally each year, and out of these nearly 20 millinon are unsafe; 95% of these occur in developing countries (WHO, 1998). Globally, there is a ratio of one unsafe abortion for every seven lie births, but in some countries like Latin America and the Caribbean, there is more than one unsafe abortion for every three live births (WHO, 1998). About 13% of pregnancy-related deaths have been attributed to complications resulting from unsafe abortion. They probably number about 67,000 deaths annually (WHO, 2003) <r> Nearly 90% of unsafe abortions take place in the developing countries, and more in those countries where abortion is illegal or quasi-legal but where facilities of legalized abortion are inadequate. It is estimated by the WHO (1994) that in the Indian subcontinent 15-24 unsafe abortions take place per 100 women aged 15-49 years. Unsafe abortions are performed 15-20 times more oftener than safe legal abortions in India at present.- Unsafe abortion, pp.259-260
- Unsafe abortions are performed in various ways: (1) severe and prolonged massaging of the abdomen as in some African countries; (2) oral administration of concoctions and drugs which are often toxic and poisonous; (3) injections of so-called ecbolics and high doses of hormones; (4) vaginal douching of hot and caustic solutions, producing burns; (5) attempted intrauterine introduction of metal rods, hairpins, knitting devices and instruments which often perforate into the peritoneal cavity or injure other pelvic organs; (6) introduction of indigenously available sticks of the shrub, “calotropis gigantean” in India and “Jatropha” and “Commelina” plants in Africa; (7) transcervical introduction of cloth pieces, gauze, catheters, vougies and pastes and (8) D&E performed in a clandestine way. Unsafe abortions are mostly performed ny untrained village abortionists, chiefly female “dais” or untrained midwives, village unlicensed doctors (quacks), licensed doctors without any training in midwifery and family planning, as well as trained doctors including gynaecologists who do not wish to disclose these procedures for socioeconomic and legal reasons. Many illegal abortions are self-induced.
- Methods and personnel, p.260
- Legal abortion is one of the safest of surgical procedures, the mortality rate per 100,000 abortions being 1.4 in USA, 2.1 in Canada and 3.0 in England and Wales; it is about 11 times safer than tonsillectomy and 100 times safer than appendicetomy in USA. In contrast, the death rate from illegal abortion in developing countries is about 50-100 per 100,000 procedures; illegal abortion is 10-250 times more dangerous than any kind of contraceptive measure, depending on the age of the woman and the method used.
It is estimated )WHO, 1994) that in India 70-89 women per 100,000 live births die from unsafe abortion; the risk of death is 1 in 250 procedures. The common causes of death are peritonitis, septicaemia, endotoxic shock, haemorrhage and tetanus. Besides, lots of these cases suffer from complications usch as trauma to the pelvic organs, cervical lacerations, uterine perforation, damage to the bladder and intestines, renal failure and pelvic abscess. Chronic suffering from chronic pelvic cellulitis, tubo-ovarian mass, pelvic adhesions, thrombophlebitis and sterility as sequelae of illegal abortion make life miserable for many of these unfortunate cases. Other possible consequences are increased risk of ectopic pregnancy,- p.260
“The Human Drama of Abortion: a Global Search for Consensus” (2006)
[edit]Faúndes A, Barzelatto J (2006). “The Human Drama of Abortion: a Global Search for Consensus”. Vanderbilt University Press. p. 21. ISBN 9780826515261.
- Safe abortion and unsafe abortion are common terms that are used frequently in international documents. WHO (1992) defines unsafe abortion as “a procedure for terminating an unwanted pregnancy either by persons lacking the necessary skills or in an environment lacking the minimal medical standards, or both” (AbouZhar and Ahman, 1998, p.276). In contrast, a medical or surgical abortion performed by a well-trained professional with the necessary resources and in a suitable medical environment is considered to be a safe abortion because there is little risk to the woman. The maternal mortality observed with safe abortion is no more than one in one hundred thousand procedures, and there are few complications. In fact, if the abortion is performed early in the pregnancy (up to twelve weeks), the associated morbidity and mortality are lower than those of a normal full-term delivery.
Most unsafe abortions are performed in countries where they are legally restricted. However, some occur in countries where abortion is legal but the conditions under which the procedure is performed are inadequate. It is also noteworthy that many safe abortions are performed in countries where abortion is legally restricted. Therefore, it is important that the usage of the terms safe abortion and unsafe abortion be kept distinct from the usage of the terms legal abortion and illegal abortion.- Safe and Unsafe Abortion, pp.21-22
- Since ancient times, a wide range of methods has been used to induce abortions, from very primitive procedures to modern surgical techniques and medications.
Traditionally and even today, a popular method of unsafe abortion has been the introduction of a solid, pointed object through the uterine cervix to cause the membrane protecting the embryo/fetus to rupture and allow a pathway for infection. The woman’s own body then rejects the infected embryo or fetus. A number of different potions and herbal teas have also been used with questionable effectiveness. A popular traditional method used mostly in Asia is to massage the pregnant woman’s abdomen forcefully. All of these methods commonly result in incomplete abortions with severe uterine or generalized infections, requiring emergency care to save the woman’s life. <br The vast majority of maternal deaths caused by induced abortion result from the performance of these primitive procedures under unhygienic conditions. Fortunately, an increasing number of abortions are performed using more modern techniques classified into two main categories: (1) instrumental evacuation of the uterine cavity through the cervix, either by dilation and curettage (D & C) or, preferably, by intrauterine vacuum aspiration and (2) the administration of medications, also referred to as pharmacological abortions. Other methods, such as the injection of substances into the uterus or the surgical removal of the fetus through the abdomen (micro-cesareans), have been abandoned because of the higher risk of complications and death (Cates et al. 1977).- Methods of Pregnancy Termination, p.22
- In general, the more advanced the pregnancy is at the time of abortion, the greater the risk of complications and death (Atrash et al., 1987; Lawson et al., 1994). Most abortions are performed within the first twelve weeks of pregnancy, but the number performed later-particularly in cases of severe fetal malformation or risk to the life of the woman-is not insignificant. In such cases, misoprostol offers the great advantage of being highly effective after twelve weeks, inducing abortion with characteristics that mimic miscarriage.
- p.24
"Evidence supporting broader access to safe legal abortion" (1 October 2015)
[edit]Faúndes, Anibal; Shah, Iqbal H. (1 October 2015). "Evidence supporting broader access to safe legal abortion". International Journal of Gynecology & Obstetrics. World Report on Women's Health 2015: The unfinished agenda of women's reproductive health. 131: S56–S59. doi:10.1016/j.ijgo.2015.03.018. ISSN 0020-7292. PMID 26433508.
- Unsafe abortion continues to be a major cause of maternal death; it accounts for 14.5% of all maternal deaths globally and almost all of these deaths occur in countries with restrictive abortion laws. A strong body of accumulated evidence shows that the simple means to drastically reduce unsafe abortion-related maternal deaths and morbidity is to make abortion legal and institutional termination of pregnancy broadly accessible. Despite this evidence, abortion is denied even when the legal condition for abortion is met. The present article aims to contribute to a better understanding that one can be in favor of greater access to safe abortion services, while at the same time not be “in favor of abortion,” by reviewing the evidence that indicates that criminalization of abortion only increases mortality and morbidity without decreasing the incidence of induced abortion, and that decriminalization rapidly reduces abortion-related mortality and does not increase abortion rates.
- A recent assessment of global maternal, newborn, and child health indicated that unsafe abortion continues to exert a heavy toll on women’s lives and well-being as it accounts for 14.5% of all maternal deaths globally. These deaths are entirely preventable if women have access to safe legal abortion, as has been shown by the accumulated evidence and abortion reforms in a number of countries, including Guyana, Nepal, and South Africa. Of course, the primary prevention for unintended pregnancy is through consistent use of effective contraception. However, no contraceptive method is 100% effective, resulting in accidental pregnancies that the WHO has estimated to total 33.5 million each year. In addition, many women—mostly young—suffer sexual violence and rape and some become pregnant with an unwanted pregnancy. Thus, the simple means to practically eliminate all unsafe abortion-related complications and maternal deaths is to make abortion legal and institutional termination of pregnancy broadly available and accessible.
- Declaring that one is in favor of greater access to safe abortion is not an easy decision for any individual or institution in the current environment of abortion stigma, harassment, and political backlash. It is only after careful evaluation of the evidence and the professional and ethical obligation to protect women’s health and lives that an organization such as FIGO can publicly declare to be in favor of women’s access to safe abortion. Hence, it is important to make clear the basis for such a courageous position.
The first basic reason to favor broad access to safe abortion is that most women faced with an unintended/unwanted pregnancy resort to abortion, irrespective of the law. Where access to abortion is restricted, women will have no option but to risk their lives and health by resorting to an unskilled clandestine provider performing abortion under unhygienic conditions. Unsafe abortions cause suffering and death, as shown by numerous studies worldwide. - While the unsafe abortion rate is higher in Latin America than in Africa, the risk of death as a result of unsafe abortion is about 15 times higher for a woman living in Africa than for a woman living in Latin America. It is a rare exception for an abortion-related death to occur in a private hospital providing services to economically privileged women. Almost all deaths occur in public hospitals where poor women receive care or in their own homes, or wherever an abortion practitioner provides a clandestine and unsafe abortion service. Thus, the poorest women in the poorest countries are the main victims of criminalization of abortion and lack of access to safe abortion care.
"Global, regional, and subregional classification of abortions by safety, 2010-14: estimates from a Bayesian hierarchical model" (November 2017 updated November 25, 2017)
[edit]Ganatra B, Gerdts C, Rossier C, Johnson BR, Tunçalp Ö, Assifi A, et al. (November 2017 updated November 25, 2017). "Global, regional, and subregional classification of abortions by safety, 2010-14: estimates from a Bayesian hierarchical model". Lancet. 390 (10110): 2372–2381. doi:10.1016/S0140-6736(17)31794-4. PMC 5711001. PMID 28964589.
- Global estimates of unsafe abortions have been produced for 1995, 2003, and 2008. However, reconceptualisation of the framework and methods for estimating abortion safety is needed owing to the increased availability of simple methods for safe abortion (eg, medical abortion), the increasingly widespread use of misoprostol outside formal health systems in contexts where abortion is legally restricted, and the need to account for the multiple factors that affect abortion safety.
- Of the 55.7 million abortions that occurred worldwide each year between 2010–14, we estimated that 30.6 million (54.9%, 90% uncertainty interval 49.9–59.4) were safe, 17.1 million (30.7%, 25.5–35.6) were less safe, and 8..0 million (14.4%, 11.5–18.1) were least safe. Thus, 25.1 million (45.1%, 40.6–50.1) abortions each year between 2010 and 2014 were unsafe, with 24.3 million (97%) of these in developing countries. The proportion of unsafe abortions was significantly higher in developing countries than developed countries (49.5% vs 12.5%). When grouped by the legal status of abortion, the proportion of unsafe abortions was significantly higher in countries with highly restrictive abortion laws than in those with less restrictive laws.
- Increased efforts are needed, especially in developing countries, to ensure access to safe abortion. The paucity of empirical data is a limitation of these findings. Improved in-country data for health services and innovative research to address these gaps are needed to improve future estimates.
- Despite scientific advances that enable the provision of safe abortion at the primary care level, unsafe abortions persist and result in a high burden of complications; maternal death; and substantial costs to women, families, and health systems.
WHO defines unsafe abortion as a procedure for termination of a pregnancy done by an individual who does not have the necessary training or in an environment not conforming to minimal medical standards. However, abortions done in accordance with these standards are considered safe and the risk of severe complications or death is minimal. The people, skills, and environment needed to meet medical standards are outlined in WHO guidelines, which are updated periodically. In the 25 years since unsafe abortion was defined, evidence has evolved and simple technologies, such as manual vacuum aspiration and medical abortion (with mifepristone and misoprostol, or misoprostol alone if mifepristone is unavailable), have made the provision of safe abortions possible at the primary care level and by health workers other than doctors. The conditions leading to a safe abortion are in turn affected by numerous factors, including the laws and policies on abortion (ie, legal context), the socioeconomic conditions, the availability of safe abortion services, and the stigma surrounding abortion. Stigma related to seeking or provision of abortion is increasingly being recognised as having an effect on how and where women access care and who provides care. - Evidence before this study
From 1990 to 2008, WHO used indirect estimation techniques to determine the incidence of abortion in countries with restrictive laws and in countries with more permissive laws but where a large number of abortions took place illegally. These abortions were labelled as unsafe, and these estimates were integrated with estimates of the incidence of legal abortion worldwide, developed by the Guttmacher Institute. Such global, regional, and subregional estimates of safe and unsafe abortions have been produced for 1995, 2003, and 2008. The most recent estimates were published in The Lancet in 2012 and concluded that 21.6 million (49%) of 43.8 million abortions in 2008 were unsafe. However, to date, categorisation of safety based on the actual characteristics of abortion has never been attempted.
Added value of this study
The new approach used in this study represents a significant advance compared with previously published estimates for several reasons. First, this study is the first to explicitly align the operational estimation of safety categories with the conceptual definition of unsafe abortion used by WHO and with the technical standards of care outlined in WHO guidelines. Second, use of a model-based approach allowed for consideration of multiple factors affecting abortion safety in a systematic way. Third, replacement of the dichotomous division of safety with a three-tiered classification (safe, less safe, and least safe) permitted a more nuanced description of the spectrum of varying situations that constitute unsafe abortion and the increasingly widespread substitution of dangerous, invasive methods with use of misoprostol outside formal health systems in some legally restricted contexts to be accounted for. Fourth, this study is the first to include uncertainty bounds around the estimates.
Implications of all the available evidence
The three-tiered categorisation of safety in this paper replaces the previous dichotomous classification of safety. Although simple and safe primary care interventions for safe abortion exist, about 25.1 million unsafe abortions took place worldwide each year between 2010 and 2014, of which 24.3 million (97%) were in developing countries. The findings call for the need to ensure access to safe abortion to the full extent of the law, particularly in low-income regions of the world. Efforts are also needed to replace the use of unsafe methods with safe methods. The study also highlighted the need for routine collection of monitoring data within health systems and development of innovative research methods to address data gaps to improve future estimates. - Estimates of the magnitude of unsafe abortion have been periodically produced since 1995. Because of the paucity of data, previous estimates relied on the legality of abortion in a given setting and a qualitative assessment of the country context as the primary basis for distinguishing safe from unsafe abortions. This approach to classification was a reasonable proxy for safety in an era when only facility-based surgical abortions met medical standards of safety and when unsafe abortions in legally restricted contexts were usually done with dangerous and invasive methods. However, the increasingly widespread substitution of such dangerous methods with misoprostol outside formal health systems necessitates reconceptualisation of how we categorise abortion safety to capture the spectrum of situations that constitute unsafe abortion and the continuum of risk they represent.
About 55.7 million abortions took place worldwide every year during the period of 2010–14, the most recent period for which information about abortion incidence is available. Here, we present a new theoretical framework within a Bayesian hierarchical model to generate cross-sectional estimates of the global, regional, and subregional distributions of these abortions by safety categories. In doing so, we replace the dichotomous classification of abortion safety that has been used since 1990 with a three-tiered classification underpinned by WHO recommendations for safe abortion. - Theoretical framework
We used the WHO definition of unsafe abortion and WHO technical guidelines to create a three-tiered classification of abortion:
Safe abortion: provided by health-care workers and with methods recommended by WHO
Less-safe abortion: done by trained providers using non-recommended methods or using a safe method (eg, misoprostol) but without adequate information or support from a trained individual
Least-safe abortion: done by untrained people using dangerous, invasive methods
We organized factors affecting safety of abortion into conceptual domains:
Availability of safe methods, trained providers, and facilities
Legal context of abortion
Financial access to services
Abortion stigma
Overall development of health services and infrastructure - We used the WHO definition of unsafe abortion and recommendations within WHO guidelines on safe abortion to conceptualise abortion safety as falling into three categories: safe, less safe, and least safe. The less-safe and least-safe categories together reflect the spectrum of unsafe abortions. We classified abortions as safe if they were done with a method recommended by WHO (medical abortion, vacuum aspiration, or dilatation and evacuation) that was appropriate to the pregnancy duration and if the person providing the abortion was trained. We classified abortions as less safe if only one of the two criteria were met—ie, either the abortion was done by a trained provider but with an outdated method (eg, sharp curettage) or a safe method of abortion (eg, misoprostol) was used but without adequate information or support from a trained individual. We classified abortions as least safe if they were provided by untrained individuals using dangerous methods, such as ingestion of caustic substances, insertion of foreign bodies, or use of traditional concoctions.
From a review of the literature and expert group discussions, we identified factors affecting abortion safety at the country level. We organised these factors into five conceptual domains: (1) the abortion service-delivery environment, which encompasses the availability of safe methods, trained providers, and facilities equipped to provide safe abortion; (2) financial access to services, which refers to a woman's ability to pay for safe abortion services within or outside her country of residence; (3) abortion stigma, which reflects attitudes toward abortion and is associated with gender inequality regarding women's empowerment, autonomy, and agency;7 (4) legal context, which accounts for the legal grounds for abortion, associated laws and policies, and their interpretation and implementation; and (5) development, which includes the overall development level of health services and health infrastructure. - During 2010–14, 55.7 million abortions occurred annually worldwide, of which 30.6 million (54.9%, 90% UI 49.9–59.4) were safe. Almost all abortions in developed countries (87.5%, 81.9–89.6), and roughly half of those in developing countries (50.5%, 45.2–55.9), were safe.
- We estimated that 17.1 million (30.7%, 90% UI 25.5–35.6) abortions worldwide for 2010–14 were less safe and that 8.0 million (14.4%, 11.5–18.1) abortions were least safe. Thus, combining the less-safe and least-safe categories, 25.1 million (45.1%, 40.6–50.1) abortions were done in unsafe circumstances each year.
- The distribution of abortions across safety categories was similar across developed subregions, with the exception of eastern Europe, where the proportion of safe abortions was marginally lower than for other subregions in Europe. Among developing regions, eastern Asia (including China) had a safety distribution similar to that of developed countries. Only in three other developing subregions (southeastern Asia, western Asia, and southern Africa) did the proportion of safe abortions exceed 50%. Other than for southern Africa, the proportion of safe abortions was 25% or less in all of Africa and throughout Latin America. However, in Latin America, most unsafe abortions were categorised as less safe, whereas, in Africa, almost all unsafe abortions were categorised as least safe. The highest proportion of least-safe abortions occurred in middle Africa, followed by western Africa and eastern Africa.
- Given that the number of abortions in the subregions of Micronesia, Polynesia, and Melanesia were small, we did not separate Oceania into its subregions. Thus, the results for Oceania reflected a mix of safety scenarios. When the Australia–New Zealand subregion was considered on its own, 92.3% (90% UI 89.3–95.4; data not shown) of abortions were safe, similar to the pattern in other developed regions.
When the distribution of abortion safety was considered by the legal status of abortion, 87.4% (90% UI 79.2–92.0) of all abortions in the 57 countries in which abortion was available on request were safe compared with 25.2% (14.5–41.0) in the 62 countries where abortion was completely banned or allowed only to save the woman's life or to preserve her physical health. In such legally restrictive settings, nearly a third of abortions (31.3%, 90% UI 21.0–41.9) were categorised as least safe. A direct association was also seen between abortion safety and country income level; most abortions in upper-middle-income countries (67.1%, 58.7–75.7) and high-income countries (82.2%, 75.8–85.7) were safe compared with about one in five abortions (21.8%, 17.4–30.7) in low-income countries. The proportion of abortions that were least safe was also significantly higher in developing countries with the most restrictive laws than in developed countries with similarly restrictive laws (31.3% vs 0.3%; data not shown). - No clear association was observed between the incidence of abortion in UN DESA subregions and the distribution of safe abortions. However, the three regions with incidences of fewer than 30 per 1000 women (northern America, northern Europe, and western Europe) also had the highest proportions of safe abortions. Similarly, no clear association was observed between the proportions of unsafe abortions by subregion and case fatality rates (data not shown). However, an association was seen between the proportions of least-safe abortions by subregion and the case fatality rates; most subregions with a high proportion of least-safe abortions had high case fatality rates.
- The results showed a disparity in abortion safety between developed and developing regions. In 2010–14, almost all abortions in developed countries were safe, although a small proportion of less-safe abortions was also seen—notably in eastern Europe—probably due to the persistence of outdated medical practices such as sharp curettage. In eastern Europe, as in many parts of Asia, development of evidence-based national standards and guidelines and training of providers could result in substantial improvements in the safety and quality of abortion care.
The subregions with the highest proportions of safe abortions (northern Europe and northern America) also showed the lowest incidence of abortion. Most countries in these two subregions have less restrictive laws on abortion, high contraceptive use, high economic development, high levels of gender equality, and well developed health infrastructures, suggesting that achievement of both low incidence of abortion and high safety in such contexts is possible.
Although eastern Asia was similar to developed regions, fewer than one in two abortions in south-central Asia and about one in four abortions in Africa were safe. Most abortions in Africa were characterised as least safe, suggesting that use of dangerous invasive methods by untrained individuals is common. Although the estimates of case fatality rates should be interpreted with caution because they were calculated with information from several different estimates and various time periods, our results suggested that the subregions with the highest proportions of least-safe abortions also had the highest case fatality rates. This finding might be due to the more serious complications arising from least-safe abortions and the poor health infrastructure to treat complications when they occur. Multifaceted interventions addressing legal, policy, and health system barriers; health-worker shortages; provider attitudes; gender inequality; and abortion stigma are needed.
Only about one in four abortions in Latin America were safe, although most unsafe abortions were categorised as less safe, reflecting the transition of use of dangerous methods to use of misoprostol outside formal health systems in this region.19 Such abortions might result in fewer complications than abortions done using dangerous methods, as shown by the lower case fatality rates in regions with a high proportion of less-safe abortions than in regions with a high proportion of least-safe abortions. However, these regions also have better functioning health systems and better access to care to treat complications when they occur. Self-management of medical abortion in early pregnancy is an evidence-based option in WHO guidelines, however the use of misoprostol outside of the formal health system, often without access to appropriate information and a trained health-care worker if needed, does not represent a standard of care, but rather an absence of safe options. Thus, despite lower case fatality rates, these abortions are considered less safe and structured health systems interventions that address access to information, medications, and support to women are needed.
The analysis showed a positive association between safe abortions and less restrictive laws. Such laws might promote an enabling environment for trained providers and improve access to safe methods. The highest proportions of safe abortion were seen in developed countries with less restrictive laws, suggesting that both the legal grounds and overall development of a country have a part in abortion safety.
Scarcity of data for the period before 2010–14 did not allow for a trend analysis with this model. Comparisons with previously published estimates of the proportions of safe and unsafe abortions cannot and should not be made because the theoretical framework, the data used, and the analytical approaches are different.
To the best of our knowledge, this study is the first to align the measurement of abortion safety with WHO's definition4 of unsafe abortion and to link the categorisation of safety to current technical standards in WHO guidelines.5, 6 Furthermore, the three-tiered classification allowed for a more nuanced gradation of safety that distinguished the least-safe abortions from other types of unsafe abortion. The use of a model-based approach resulted in a systematic consideration of multiple factors that affect the conditions under which abortions take place and allowed, for the first time, the construction of uncertainty bounds around the estimates. - The possibility of prosecution for seeking an abortion might also lead women to unsafe options; however, we were unable to quantify this risk for use as a covariate. Additionally, although abortions in both the first trimester and later are safe if done according to WHO standards, the risk of complications does increase with increasing duration of pregnancy. However, we were unable to account for this in the model because of data constraints.
Innovative research to address these gaps is urgently needed, especially in contexts where many abortions occur outside formal health systems. Where legal grounds for provision of an abortion exist, increased commitment to collection and standardised reporting of routine data with monitoring indicators recommended by WHO are needed. Improvements in data would also allow future estimates to be disaggregated to the country level; for inequalities related to age, marital status, and economic conditions to be examined; and for national-level progress in increasing access to safe abortion to become visible.
In conclusion, this analysis suggested that unsafe abortion is still a major problem in developing countries and that progress towards safer abortion is needed, even in some developed countries. Although efforts to increase the availability, accessibility, and affordability of contraception can reduce the incidence of unintended pregnancies and, therefore, abortions, it is essential to combine this strategy with interventions to ensure access to safe abortion. Both strategies are needed to eliminate unsafe abortion and to fulfil the global commitment to the Sustainable Development Goal of universal access to sexual and reproductive health.
"Unsafe abortion: the silent scourge" (2003-12-01)
[edit]Grimes DA (2003-12-01). "Unsafe abortion: the silent scourge"]. British Medical Bulletin. 67 (1): 99–113. doi:10.1093/bmb/ldg002. PMID 14711757.
- An estimated 19 million unsafe abortions occur worldwide each year, resulting in the deaths of about 70,000 women. Legalization of abortion is a necessary but insufficient step toward improving women’s health. Without skilled providers, adequate facilities and easy access, the promise of safe, legal abortion will remain unfulfilled, as in India and Zambia. Both suction curettage and pharmacological abortion are safe methods in early pregnancy; sharp curettage is inferior and should be abandoned. For later abortions, either dilation and evacuation or labour induction are appropriate. Hysterotomy should not be used. Timely and appropriate management of complications can reduce morbidity and prevent mortality. Treatment delays are dangerous, regardless of their origin. Misoprostol may reduce the risks of unsafe abortion by providing a safer alternative to traditional clandestine abortion methods. While the debate over abortion will continue, the public health record is settled: safe, legal, accessible abortion improves health.
- The tragedy of unsafe abortion goes largely unnoticed, a silent scourge in developing countries. Were a jumbo jet carrying 400 women of reproductive age to crash today in Central Africa, with loss of all lives on board, the response would be prompt and predictable. International press coverage would start within hours, with television crews and teams of investigators pouring over the smoking wreckage in search of the cause. Reporters would dutifully interview grieving relatives. Imagine the global response if yet another identical jet, loaded to capacity with women younger than 45 years, met the same fate a few days later in Southeast Asia. Then another in South America. And another in the Caribbean. Suppose that, over a year, 168 such airliners went down, killing all on board. How long would governments of the world allow such an airplane to fly before demanding corrective action?
- Year in and year out, this many women (about 70,000) die of complications of unsafe abortion1. An estimated 19 million desperate women each year risk degradation, disease and death through such abortions. The response of the international community remains muted, perhaps in part because the victims are all women, they are mostly of colour, and they live in developing countries. They die in places like Ouagadougou, not Oslo. Their deaths are all the more tragic, since nearly all are preventable.
More is known today about the epidemiology of legally induced abortion than any other operation. In contrast, huge gaps persist in our understanding of the incidence, morbidity and mortality of unsafe abortion. Because of stigma or fear of legal reprisals, unsafe abortions are grossly under-reported, and the complications thereafter are often concealed or attributed to spontaneous miscarriage. For example, a recent hospital study from Ethiopia reported that 86% of abortions were spontaneous, yet the mean gestation age at admission was 15 weeks, an improbable scenario.
Despite gross under-reporting (due in part to deaths outside of hospital), unsafe abortion remains one of the five leading causes of maternal death in most developing countries.
For every woman who dies, many more are left wounded, some with life-long consequences, including infertility, chronic pelvic pain and genital trauma.
Through the leadership of the World Health Organization, several important publications in recent years have addressed the complex issue of unsafe abortion and its remedies. These include review articles, books and the May 2002 issue of Reproductive Health Matters. Since the social and political approaches to the problem of unsafe abortion have been explored in detail in these references, I will focus on the medical aspects. This article will review the scope of the problem and address strategies for prevention and treatment of unsafe abortion and its sequelae. - ‘Unsafe abortion’ is defined by the World Health Organization as ‘a procedure for terminating an unwanted pregnancy either by persons lacking the necessary skills or in an environment lacking the minimal medical standards or both’. Of note, ‘unsafe’ is not a synonym for ‘illegal’ or ‘clandestine’. For example, legal abortions may be unsafe because of poorly trained clinicians, inadequate facilities, or both.
- Legalization of abortion can dramatically improve women’s health. Several natural experiments reveal the potential. In the USA, for example, the legalization of abortion led to the emptying and then closing of septic abortion wards in major metropolitan hospitals. On a nationwide basis, deaths from illegal abortion nearly disappeared within a few years of nationwide legalization.
The opposite was observed in Romania after abortion was made inaccessible by the dictator Ceaucescu. Birth rates remained stable, but maternal mortality rates soared to the highest in Europe. Women resorted to unsafe abortion to control their fertility, and many died. When Ceaucescu was deposed and abortion again became accessible, maternal mortality rates plummeted.
More recently, Poland severely restricted abortion after decades of easy access. The result has been an estimated 80,000–200,000 clandestine abortions annually, women travelling to other countries for service, an increase in the cost of abortion, and no change in birth rate. Clearly, the public health has suffered as a result. - Legalization of abortion, although important, is insufficient. India has had legal abortion on the books for several decades, as has Zambia. However, the ‘devil is in the details’. In both countries, numerous impediments to care, ranging from requirement for several doctors’ signatures to lack of accessible clinics, prevent most women in need from getting care in a timely fashion. Hence, women continue to rely on unsafe abortion to control their fertility.
A companion article in this issue recounts the South African experience. A recent analysis of the public health impact of legalization of abortion in 1997 found little benefit. However, the low uptake (abortion ratio 36 per 1000 live births; abortion rate 3 per 1000 women aged 12–49 years) suggests a large unmet need for safe, legal abortion. By comparison, the corresponding abortion ratio and rate for the USA are 264 and 17, respectively. Hence, many women in South Africa probably still resort to unsafe practices. - Women in developing countries often must run a gauntlet to get a safe abortion. Problems include the metropolitan concentration of abortion providers, consent to contraceptive sterilization as a prerequisite, lack of an appointment system and hefty charges for services that should be free. Lack of confidentiality of providers regarding minors poses another obstacle for adolescents. Even in India, where abortion has been legal for three decades, most women in one survey were unaware that it was legal.
- Simple, inexpensive equipment is needed for providing abortion services and caring for most complications that occur. Elaborate operating theatre set-ups and availability of general anaesthesia, required by some bureaucracies as a prerequisite for licensing20, are inappropriate. Provided that arrangements and transportation (e.g. a jeep-taxi in rural India or a speedboat in Bangladesh) are in place for quickly moving patients to hospitals, if needed, free-standing abortion clinics around the world have achieved an outstanding safety record. Although abortion equipment is simple, it must be available. A major barrier to care in many developing countries is the lack of basic equipment and drugs for all gynaecological care.
- Two principal determinants of the safety of legally induced abortion are gestational age and choice of method. Both are closely interrelated. Abortion morbidity as a function of gestational age plots as a ‘J’-shaped curve. The nadir for complication rates by vacuum aspiration occurs at 7–10 weeks from last menses. Among first-trimester surgical procedures, suction curettage is superior to sharp curettage in speed, comfort and safety. The metal curette, introduced in 1843 by Recamier to ‘scrape off uterine fungosities’, sparked an immediate, strident debate. Scanzoni protested that the metal curette was ‘an instrument based on an entirely erroneous thought, which takes from it all practical utility’. A century and a half later, solid evidence supports Scanzoni’s dim view of the metal curette; it should be relegated to museums.
- Local anaesthesia is safer than general anaesthesia for early abortion; it is cheaper as well. Indeed, in some countries, general anaesthesia is the leading cause of death from early abortion. However, local anaesthesia is not without risks. Toxicity and occasional deaths can occur if clinicians exceed safe doses of local anaesthetic agents, especially those of the amide class (lignocaine family). In the USA, no deaths have been attributed to local anaesthesia with ester anaesthetics (procaine family), although their use is less common. In general, clinicians should use the smallest amount of the lowest concentration adequate for the purpose. For example, 1% lignocaine is one of the more toxic local anaesthetic agents; using a 0.5% solution provides excellent anaesthesia with a wider margin of safety.
- Formal pathology examination of the uterine contents is unnecessary. In contrast, visual inspection of the aspirate by the clinician or a designee is mandatory before the patient leaves the facility. A number of women have died from unsuspected ectopic pregnancies in this setting. Confirmation of the appropriate type and volume of tissue excludes ectopic pregnancy (except for the rare ectopic twin) as well as failed attempted abortion. The requisite equipment is simple: a source of back-lighting (such as a horizontal X-ray viewing box), a mesh kitchen strainer and a shallow transparent dish (like that used for baking pies). When the rinsed tissue is suspended in water and examined with back-lighting, this simple set-up allows immediate identification of embryonic tissue as early as 5 weeks and recognition of molar pregnancy as well.
- Several ancillary measures lower morbidity as well. All patients having vacuum aspiration abortions should receive prophylactic antibiotics, although the optimal regimen remains unclear. Doxycycline is popular, given its low cost, high safety and wide spectrum. Rh-negative women should receive Rh immunoglobulin.
- Second-trimester abortion can also be performed surgically or pharmacologically. Through about 16 weeks, dilation and evacuation (D&E) is superior to labour-induction abortions. The comparative safety and acceptability of D&E versus labour-induction abortion at later gestational ages are currently unknown. Studies with abortifacients no longer used, such as intra-amniotic PGF, showed that D&E was superior to labour induction. One recent cohort study from a US hospital showed D&E to be significantly safer than labour-induction abortion, but selection bias was evident. Randomized controlled trials comparing contemporary regimens with D&E are needed to resolve this question. D&E has several appealing features for developing countries, including reducing reliance upon scarce hospital beds and resources.
- The range of abortion methods used varies widely in safety and efficacy. Oral abortifacients have included quinine, ampicillin, laundry bluing, turpentine, bleach, acid, tea made of livestock faeces and other vegetable concoctions. Potassium permanganate tablets and herbal preparations have been used vaginally. Foreign bodies inserted through the cervix include sticks, roots, wires, knitting needles, coat hangers, rubber catheters and bougies, ball-point pens, bicycle spokes and chicken bones. The last foreign body has led to unexplained infertility. Physical methods have included abdominal massage, and lifting of heavy weights.
In the past, more invasive methods, e.g. introducing foreign bodies into the uterus, were more effective in producing abortions. They also tended to carry greater risks of trauma and infection. In one study from the Ivory Coast, plant infusions carried a high risk of neurotoxicity and maternal death, while intrauterine approaches were related to peritonitis.
Access to misoprostol has changed the landscape of unsafe abortion in several ways. First, it provides safe entrée into medical care. In many countries where legal abortion is not available, women induce vaginal bleeding by inserting a foreign body through the cervix. Once a diagnosis of ‘spontaneous’ incomplete or inevitable abortion is made, the woman can have a uterine aspiration with appropriate medical care. Misoprostol can cause such bleeding without the risk of instrumentation. In one report from Brazil, the infection rate associated with misoprostol was significantly lower than that with alternative traditional methods. Second, if given in sufficient doses and with sufficient frequency, misoprostol alone can abort a high proportion of pregnancies. - A broad array of personnel perform unsafe abortions. Aside from the woman herself, others include physicians working at clandestine sites or in hospital operating theatres after hours. Others with medical experience include midwives, traditional birth attendants, pharmacists and nurses. Most worrisome are ‘untrained quacks’ whose motives may be financial and their skills negligible.
- While the benefit of prophylactic antibiotics for vacuum aspiration has been established, the advisability of prophylaxis after other types of abortion is unclear. A recent Cochrane review has found the evidence too sparse to reach a conclusion. Rh immune globulin should be given as indicated.
- The treatment of incomplete abortion is uterine evacuation. For decades, the assumption was that surgical removal was necessary. For first-trimester spontaneous abortion, that tenet has been challenged. Watchful waiting (expectant management) may be preferable, both in terms of emotional and physical welfare.
Alternatively, oxytocin has been used for decades to help expel tissue. More recently, misoprostol has attracted great attention as a uterotonic agent in this setting. A randomized controlled trial comparing surgical evacuation versus pharmacological evacuation with misoprostol found the latter to have fewer immediate complications; however, about half of those randomized to receive misoprostol later required surgical treatment. A Cochrane review in progress will compare expectant management with surgical intervention of miscarriage; another will compare medical (pharmacological) management of miscarriage.
Should surgical intervention be elected, suction curettage is preferable to sharp curettage. Vacuum aspiration (suction curettage) with either an electrical pump or syringe as vacuum source is the standard of practice. For management of incomplete second-trimester abortion, pharmacological agents or surgical evacuation are options. Specially designed grasping forceps for D&E procedures, such as the Bierer or Sopher forceps, can quickly empty a large uterus, whereas labour-induction methods may take hours. Time can be critical when severe infection or heavy bleeding occurs. Hysterotomy to produce abortion (or to manage abortion) is an obsolete operation. This approach is needlessly risky, painful and expensive. Alternative means of emptying the uterus are preferable. - While oxytocic agents can assist, the definitive treatment of haemorrhage usually is to empty the uterus. Should uterine trauma or coagulopathy be responsible, specific treatment is indicated. More commonly, however, the task is to remove remaining tissue and help the uterus contract. Massage of the uterus, or firm, sustained compression between a vaginal and abdominal hand, can help temporize.
Should surgical evacuation be necessary, this should not be delayed to allow for correction of anaemia. Young, healthy women tolerate operations with very low haematocrits. Prompt resuscitation with volume expanders, rather than red cells, and rapid transfer to the operating theatre are appropriate. Although colloids, such as albumin, dextran 70, hydroxyethyl starches and plasma protein fraction, have been widely recommended for fluid resuscitation, a Cochrane review found them of comparable benefit to crystalloids, which are much less expensive. Hence, the latter should be used. - As with most gynaecological infections, the microbiology of post-abortal infection reflects the resident flora in the lower genital tract. Hence, antibiotic coverage should include Gram-positive organisms, Gram-negative rods and anaerobes. Some women will have involvement with sexually transmitted pathogens. When foreign bodies are involved, Clostridium perfringens needs to be considered as well.
Antibiotic coverage will depend on local availability, but two-drug therapy should be considered for serious infections. Examples include those mentioned by the Centers for Disease Control and Prevention for treatment of pelvic inflammatory disease, such as cefotetan plus doxycycline, or gentamicin plus clindamycin. Parenteral therapy is preferred, although if gut function is adequate, doxycycline can be administered orally with excellent serum levels obtained. Should the patient not respond appropriately, the possibilities of retained tissue, perforation, abscess formation and bowel injury need to be considered and evaluated.
A common practice in some developing countries is to allow several days of antibiotic therapy (sometimes only oral tetracycline) for clinical improvement before removal of retained tissue. Based on considerable indirect evidence, this delay appears dangerous. Serum levels of antibiotics will be achieved within an hour, and if the patient has stable vital signs, she should undergo evacuation promptly. The mainstay of treatment is emptying the uterus, and antibiotics will not succeed until the necrotic, infected tissue is removed. The common theme in fatal septic abortion is delay: delay in recognition, delay in getting to care, then delay in initiating care upon arrival. - Septic shock remains an important cause of death from unsafe abortion. The cornerstones of management include treatment of infection and cardiovascular support. For example, adult respiratory distress syndrome develops in one-quarter to one-half of such patients, and this complication itself carries a high risk of death. High-dose, broad-spectrum antibiotics are indicated; no evidence indicates that triple antibiotics are preferable to two drugs.
Recently published systematic reviews have examined several ancillary treatments of sepsis and septic shock. Corticosteroids appear worthless and, indeed, may be harmful. They should not be used. Naloxone and intravenous polyclonal immunoglobulin appear promising, but more research is needed. Drotrecogin alpha also improves survival in severe sepsis, but is expensive.
Should the patient not respond, laparotomy is advisable. Similarly, abdominal exploration is usually indicated for uterine perforation with suspicion of organ injury, clostridial myometritis with intramural gas formation and suspected or confirmed pelvic abscess. - Bowel injury is a common consequence of uterine perforation, either with pointed instruments or grasping forceps. The distal ileum appears to be most vulnerable to injury, followed by the sigmoid. Figure depicts small bowel herniated through a perforation of the utero-vesical space during an attempted midtrimester abortion; the uterus was intact. Resection and reanastomosis of the necrotic bowel were required to save the patient’s life.
Injuries of the colon are easier to recognize than are small-bowel injuries, because of prompt peritoneal soiling. A normal or declining white blood count can be deceiving—a harbinger of septic shock. In general, any woman with abdominal pain after uterine instrumentation should be considered to have a perforation with bowel injury until proven otherwise. In the face of faecal contamination and severe peritonitis, colorectal injuries should not be repaired primarily. Diverting colostomy with take-down some months later is prudent. Patients should be advised about and consented for colostomy whenever a laparotomy is performed in this setting. As with other contaminated cases, the wound should have a delayed primary closure. - Lack of training, unfamiliarity with treatment options, out-of-stock drugs, broken equipment, sporadic electricity and water, and transportation challenges all threaten the health of women grappling with unsafe abortion. Perhaps the greatest danger of all is indifference—or overt disdain.
The lack of commitment on the part of medical and nursing staff to provide prompt, attentive and emotionally supportive care indirectly dooms women whose lives could easily be saved. Many women who reach medical facilities are met with suspicion and hostility, and their treatment deferred while other more ‘suitable’ candidates receive medical attention10. When dealing with patients in need, judgemental behaviour on the part of health care personnel is both medically dangerous and ethically indefensible.
While the debate over the role of abortion in society will continue unabated, the public health record is clear13. Safe, legal and accessible abortion improves the health of women and their families. When medical historians look back upon our era, the legalization of abortion will stand out, along with the development of antibiotics and immunization, as a public health triumph.
"Unsafe abortion: The preventable pandemic" (2006)
[edit]Grimes, DA; Benson, J; Singh, S; Romero, M; Ganatra, B; Okonofua, FE; Shah, IH (2006). "Unsafe abortion: The preventable pandemic" (PDF). The Lancet. 368 (9550): 1908–19. doi:10.1016/S0140-6736(06)69481-6. PMID 17126724. S2CID 6188636. Archived (PDF) from the original on 29 June 2011.
- Ending the silent pandemic of unsafe abortion is an urgent public-health and human-rights imperative. As with other more visible global-health issues, this scourge threatens women throughout the developing world. Every year, about 19–20 million abortions are done by individuals without the requisite skills, or in environments below minimum medical standards, or both. Nearly all unsafe abortions (97%) are in developing countries. An estimated 68 000 women die as a result, and millions more have complications, many permanent. Important causes of death include haemorrhage, infection, and poisoning. Legalislation of abortion on request is a necessary but insufficient step toward improving women’s health; in some countries, such as India, where abortion has been legal for decades, access to competent care remains restricted because of other barriers. Access to safe abortion improves women’s health, and vice versa, as documented in Romania during the regime of President Nicolae Ceausescu. The availability of modern contraception can reduce but never eliminate the need for abortion. Direct costs of treating abortion complications burden impoverished health care systems, and indirect costs also drain struggling economies. The development of manual vacuum aspiration to empty the uterus, and the use of misoprostol, an oxytocic agent, have improved the care of women. Access to safe, legal abortion is a fundamental right of women, irrespective of where they live. The underlying causes of morbidity and mortality from unsafe abortion today are not blood loss and infection but, rather, apathy and disdain toward women.
- p. 1908
- Worldwide, an estimated 68 000 women die as a result of complications from unsafe induced abortions every year—about eight per hour. This prevalence translates into an estimated case-fatality rate of 367 deaths per 100 000 unsafe abortions, which is hundreds of times higher than that for safe, legal abortion in developed nations.
- p. 1910
- Nearly 5000 years ago, the Chinese Emperor Shen Nung described the use of mercury for inducing abortion. Although one publication lists over 100 traditional methods used for inducing abortion, unsafe methods today can be divided into several broad classes: oral and injectable medicines, vaginal preparations, intrauterine foreign bodies, and trauma to the abdomen (panel 2). In addition to detergents, solvents, and bleach, women in developing countries still rely on teas and decoctions made from local plant or animal products, including dung. Foreign bodies inserted into the uterus to disrupt the pregnancy often damage the uterus and internal organs, including bowel. In settings as diverse as the South Pacific and equatorial Africa, abortion by abdominal massage is still used by traditional practitioners. The vigorous pummelling of the woman’s lower abdomen is designed to disrupt the pregnancy but sometimes bursts the uterus and kills the woman instead.
- p.1911
- Increasing legal access to abortion is associated with improvement in sexual and reproductive health. Conversely, unsafe abortion and related mortality are both highest in countries with narrow grounds for legal abortion.33 More than 61% of the world’s population resides in countries where induced abortion is allowed without restriction or for a wide range of reasons such as protection of the woman’s life, preservation of her physical or mental health, and socioeconomic grounds.34 In 72 countries, most of which are in the developing world, 26% of the world’s population lives where abortion is prohibited altogether or allowed only to save the woman’s life.34 Most of these restrictive laws originated from European colonial laws from previous centuries, although the European nations discarded their restrictive abortion laws decades ago.
- p.1911
- The prevalence of unsafe abortions remains the highest in the 82 countries with the most restrictive legislations, up to 23 unsafe abortions per 1000 women aged 15–49 years. By contrast, the 52 countries that allow abortion on request have a median unsafe abortion rate as low as two per 1000 women of reproductive age.33 Although the case-fatality rate from unsafe abortions indicates the general level of health care and the availability of post-abortion services, the rate remains the highest in countries where abortion is legally restricted. In such countries, the median ratio for unsafe abortion mortality is 34 deaths per 100 000 livebirths; this ratio steadily decreases as legal grounds for abortion increase. The ratio falls to one or less per 100 000 livebirths in countries that allow abortion on request.33 Even in countries where improved access to health care and emergency obstetric services has greatly reduced overall maternal mortality, restrictive abortion laws translate into abortion deaths constituting a disproportionately high share of maternal deaths.
Making abortion legal, safe, and accessible does not appreciably increase demand. Instead, the principal effect is shifting previously clandestine, unsafe procedures to legal and safe ones. Hence, governments need not worry that the costs of making abortion safe will overburden the health-care infrastructure. Countries that liberalised their abortion laws such as Barbados, Canada, South Africa, Tunisia, and Turkey did not have an increase in abortion. By comparison, the Netherlands, which has unrestricted access to free abortion and contraception, has one of the lowest abortion rates in the world.- p.1913
- The indirect costs of unsafe abortion are substantial, yet more difficult to quantify. They include the loss of productivity from abortion-related morbidity and mortality on women and household members; the effect on children’s health and education if their mother dies; the diversion of scarce medical resources for treatment of abortion complications; and secondary infertility, stigma, and other sociopsychological consequences. For example, an estimated 220 000 children worldwide lose their mothers every year from abortion-related deaths. Such children receive less health care and social care than children who have two parents, and are more likely to die.
- p.1914
- Primary prevention includes reduction in the need for unsafe abortion through contraception, legalisation of abortion on request, the use of safer techniques, and improvement of provider skills. Access to safe, effective contraception can substantially reduce—but never eliminate–the need for abortion to regulate fertility. The effect of national contraceptive programmes on reducing the rate of abortion is well documented. In seven countries (Bulgaria, Kazakhstan, Kyrgyzstan, Switzerland, Tunisia, Turkey, and Uzbekistan), abortion rates fell as use of modern contraception rose. In another six countries (Cuba, Denmark, Netherlands, Republic of Korea, Singapore, and USA), abortion and contraception increased simultaneously; the uptake of effective contraception did not keep pace with couples’ increasing desires for smaller family sizes. In several of the six countries, abortion rates ultimately declined with continued contraceptive use and stabilisation of fertility rates at lower levels. Even with high rates of contraceptive use, however, unintended pregnancies will continue. No contraceptive method is 100% effective, and many couples in the developing world still encounter obstacles to contraception. Every year, 80 million women worldwide have an unintended pregnancy, and 60% of these are aborted. Thus, the need for safe abortion will continue. The developing world has seen a revolution in contraceptive use—from a mere 9% of couples using any method in 1960–6565 to 59% in 2003. Nevertheless, an estimated 27 million unintended pregnancies happen worldwide every year with the typical use of contraceptives. Six million would happen even with perfect (i.e., correct and consistent) use. An estimated 123 million women have an unmet need for family planning.
- p.1914
- The public health rationale to address unsafe abortion was first drawn to attention by the World Health Assembly four decades ago. In 1994, the Programme of Action of the International Conference on Population and Development stated, “In circumstances where abortion is not against the law, such abortion should be safe.” The Report of the Fourth World Conference on Women, held in Beijing in 1995, noted “unsafe abortions threaten the lives of a large number of women, representing a grave public health problem as it is primarily the poorest and youngest who take the highest risk”. At the Special Session of the UN General Assembly in June, 1999, governments agreed that “in circumstances where abortion is not against the law, health systems should train and equip health-service providers and should take other measures to ensure that such abortion is safe and accessible”. By investing in abortion safety and availability, governments throughout the world can save the lives of tens of thousands of women every year.
- p.1917
- Unsafe abortion endangers health in the developing world, and merits the same dispassionate, scientific approach to solutions as do other threats to public health. Although the remedies are available and inexpensive, governments in developing nations often do not have the political will to do what is right and necessary. The beneficiaries of access to safe, legal abortion on request include not only women but also their children, families, and society—for present and future generations. Women have always had abortions and will always continue to do so, irrespective of prevailing laws, religious proscriptions, or social norms. Although the ethical debate over abortion will continue, the public-health record is clear and incontrovertible: access to safe, legal abortion on request improves health. As noted by Mahmoud Fathalla, “Pregnancy-related deaths ... are often the ultimate tragic outcome of the cumulative denial of women’s human rights. Women are not dying because of untreatable diseases. They are dying because societies have yet to make the decision that their lives are worth saving.” Simply put, they die because they do not count.
- p.1917
"Unsafe abortion: unnecessary maternal mortality" (2009)
[edit]Haddad LB, Nour NM (2009). "Unsafe abortion: unnecessary maternal mortality". Reviews in Obstetrics & Gynecology. 2 (2): 122–126. PMC 2709326. PMID 19609407.
- Every year, worldwide, about 42 million women with unintended pregnancies choose abortion, and nearly half of these procedures, 20 million, are unsafe. Some 68,000 women die of unsafe abortion annually, making it one of the leading causes of maternal mortality (13%). Of the women who survive unsafe abortion, 5 million will suffer long-term health complications. Unsafe abortion is thus a pressing issue. Both of the primary methods for preventing unsafe abortion—less restrictive abortion laws and greater contraceptive use—face social, religious, and political obstacles, particularly in developing nations, where most unsafe abortions (97%) occur. Even where these obstacles are overcome, women and health care providers need to be educated about contraception and the availability of legal and safe abortion, and women need better access to safe abortion and postabortion services. Otherwise, desperate women, facing the financial burdens and social stigma of unintended pregnancy and believing they have no other option, will continue to risk their lives by undergoing unsafe abortions.
- According to the World Health Organization (WHO), every 8 minutes a woman in a developing nation will die of complications arising from an unsafe abortion. An unsafe abortion is defined as “a procedure for terminating an unintended pregnancy carried out either by persons lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both.”1 The fifth United Nations Millennium Development Goal recommends a 75% reduction in maternal mortality by 2015. WHO deems unsafe abortion one of the easiest preventable causes of maternal mortality and a staggering public health issue.
- Obtaining accurate data for abortions is challenging, and especially so for unsafe abortion. Two-thirds of nations do not have the capacity to collect data, and data collection varies from country to country in both quantity and quality. Because unsafe abortion is often done clandestinely by untrained individuals or by the pregnant women themselves, much of it goes undocumented; figures are therefore estimates. Data suggest that even as the overall abortion rate has declined, the proportion of unsafe abortion is on the rise, especially in developing nations. From 1995 to 2003, the overall number of abortions declined, but the unsafe abortion rate was steady (from 15 to 14 abortions per 1000 women, respectively), constituting an increase from 44% to 48%.
In Western nations, only 3% of abortions are unsafe, whereas in developing nations 55% are unsafe. The highest incidences of abortions that are unsafe occur in Latin America, Africa, and South East Asia (Figure 1). - Even safe abortion in developing nations carries risks that depend on the health facility, the skill of the provider, and the gestational age of the fetus. With unsafe abortion, the additional risks of maternal morbidity and mortality depend on what method of abortion is used, as well as on women’s readiness to seek postabortion care, the quality of the facility they reach, and the qualifications (and tolerance) of the health provider. Methods of unsafe abortion include drinking toxic fluids such as turpentine, bleach, or drinkable concoctions mixed with livestock manure. Other methods involve inflicting direct injury to the vagina or elsewhere—for example, inserting herbal preparations into the vagina or cervix; placing a foreign body such as a twig, coat hanger, or chicken bone into the uterus; or placing inappropriate medication into the vagina or rectum. Unskilled providers also improperly perform dilation and curettage in unhygienic settings, causing uterine perforations and infections. Methods of external injury are also used, such as jumping from the top of stairs or a roof, or inflicting blunt trauma to the abdomen.
- Worldwide, some 5 million women are hospitalized each year for treatment of abortion-related complications such as hemorrhage and sepsis, and abortion-related deaths leave 220,000 children motherless. The main causes of death from unsafe abortion are hemorrhage, infection, sepsis, genital trauma, and necrotic bowel. Data on nonfatal long-term health complications are poor, but those documented include poor wound healing, infertility, consequences of internal organ injury (urinary and stool incontinence from vesicovaginal or rectovaginal fistulas), and bowel resections. Other unmeasurable consequences of unsafe abortion include loss of productivity and psychologic damage.
The burden of unsafe abortion lies not only with the women and families, but also with the public health system. Every woman admitted for emergency postabortion care may require blood products, antibiotics, oxytocics, anesthesia, operating rooms, and surgical specialists. The financial and logistic impact of emergency care can overwhelm a health system and can prevent attention to be administered to other patients. - Abortion laws have a spectrum of restrictiveness. Nations may allow abortions based on saving the mother’s life, preserving physical and mental health, and socioeconomic grounds, or may be completely unrestrictive. Data indicate an association between unsafe abortion and restrictive abortion laws. The median rate of unsafe abortions in the 82 countries with the most restrictive abortion laws is up to 23 of 1000 women compared with 2 of 1000 in nations that allow abortions. Abortion-related deaths are more frequent in countries with more restrictive abortion laws (34 deaths per 100,000 childbirths) than in countries with less restrictive laws (1 or fewer per 100,000 childbirths).
- The same correlation appears when a given country tightens or relaxes its abortion law. In Romania, for example, where abortion was available upon request until 1966, the abortion mortality ratio was 20 per 100,000 live births in 1960. New legal restrictions were imposed in 1966, and by 1989 the ratio reached 148 deaths per 100,000 live births. The restrictions were reversed in 1989, and within a year the ratio dropped to 68 of 100,000 live births; by 2002 it was as low as 9 deaths per 100,000 births. Similarly, in South Africa, after abortion became legal and available on request in 1997, abortion-related infection decreased by 52%, and the abortion mortality ratio from 1998 to 2001 dropped by 91% from its 1994 level.
- Less restrictive abortion laws also do not guarantee safe abortions for those in need; better education and access to health care are also required. In India, unsafe illegal abortions persist despite India’s passage of the Medical Termination of Pregnancy Act in the early 1970s. The act appeared to remove legal hindrances to terminating pregnancies in the underfunded (national) health care system, but women still turn to unqualified local providers for abortion. Clearly, the implications of the law never reached the population that most needed to rely on it. This example is also seen in Cambodia, where abortion is legally available on request and women often attempt to abort themselves before turning to hospital.
- More than one-third of all pregnancies are unintended, and 1 in 5 ends in abortion. In developing countries, two-thirds of unintended pregnancies occur among women who were not using any method of contraception. Greater contraceptive access and use alone can thus drastically reduce safe and unsafe abortion by reducing unintended pregnancies.
- In nations where abortion is legal, providing women better access to health centers that perform abortions is imperative. Practitioners need to become better trained in safer abortion methods and be able to transfer patients to a medical facility that is capable of providing emergency care when a complication arises. WHO strongly advises that all health facilities that treat women with incomplete abortions have the appropriate equipment and trained staff needed to ensure that care is consistently available and provided at a reasonable cost. In addition, postabortion family planning counseling needs to be an integral part of the service.
Evidence demonstrates that liberalizing abortion laws to allow services to be provided openly by skilled practitioners can reduce the rate of abortion-related morbidity and mortality. However, sociopolitical and religious obstacles have and will continue to play a role in passing abortion laws. The roles of research, grassroots organizations, health providers, activists, and media are vital in highlighting the importance of relaxing abortion laws. The emotional, physiologic, and financial cost on women and families, as well as the burden on the economic health system, should no longer be ignored. - Main Points
The World Health Organization deems unsafe abortion one of the easiest preventable causes of maternal mortality.
Data suggest that even as the overall abortion rate has declined, the proportion of unsafe abortion is on the rise.
Methods of unsafe abortion include drinking toxic fluids; inflicting direct injury to the vagina, cervix, or rectum; or inflicting external injury to the abdomen. Complications also arise from unskilled providers causing uterine perforation and infections.
Worldwide, 5 million women are hospitalized each year for treatment of abortion-related complications, and abortion-related deaths leave 220,000 children motherless.
Data indicate an association between unsafe abortion and restrictive abortion laws.
Preventing unintended pregnancy, providing better access to health care, and liberalizing abortion laws to allow services to be openly provided can reduce the rate of abortion-related morbidity and mortality.
“Unintended pregnancy and pregnancy outcome: equity and social determinants” (2010)
[edit]Shawn Malarcher, L.G. Olson and Norman Hearst; “Unintended pregnancy and pregnancy outcome: equity and social determinants”, Blas E, Kurup AS, eds. (2010). “Equity, social determinants and public health programmes”. World Health Organization.
- Worldwide, 40% of all pregnancies are unintended. Comparison of desired family size to actual fertility demonstrates that, in almost all countries, the burden of unintended pregnancy disproportionately affects the poor. Other disadvantaged groups that have higher rates of unintended pregnancy in many settings include young people, the uneducated, ethnic minorities and migrants.
Women with an unintended pregnancy may be faced with a choice between terminating the pregnancy or an unwanted birth. Unsafe abortion accounts for 13% of maternal deaths worldwide, and disadvantaged women are less likely to have access to safe abortion services and to proper care to treat complications. Poor women also suffer disproportionate consequences of unwanted childbearing, including health and social consequences for themselves and their children. Vulnerability to unintended pregnancy is strongly influenced by access to and use of effective contraception and by exposure to unwanted sex through child marriage and sexual violence. These all have strong social determinants.- p.178
- Several procedures are currently available to assist women with safe termination of pregnancy. Expansion of safe induced abortion services into remote and rural areas is possible largely as a result of advances in medical technologies, which have reduced cost and simplified procedures. Complication rates for these procedures are extremely low, with almost all abortion-attributable morbidity and mortality resulting from untrained providers, use of harmful procedures or failure to use appropriate infection prevention procedures. “Unsafe abortion” is defined as a procedure for terminating pregnancy carried out by attendants without appropriate skills, or in an environment that does not meet minimum standards for the procedure, or both. Unsafe abortion is a major cause of maternal mortality, accounting for an estimated 13% of maternal deaths worldwide. The highest estimated rate of unsafe abortion is in Latin America and the Caribbean, where there are 33 unsafe abortions per 100 live births, followed by Africa (17 per 100 live births) and Asia (13 per 100 live births)¬.
- p.182
- In 2005, an estimated 5 million women were hospitalized for treatment of complications from unsafe abortion. Rates of unsafe abortion are highest among young women, with almost 60% of unsafe abortions in Africa occurring among women under age 25. A number of studies have documented higher complication rates and mortality resulting from unsafe abortion among women of low socioeconomic status. Factors that contribute to observed differentials in abortion complications include the health status of women, longer delay in seeking induced abortion, use of less skilled providers, use of more dangerous methods and longer delay in seeking care for complications. Figure 10.2 illustrates the differences in care-seeking behaviour among women of varying socioeconomic status. Women from more affluent households are more likely to obtain an induced abortion from a physician or nurse, while poor women living in rural areas are more likely to use a traditional practitioner or self-induce an abortion.
Women report that socioeconomic concerns are a primary consideration in deciding whether to seek an induced abortion. Poorer women and adolescents are less likely to have the financial resources; less likely to have the knowledge of when, where and from whom to seek an induced abortion; or lack the social support to secure safe abortion services.- p.182
- The principal social determinant of recourse to unsafe abortion is real or perceived legal restriction on safe abortion. Developing countries are much more likely to restrict access to legal abortion than developed countries, and the restrictions disproportionately affect poorer women. While abortion is allowed to preserve women’s physical or mental health in 86% of developed countries, only 55% of developing countries allow this. Many conditions that make pregnancy dangerous, however, such as valvular heart disease, are more common in developing countries and more common among poorer women within those countries, and women in those countries and poorer women within them are less likely to have access to effective treatment. Affected women are then forced to make an invidious choice between a high-risk pregnancy and an unsafe abortion.
Outcomes are much worse for women who lack access to safe abortion. Safe abortion may be available to some women even where abortion is illegal. Studies of abortion providers in contexts where abortion was heavily restricted by law show that higher income, urban women were more likely to receive safe abortion than poor, rural women. Widespread access to safe abortion generally requires a context in which abortion is legal. But while criminalization of abortion promotes unsafe abortion, unsafe abortion should not be equated with illegal abortion. Legal abortions – like any other medical procedure – may be unsafe where clinicians are poorly trained or facilities are inadequate. Some countries in which abortion is legal for most indications continue to have high rates of unsafe abortion. India and South Africa are countries where high rates of unsafe abortion persist despite changes in the law that should make safe abortion readily available. Contributing factors include cost, procedural and bureaucratic delays, inadequate numbers of trained practitioners to meet demand and concerns about confidentiality for women below the age of majority.- pp.182–183.
- The medical factors that influence vulnerability to mortality and morbidity after unsafe abortion are the method used and the care received in the event of complications such as sepsis. Where a reasonable standard of hospital care is available, mortality should be low, and the cost of care is relatively modest – US$ 8.51 for drugs and equipment, according to the United Nations Population Fund (UNFPA).
The risk of death after an unsafe abortion varies widely. In developed countries, the mortality rate of unsafe abortion is much higher than that of legal abortion (in the United States the mortality of legal abortion is 0.6/100 000 procedures, but in developed countries the mortality of unsafe abortion averages 10/100 000 procedures). But this is low compared to rates in developing countries, and since legal abortion is more likely to be available in developed countries and thenumber of unsafe abortions in these countries is low, the number of deaths from unsafe abortion is tiny. In Latin America, the case fatality rate is also relatively low at about 50/100 000 unsafe abortions; despite the high incidence of unsafe abortion in this region, relatively few deaths result (less than 3% of the world total). In sub-Saharan Africa the mortality rate is 750/100 000 unsafe abortions. Although this region accounts for less than one quarter of the world’s unsafe abortions, it accounts for over half of the resulting deaths.- p.183
- Social determinants play a key role in both unintended pregnancy and pregnancy outcome. Women from disadvantaged social circumstances are more likely to experience an unintended pregnancy than women with greater financial and social resources. When faced with an unwanted pregnancy, women with less means are also more likely to face more severe consequences from an unsafe abortion or an unwanted birth than more advantaged women. These disparities in unintended pregnancy and its consequences are the result of social, political and economic systems that do not provide access to correct knowledge of sexual and reproductive health and to necessary services.
- p.189
- Poor women are especially vulnerable because they are less likely to deliver under the care of a skilled birth attendant, sometimes resulting in rates of maternal morbidity and mortality orders of magnitude higher than for richer women. Even when they do have skilled birth attendance, they may still suffer from differential outcomes of care because not all “skilled” birth attendants have the same level of skill or the same access to hospital back-up when complications arise. For women who choose not to keep an unwanted pregnancy, the lack of access to safe abortion services can also increase risk by orders of magnitude.
- p.189
- The number of unsafe abortions can be reduced by decreasing the number of unintended pregnancies or by increasing access to safe abortion. The most effective means of reducing the overall number of abortions (safe and unsafe) is to decrease the number of unintended pregnancies by increasing use of modern contraception. Changes in legislation that liberalize access to safe induced abortion services have substantial effects on women’s health, as demonstrated by recent experience in Romania and South Africa. After the introduction of restrictive abortion policy in 1966, Romania saw an increase in abortion-attributable mortality. By 1989, mortality rates had risen sevenfold and abortion accounted for 87% of maternal deaths. Reversal of the law in 1989 coincided with a drop in mortality by more than half within the first year and by 2002 the mortality rate had been reduced to 9 per 100 000 live births. South Africa has experienced a similar trend with a 91% drop in abortion-related deaths from 1994 to 1998/2001 after the Choice on Termination of Pregnancy Act went into effect in 1997.
- p.190
- In the absence of programmatic effort to expand services, legislation alone may not lead to such dramatic improvements. Even where safe abortion is not legally restricted, high-quality services may not be widely accessible or providers’ skills and methods may be inadequate. In the United States, for example, where abortion is legal, 34% of women (mostly in rural areas) live in regions with no abortion provider.
- p.190
- Countries unwilling for whatever reason to legalize safe abortion should at least consider a policy of harm minimization. The legal basis for harm minimization is removal of penalties for a woman who has an abortion, as prefigured in the 1995 Beijing Platform for Action on the human rights of women, to which most WHO Member States are signatories. In harm minimization programmes, women who have decided to have an illegal abortion are steered towards less unsafe methods of abortion and followed up to ensure identification and treatment of complications. Such programmes are simple to mount and effective.
- p.190
"An introduction to maternal mortality" (2008)
[edit]Nour NM (2008).[ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2505173/ "An introduction to maternal mortality"]. Reviews in Obstetrics & Gynecology. 1 (2): 77–81. PMC 2505173. PMID 18769668.
- Every minute a woman dies during labor or delivery. The highest maternal mortality rates are in Africa, with a lifetime risk of 1 in 16; the lowest rates are in Western nations (1:2800), with a global ratio of 400 maternal deaths per 100,000 live births. The main causes of death are postpartum hemorrhage (24%); indirect causes such as anemia, malaria, and heart disease (20%); infection (15%); unsafe abortion (13%); eclampsia (12%); obstructed labor (8%); and ectopic pregnancy, embolism, and anesthesia complications (8%). Forty-five percent of postpartum deaths occur within the first 24 hours and 66% occur during the first week. Of the estimated 211 million pregnancies, 46 million result in induced abortions. Sixty percent of these abortions are unsafe and cause 68,000 deaths annually.
- The consensus among international organizations is that quality care requires services throughout a woman’s reproductive life. These organizations design programs that focus on improving outcome during the intrapartum/postpartum period, offering family planning services, providing safe abortions, and increasing antepartum care.
- Donors, UN organizations, and governments have made great strides in promoting family planning and contraceptive use. Due to this effort, millions of maternal deaths have been prevented. However, contraceptive use in many resource-poor nations is still not at optimal levels. The overall lack of contraceptive access rate is 50%, with a low of 4% in Europe and high of 57% in countries in Africa. This lack of access to contraception leads to unwanted pregnancies, increased demand for abortions, and deaths related to unsafe abortions. Measuring maternal mortality requires that the mother be pregnant, so prevention of pregnancy makes it difficult to quantify how many deaths have been prevented. Nevertheless, if unwanted pregnancies are prevented, data suggest that between 25% to 40% of maternal deaths could be eliminated.
- Given the high rate of maternal death due to unwanted pregnancies, some countries, such as South Africa, Tunisia, and Cape Verde, are recognizing the importance of developing wider access to safe abortions. In countries such as Mali, Sudan, Benin, and Burkina Faso, where legally, politically, and culturally access to abortion creates internal dispute, governments have allowed women access to safe abortions under specific circumstances, such as in cases of rape or fetal malformation. There are still some countries where women’s access to safe abortions is nonexistent and medical communities face resistance when advocating policy change. Women who seek help may be ostracized.
"Abortion and maternal mortality in the developing world" (2006)
[edit]Okonofua, F. (2006). "Abortion and maternal mortality in the developing world" (PDF). Journal of Obstetrics and Gynaecology Canada. 28 (11): 974–79. doi:10.1016/S1701-2163(16)32307-6. PMID 17169222. Archived from the original (PDF) on 11 January 2012.
- Unsafe abortion is an important public health problem, accounting for 13% of maternal mortality in developing countries. Of an estimated annual 70 000 deaths from unsafe abortion worldwide, over 99% occur in the developing countries of sub-Saharan Africa, Central and Southeast Asia, and Latin America and the Caribbean. Factors associated with increased maternal mortality from unsafe abortion in developing countries include inadequate delivery systems for contraception needed to prevent unwanted pregnancies, restrictive abortion laws, pervading negative cultural and religious attitudes towards induced abortion, and poor health infrastructures for the management of abortion complications. The application of a public health approach based on primary, secondary, and tertiary prevention can reduce morbidity and mortality associated with unsafe abortion in developing countries. Primary prevention includes the promotion of increased use of contraception by women (and by men) at risk for unwanted pregnancy; secondary prevention involves the liberalization of abortion laws and the development of programs to increase access to safe abortion care in developing countries. In contrast, tertiary prevention includes the integration and institutionalization of post-abortion care for incomplete abortion and the early and appropriate treatment of more severe complications of abortion. Efforts to address these problems will contribute both to reducing maternal mortality associated with induced abortion and to achieving the Millennium Development Goals in developing countries.
- p.974
- Induced and unsafe abortion is a critical public health problem and an important cause of maternal mortality in developing countries. Worldwide, of the 600 000 maternal deaths from pregnancy-related causes each year, an estimated 13% are attributable to complications of induced and unsafe abortion. Many of these deaths occur in developing countries where abortion laws are often restrictive and access to safe abortion is largely denied to women with unwanted pregnancies. Abortion-related deaths are hundreds of times more common in Latin America, sub- Saharan Africa, and Southeast and south Central Asia than in more developed regions of the world, where women have better access to safe abortion practices and procedures. The World Health Organization (WHO) estimates that in developing countries, 67 500 women die from abortion complications each year; in developed countries, 300 die each year.
- p.974
- Abortion is a largely preventable source cause of maternal mortality. Technologies and skills to prevent unwanted pregnancies and unsafe abortion are generally available in both developed and some developing countries. A recent World Bank analysis indicates that 90% of abortion-related mortality could be reduced simply by providing safe abortion care. However, lack of political will and lack of resources to apply these technologies are responsible for the high rate of maternal mortality associated with induced abortion in developing countries. Abortion mortality almost exclusively affects women in developing countries, and it is the disadvantaged, poor, and rural women in these countries who are most affected.
- p.975
- Abortion is highly restricted in many parts of the developing world. Of the 107 countries around the world that either prohibit or strongly restrict access to legal abortion services, the only industrialized countries are Poland and the Republic of Ireland. The rest are developing and low-income countries in Africa, Southeast and Central Asia, and South America and the Caribbean. Abortion laws in developing countries were derived from laws of European colonizers; however, although these European countries (notably Britain, France, Portugal, and Spain) have modernized their laws, many of the colonized countries have continued to maintain the old laws despite years of independence. Contrary to their intended purpose, however, restrictive laws have not prevented abortion in these countries; instead the laws have criminalized women and driven the practice of abortion underground, making it unsafe for women.
- p.976
- In many developing countries, because of restrictive abortion laws, termination of pregnancy is undertaken either by women themselves, using highly dangerous methods, or by “backstreet” abortionists lacking minimal training, skills, and experience. The consequence is a high rate of associated complications that result in mortality. Data indicate that more than 30% of women seeking termination of pregnancy in countries with restrictive abortion laws may experience moderate to severe complications.
- p.976
- In Zambia and Ghana, two countries in Africa with liberal abortion laws, the lack of strong service delivery systems that integrate abortion and post-abortion care is the major reason that women in those countries still suffer complications of unsafe abortion. Women, and many providers, in these countries are not even familiar with opportunities provided under the law to terminate unwanted pregnancies safely, and policymakers do not regularly provide and disseminate clear guidelines and procedures for abortion and post-abortion care. In Indonesia, the negative attitudes of providers often prevent women from seeking menstrual regulation approved by the Ministry of Health. These negative attitudes by health providers are also carried over to women who suffer complications of induced abortion and
- pp.976-977
- The continued low contraceptive prevalence rates in developing countries account for the high rate of unwanted pregnancies that lead to unsafe and induced abortion-related mortality. Data from the United Nations Population Fund (UNFPA) indicate that the prevalence of modern contraceptive use is currently around 55% for Asia, 49% for Latin America and the Caribbean, and only 15% for sub-Saharan Africa, with large unmet needs for contraception in many of these countries.
- p.977
- Pregnancies can now be terminated using eminently safe methods such as manual vacuum aspiration (MVA) and mifepristone and misoprostol regimens. Programs that aim to reduce abortion mortality must teach the appropriate use of these methods to physicians and to mid-level providers such as nurses and midwives, as has been done in Ghana and South Africa, to decentralize the use of these methods for the effective secondary prevention of abortion mortality. Programs to integrate the teaching of these methods into medical, midwifery, and nursing curricula are also useful and should be pursued in developing countries.
- p.977
- The most common complication of unsafe abortion in developing countries is incomplete abortion. There is now incontrovertible evidence that MVA is more cost-effective and safer than traditional dilatation and curettage (D&C) in treating incomplete abortion in developing countries. MVA used as part of post-abortion care has found increasing acceptability among health workers, health administrators, and policymakers in developing countries. However, many countries are still grappling with several issues relating to its provision, including key aspects of clinical care, information, and counselling, the extent to which MVA use can be decentralized to mid-level providers, the cost of services, and the provision of post-abortion family planning to women with incomplete abortion. The extent to which these related issues are resolved in each country will determine the extent to which post-abortion care can contribute to reducing abortion-related maternal mortality in developing countries in the coming years.
- p.978
- The application of a public health approach based on primary, secondary, and tertiary prevention can reduce morbidity and mortality associated with unsafe abortion in developing countries. Primary prevention includes the promotion of increased use of contraception by women at risk of unwanted pregnancy. Secondary prevention involves the liberalization of abortion laws and programs to increase women’s access to safe abortion care in developing countries. Tertiary prevention includes the integration and institutionalization of post-abortion care for incomplete abortion and the early and appropriate treatment of more severe complications of abortion. Efforts to address these problems will contribute to reducing maternal mortality associated with induced abortion and to achieving the MDGs in developing countries
- p.978
“Freedom of Choice: A Youth Activist’s Guide to Safe Abortion Advocacy” (January 2013)
[edit]Rinaldi Ridwan, Rachel Jacobson, Nida Mushtaq, Kokou Sename Djagadou, Clara Fok, Oriana Lopez Uribe, of Choice: A Youth Activist’s Guide to Safe Abortion Advocacy”, Youth Coalition for Sexual and Reproductive, (January 2013)
- The facts speak for themselves:
* Two-thirds of all unsafe abortions are sought by women under the age of 30.
* Adolescent girls (aged 10-19) account for 70% of hospitalizations from unsafe abortion complications.
* Adolescents and young women aged 15-24 account for 40% of all unsafe abortions worldwide and three million unsafe abortions occur every year among this age group.- p.1
- Over the past several years, the issue of maternal mortality has begun to receive the funding and political attention that it deserves. Still, one of the main causes of maternal death has not garnered as much support and has, in fact, often been ignored in the broader maternal health movement: unsafe abortion.
The legal status of abortion in a given country is a key determinant of young women’s access to abortion care; the legal status of abortion in less progressive countries are more restrictive with qualifiers that often deny young women and girls the agency they need to decide on their bodily integrity in accessing such services. Very general laws on abortion often hide the very real obstacles women, especially young women, face in accessing care. Even in countries where abortion is technically legal or decriminalized, young women may still be unable to access abortion care. For example, mandatory waiting periods, parental or spousal consent laws, lack of public funding, lack of information on safe abortion and stigma, all work to limit young women’s access to abortion care.- p.1
- While women living in countries with less restrictive abortion laws have more access to safe abortion services and information, unsafe abortions (including self-induced abortions) are notably high in countries with more restrictive laws. Countries in Western Europe have some of the most liberal abortion laws and the lowest rates of abortion and maternal mortality due to abortion. Countries in Eastern Europe have the highest rates of abortion and some of the most restrictive laws compared to the rest of the region and other similar countries.
- p.4
- Countries with laws that permit abortion upon request do not ask the woman to qualify her decision. In these countries, women must only and a physician that is willing to perform the abortion; however, in many countries with the most liberal abortion laws, gestational time limits are imposed, often making abortion available only in the first trimester. After this time, a woman must present what is considered a valid reason for terminating her pregnancy. Even if a country has laws and policies that allow abortion under any circumstance, this does not mean that the government will take the responsibility to ensure that safe abortion care is accessible or available.
- pp.7-8
- In addition to the legal issues, access to safe abortion is often complicated by many other socioeconomic obstacles on the part of the State or their unwillingness to invest resources into providing safe, available, accessible and affordable abortion that is free from stigma and discrimination.
- p.8
- Kenya relaxed its abortion laws in the 2010 constitution by giving health professionals more leeway in determining when abortion is permitted but the rate of 48 abortions for every 1,000 women – highest in Africa and mostly unsafe – persists. Absence of health infrastructure support for abortion care and widespread stigma against women seeking abortion are two major obstacles in providing safe abortion for women.
- p.8
- Abortion related stigma is one of the most difficult obstacles to tackle and requires a complete shift in community behaviour and attitude. Many families and service providers guilt women seeking abortion by pushing cultural stereotypes around gender and reproductive roles onto women. In such situations, women are forced to carry an unwanted pregnancy or resort to an illegal – often unsafe – abortion, even where liberal laws exist. This has been the case in Nepal, a country that is globally applauded for its most liberal laws in contrast to its regional counterparts in South Asia as well as the Global South.
- pp.8-9
"Legal or Not, Abortion Rates Compare" (October 11, 2007)
[edit]Elisabeth Rosenthal (October 11, 2007). "Legal or Not, Abortion Rates Compare". New York Times.
- A comprehensive global study of abortion has concluded that abortion rates are similar in countries where it is legal and those where it is not, suggesting that outlawing the procedure does little to deter women seeking it.
Moreover, the researchers found that abortion was safe in countries where it was legal, but dangerous in countries where it was outlawed and performed clandestinely. Globally, abortion accounts for 13 percent of women’s deaths during pregnancy and childbirth, and there are 31 abortions for every 100 live births, the study said. - “We now have a global picture of induced abortion in the world, covering both countries where it is legal and countries where laws are very restrictive,” Dr. Paul Van Look, director of the W.H.O. Department of Reproductive Health and Research, said in a telephone interview. “What we see is that the law does not influence a woman’s decision to have an abortion. If there’s an unplanned pregnancy, it does not matter if the law is restrictive or liberal.”
But the legal status of abortion did greatly affect the dangers involved, the researchers said. “Generally, where abortion is legal it will be provided in a safe manner,” Dr. Van Look said. “And the opposite is also true: where it is illegal, it is likely to be unsafe, performed under unsafe conditions by poorly trained providers.” - Anti-abortion groups criticized the research, saying that the scientists had jumped to conclusions from imperfect tallies, often estimates of abortion rates in countries where the procedure was illegal. “These numbers are not definitive and very susceptible to interpretation according to the agenda of the people who are organizing the data,” said Randall K. O’Bannon, director of education and research at the National Right to Life Educational Trust Fund in Washington.
He said that the major reason women die in the developing world is that hospitals and health systems lack good doctors and medicines. “They have equated the word ‘safe’ with ‘legal’ and ‘unsafe’ with ‘illegal,’ which gives you the illusion that to deal with serious medical system problems you just make abortion legal,” he said. - The study indicated that about 20 million abortions that would be considered unsafe are performed each year and that 67,000 women die as a result of complications from those abortions, most in countries where abortion is illegal.
- Some countries, like South Africa, have undergone substantial transitions in abortion laws in that time. The procedure was made legal in South Africa in 1996, leading to a 90 percent decrease in mortality among women who had abortions, some studies have found.
Abortion is illegal in most of Africa, though. It is the second-leading cause of death among women admitted to hospitals in Ethiopia, its Health Ministry has said. It is the cause of 13 percent of maternal deaths at hospitals in Nigeria, recent studies have found.
"Induced abortion: estimated rates and trends worldwide" (2007)
[edit]Sedgh G, Henshaw S, Singh S, Ahman E, Shah IH (2007). "Induced abortion: estimated rates and trends worldwide". Lancet. 370 (9595): 1338–45. doi:10.1016/S0140-6736(07)61575-X. PMID 17933648. S2CID 28458527.
- Unsafe and safe abortions correspond in large part with illegal and legal abortions, respectively. The findings presented here indicate that unrestrictive abortion laws do not predict a high incidence of abortion, and by the same token, highly restrictive abortion laws are not associated with low abortion incidence. Indeed, both the highest and lowest abortion rates were seen in regions where abortion is almost uniformly legal under a wide range of circumstances.
Results of previous studies have shown a strong correlation between abortion and contraception use such that, in settings with steady fertility rates over time, abortion incidence declines as contraceptive use increases. An analysis of trends in Eastern Europe and western and south-central Asia indicates that this pattern is evident in those regions.- p.1343
- [S]ome abortions in restricted settings are done by trained providers, but most abortions in these settings have high risks to a woman’s life and health. In Africa, where abortion is highly restricted by law in nearly all countries, there are 650 deaths for every 100 000 procedures, compared with fewer than 10 per 100 000 procedures in developed regions.18 Worldwide, an estimated 5 million women are hospitalised every year for treatment of complications related to unsafe abortion. Moreover, illegal procedures are harmful even when they do not lead to these consequences, because they require women to take actions in violation of the law and often without the knowledge or support of their partners or family.
- p.1344
- Worldwide, the rate of unsafe abortion declined slightly between 1995 and 2003, but the proportion of all abortions that were unsafe increased from 44% to 48% in the same interval. These findings reinforce the need to ensure that existing resources for reducing the rates of unsafe abortions are used as fully as possible. WHO has issued technical and policy guidance to assist countries in making safe abortion accessible to the full extent permitted by the law, which include: using the safe methods now available for first-trimester abortions, in particular manual and electric vacuum aspiration and medical abortion; training providers on safe and aseptic abortion practice; training mid-level health professionals to do these procedures to the extent allowed by law; ensuring that the needed equipment and supplies are available for safe and appropriate procedures; and providing high quality post-abortion care that includes contraceptive counselling and services.
- p.1344
"Unsafe abortion: global and regional incidence, trends, consequences, and challenges" (December 2009)
[edit]Shah, I; Ahman, E (December 2009). "Unsafe abortion: global and regional incidence, trends, consequences, and challenges" (PDF). Journal of Obstetrics and Gynaecology Canada. 31 (12): 1149–58. doi:10.1016/s1701-2163(16)34376-6. PMID 20085681. Archived from the original (PDF) on 16 July 2011.
- An estimated 70 000 women die each year because of complications of unsafe abortion; the recent killing of Dr George Tiller is a stark reminder that providers of abortion also suffer grave consequences. This trend persists against the backdrop of major advances in the medical profession, especially in terms of the availability of safe and effective technologies and skills for induced abortion. Unsafe abortion presents one of the most critical global public health and human rights challenges of the present times.
Each day 192 women die because of complications arising from unsafe abortion; that is one woman every eight minutes, nearly all of them in developing countries. These women are likely to have had little or no money to procure safe services; many of them are young, perhaps in their teens, living in rural areas and having little social support to deal with their unplanned pregnancy. Some of them have been raped, and some have experienced an accidental pregnancy due to the failure of the contraceptive method they were using or the incorrect or inconsistent way they used it. Some of them lacked knowledge of methods to prevent unintended pregnancy or did not have the means to obtain them. Some may have found contraceptive services hard to reach, while others may have been turned away by judgemental or insensitive providers. A large percentage of them may have first attempted to self-induce the abortion and failing that, they may have turned to an unskilled, but relatively inexpensive and affordable provider.- p.1150
- Among the 5 million women who are estimated to suffer temporary or permanent disability each year because of unsafe abortion, more than three million are likely to suffer from the effects of reproductive tract infections and 1.7 million are estimated to develop secondary infertility. Overall, some 24 million women are estimated to be currently suffering from secondary infertility due to an unsafe abortion.
- p.1155
- The public health impact of unsafe abortion has long been recognized. As early as 1967, the World Health Assembly identified unsafe abortion as a serious public health problem in many countries. Discussions that grew out of the1968 International Conference on Human Rights in Tehran culminated in the new concept of “reproductive rights,” which was subsequently highlighted at the 1994 International Conference on Population and Development (ICPD). ICPD established a number of goals and targets, including universal access to reproductive health services by 2015. On induced abortion, the ICPD consensus statement noted:
All Governments and relevant intergovernmental and non-governmental organizations are urged to strengthen their commitment to women’s health, to deal with the health impact of unsafe abortion as a major public health concern and to reduce there course to abortion through expanded and improved family-planning services....In circumstances where abortion is not against the law, such abortion should be safe. In all cases, women should have access to quality services for management of complications arising from abortion. Post-abortion counselling, education and family-planning services should be offered promptly, which will also help to avoid repeat abortion.- p.1155
- The Special Session of the United Nations General Assembly in June–July 1999 urged countries that “in circumstances where abortion is not against the law, health systems should train and equip health-service providers and should take other measures to ensure such abortion is safe and accessible.” The Reproductive Health Strategy of the WHO, approved in 2004, noted that “[a]s a preventable cause of maternal mortality and morbidity, unsafe abortion must be dealt with as part of the Millennium Development Goal on improving maternal health and other international development goals and targets.”
- p.1156
- Given the broad recognition of unsafe abortion as a serious public health problem, it should be easy to agree on strategies and policies for addressing it effectively. However, the discourse is diverse, ranging from views of abortion as a human right and a woman’s choice, to assertions that liberalizing abortion increases the incidence of abortion. Some-times it is suggested that abortion is a taboo topic in certain cultural, social, or religious contexts or that there could be a public backlash against liberalizing the restrictions. There-fore, inaction is put forth as the best course of action. Much of the discourse has continued to be devoid of scientific evidence and informed discussion.
- p.1157-1158
"Unsafe abortion: the global public health challenge" (April 27, 2009)
[edit]Iqbal H. Shah & Elisabeth Ahman, Chapter 2 “Unsafe abortion: the global public health challenge”, in Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD (eds.). “Management of unintended and abnormal pregnancy: comprehensive abortion care”. (April 27, 2009) Oxford: Wiley-Blackwell. ISBN 978-1-4051-7696-5.
- The World Health Organization (WHO) defines “unsafe abortion” as a procedure for terminating an unintended pregnancy either by individuals without the necessary skills or in an environment that does not conform to the minimum medical standards, or both. With the advent and expanding use of early medical abortion, this definition may need to be modified to incorporate standards appropriate to these less technical methods of pregnancy termination.
- p.18
- More than 60% of the world’s population lives in countries where induced abortion is allowed for a wide range of reasons. Nevertheless, some of these countries have a high incidence of unsafe abortion. Current estimates indicate that only 38% of women aged 15 to 44 years live in countries where abortion is legally available and where no evidence of unsafe abortion exists. A number of countries allow abortion ob broad grounds, but unsafe abortions still occur outside the legal framework. Abortion has been, for example,, legal on request in India since 1972; however, many women are unaware that safe and legal abortion is available. Even those who know of its legality may not have access to safe abortion because of poor quality of services and/or economic and social constraints. Reports also suggest that unsafe abortions may be increasing in several of the newly independent states, formerly part of Russia, as a result of increased fees and fewer services for legal abortions.
- p.18
- In 2003, about 3% of all women of reproductive age worldwide had an induced abortion. Overall, the number of induced abortions declined from 46 million in 1995 to 42 million in 2003. Most of the decline occurred in developed countries (10.0 million to 6.6 million), with little change evident in developing countries (35.5 million to 35 million).
Induced abortion rates are, however, surprisingly similar across regions. A woman’s likelihood of having an induced abortion is almost the same whether she lived in a developed country (26 per 1,000) or a developing country (29 per 1,000). The main difference is safety: abortion is primarily safe in the former and mostly unsafe in the latter. Latin America, which has some of the world’s most restrictive induced abortion laws, has the highest abortion rate (31 per 1,000), but other regions have similar rates: Africa and Asia (29), Europe (28) and North America (21), and Oceania (17). Induced abortion rates vary by subregion, however. Eastern Africa and South East Asia who a rate of 39 per 1,000 women, while other subregions in Africa and Asia exhibit rates between 22 and 28 per 1,000. The Caribbean and South America subregions have high rates of 35 and 33 per 1,000. However, the highest abortion rate remains in Eastern Europe (44 per 1,000). In Europe, most induced abortions are safe and legal and the abortion incidence has been low for decades. The abortion rate has fallen substantially in recent years in eastern Europe, as contraceptives have become increasingly available. Nevertheless, women continue to rely on induced abortion to regulate fertility to a greater extent in this region than elsewhere.- p.19
- The distinction among regions becomes more marked when one compares the incidence and proportion of safe and unsafe abortions. In 2003, 48% of all abortions worldwide were unsafe, and more than 97% of these unsafe abortions occurred in developing countries. In Africa and Latin America abortions are almost exclusively unsafe; so are almost 40% of abortions in Asia. Unsafe abortion is rare in Europe. Legal restrictions on abortions have little effect on women’s propensity to terminate an unintended pregnancy. Restrictions do however, lead to clandestine abortions, which, in turn, injure and kill many women.
- p.20
- Since 1990, WHO has been collecting data and estimating the incidence of unsafe abortion. However, estimating the magnitude of unsafe abortion is complex for several reasons. Induced abortion is generally stigmatized and frequently censured by religious teaching or ideologies, which makes women reluctant to admit to having had an induced abortion. Surveys show that underreporting occurs even where abortion is legal. This problem is exacerbated in settings where induced abortion is restricted and largely inaccessible, or legal but difficult to obtain. Little information is available on abortion practice in these circumstances, and abortions tend to be unreported or vastly underreported. Moreover, clandestine induced abortions may be misreported as spontaneous abortion (miscarriage). The language used to describe induced abortion reflects this ambivalence: terms include “induced miscarriage” (fausse couche provoquee), “menstrual regulation,” and “regulation of a delayed or suspended menstruation.” In spite of these challenges, estimates of the frequency of unsafe abortion can be made mainly by using hospital data on abortion complications or abortion data from surveys and validated against the legal context of induced abortion, contraceptive prevalence, and total fertility rate (the average number of children a woman is likely to by the end of her reproductive years). Globally, WHO estimates that some 19 to 20 million unsafe abortions occurred each year between 1993 and 2003. This figure has remained relatively constant despite an increase in contraceptive prevalence during the same period. Although the transition to low fertility with smaller families has become a norm in most countries, family planning has not been able to entirely meet the need of couples to regulate fertility.
- p.21
- Globally, an estimated 1 in 10 pregnancies ended in an unsafe abortion in 2003, giving a ratio of 1 unsafe abortion to about 7 live births. The unsafe abortion rates or ratios for each region are estimated by dividing the number of unsafe abortions in that region by the regional number of all women aged 15 to 44 years or by the regional number of live births respectively, in the same reference year.
- p.21
- Absolute numbers of unsafe abortions cannot be compared meaningfully across regions and subregions or over time because of differing size of populations at risk.
- p.29
- Unsafe abortion rates close to 30 per 1,000 women aged 15 to 44 years are seen in both Africa and Latin America and the Caribbean; however, because of the higher numbers of births, the unsafe abortion ratio for Africa is only hal f that for Latin America. According to recent estimates, the number of unsafe abortions in South America may have reached a peak and begun to decline. If Cuba, where abortion is legally available upon request, is excluded from the calculation, the rate for the Caribbean falls between that for Central America (25 per 1,000) and South America (33 per 1,0000). The range of estimates for Africa is wide: eastern Africa has the highest rate of any subregion, at 39 per 1,0000, whereas South Africa has among the lowest, at 18 per 1,000 (not counting legal abortions of 5 per 1,000 women). The 1996 law liberalizing abortion in South Africa has clearly reduced the number of unsafe abortions in the subregion. Half of all unsafe abortions take place in Asia; however, rates and ratios are generally lower. Only in South-East Asia are rates and ratios similar to those of Africa and Latin America. South-Central Asia has the highest number of unsafe abortions of any subregion, owing to the sheer size of its population.
- p.29
- The ratio of unsafe abortion generally ranges from 10 to 20 unsafe abortions per 100 births. However, when declining fertility results in fewer and fewer births without an accompanying major shift from unsafe abortion to modern contraceptive uptakes, ratios become high. Also, where the motivation is stronger to end an unwatned or unintended pregnancy through abortion rather than unwanted birth, the ratio would be higher. Such is the case in South America (38 per 100), Central America (26 per 100), the Caribbean (26 per 100) for all countries vs. 19 per 100 for countries at risk) and South-East Asia (31 per 100 for all countries vs. 27 per 100 for countries at risk).
- p.30
- The interpretation of trends in unsafe abortion ratios is not straightforward because it is a composite index of the degree of motivation to terminate an unwanted pregnancy by induced abortion as well as the trends in unsafe abortion relative to live births. With the increasing motivation to regulate fertility, the unsafe abortion ratio increases.
Notwithstanding the complex relationship between trends in fertility and trends in unsafe abortion ratios, two main patterns emerge. The first is represented by South America, and also includes Central America, the Caribbean, and South Africa, where fertility has decline to around 2.5 children per woman. South Africa nevertheless is distinct with legal, safe abortion increasingly replacing unsafe abortion. However, the case of South America is striking: the unsafe abortion ratio is still very high in spite of a rise in the prevalence of modern contraceptives from 50 to 65, with more than half of the modern method use attributable to sterilization to terminate childbearing. Nonetheless, an unmet need for spacing births appears to be met through unsafe abortion. The decline in regional numbers of births is because of the increasing tendency to regulate fertility by either contraceptive use or unsafe abortion. The speed of decline in fertility has outstripped the decline in unsafe abortion, thus accounting for relatively higher ratios.
South-East Asia and South-Central Asia (and to some extent western Asia and Oceania) represent the other pattern of moderately high fertility of around three children per woman and less than 50% modern contraceptive method use. A moderate decline in the unsafe abortion rate is noticed with little change in the ratio relative to live births. The trend in western Asia is less clear, because available data are generally limited.
- Contraceptive methods remain inaccessible or limited in choice for married women in some countries. However, access to contraception is worse for unmarried women, particularly adolescents. The age patterns of unsafe abortion reveal these most vulnerable groups. A recent review found that two-thirds of unsafe abortions occur among women aged 15-30 years. More importantly from a public health perspective, 2.5 million, or almost 14%, of all unsafe abortions in developing countries occur among women younger than 20 years of age.
- Each year more than 5 million women having an unsafe abortion (about one in four) experience complications, placing heavy demands on scarce medical resources. Mortality because of unsafe abortion is estimated from the total maternal mortality level. The estimated number of maternal deaths as a result of unsafe abortion ranges between 65,000 and 70,000 deaths per year. This corresponds to one woman dying because of a botched abortion approximately every 8 minutes. The most recent estimate (for 2003) shows that nearly all deaths attributable to unsafe abortion occur in developing countries. In eastern, western, and middle Africa, where maternal mortality is high, the unsafe abortion-related mortality ratio is higher than anywhere else, double that of Asia and more than five times that of Latin America. Morbidity is an even more frequent consequence of unsafe abortion; the disease burden for Africa is exceptionally high, threatening women’s lives and health and straining scarce resourced.
- The high risk of death from unsafe abortion in Africa reflects the procedures used and the poor availability, accessibility, and quality of services for management of complications. In middle, western, and eastern Africa, dangerous abortion methods, failing infrastructure, and poor public health facilities result in estimated case-fatality rates of around 800 per 100,000 procedures. IN contrast, South and Central America have case-fatality rates lower than 100 per 100,000 as a result of better infrastructures for health services and wider use of misoprostol. For Southern and Northern Africa and South-East Asia, the rates appear low but are still almost 200 times higher than that associated with a legal and safe abortion in the USA.
- Although unsafe abortion accounts for 13% of maternal deaths, it causes one-fifth of the total burden of the consequence of pregnancy and childbirth complications. The DALY of 100 per 1000 unsafe abortions in Latin America and the Caribbean is estimated to be the lowest among developing regions. The DALYs in Africa, Asia, and Oceania are six times, four times, and three times higher, respectively. These disparities reflect the risks because of abortion methods as well as access to health services in case of complications.
The most common causes for women to seek hospital care following an unsafe abortion are sepsis, hemorrhage, and trauma. However, for every woman who seeks medical care, many more have chronic pelvic or back pain and other complications.
- Induced abortion is arguably the most important human rights and equity issue of our time. Induced abortion exists in all parts of the world. Legal restrictions, mostly in developing countries, make abortion clandestine. The persistence of unsafe abortion continues to exert a heavy toll on women’s lives, especially in poor regions of the world and among the most disadvantaged.
“Adding it Up: The Costs and Benefits of Investing in Family Planning and Newborn Health” (2009)
[edit]Susheela Singh, Jacqueline E. Darroch, Lori S. Ashford, Michael Vlassoff ; (2009). “Adding it Up: The Costs and Benefits of Investing in Family Planning and Newborn Health” (PDF). New York: Guttmacher Institute and United Nations Population Fund.
- New analyses also show that the direct health benefits of meeting the need for both family planning and maternal and newborn health services would be dramatic.
*Unintended pregnancies would drop by more than two-thirds, from 75 million in 2008 to 22 million per year.
*Seventy percent of maternal deaths would be averted—a decline from 550,000 to 160,000.
*Forty-four percent of newborn deaths would be averted—a decline from 3.5 million to 1.9 million.
* Unsafe abortions would decline by 73%, from 20 million to 5.5 million (assuming no change in abortion laws), and the number of women needing medical care for complications of unsafe procedures would decline from 8.5 million to two million.
The healthy years of life lost due to disability and pre-mature death among women and their newborns would be reduced by more than 60%. (This is measured in disability-adjusted life years, or DALYs, an internationally used standard for comparing the cost-effectiveness of health services.) More women would survive hemorrhage and infection, and fewer would endure needless suffering from fistula, infertility and other health problems related to pregnancy or childbirth. Newborns would have improved chances of surviving asphyxia, low birth weight and infection.- pp.4-5
- In 2003, nearly 20 million abortions worldwide—about 47% of all abortions—were unsafe procedures. Unsafe abortions are defined as those performed by individuals lacking the requisite skills or in environments below the minimum medical standards, or both. More than 95% of unsafe abortions were in developing countries. The 1994 International Conference on Population and Development (ICPD) recognized unsafe abortion as a major health concern. It called for all women to have access to quality services to manage the complications arising from unsafe abortion.4 The failure to obtain postabortion care stems from a variety of factors, including inadequate capacity of health care systems; poor service quality; social stigma, which discourages women from using services; poverty and women’s low status; and women’s lack of independence in seeking health care.
- pp.11-12
- The ICPD also stated that in circumstances where abortion is not against the law, services should be safe. In some developing countries where abortion is permitted under broad legal criteria (for socioeconomic reasons or without restriction as to reason), safe services are generally accessible and almost all abortions are safe. Examples include Cuba, Tunisia, Turkey and Vietnam. In others, such as Cambodia, India, Nepal, South Africa and Zambia, access to safe abortion services is inadequate and a large proportion of women obtaining abortions still do so under unsafe conditions. A number of other countries that permit abortion for specific reasons (to protect the woman’s physical or mental health or in cases of fetal impairment, rape or incest), such as Colombia, Ethiopia and Ghana, are taking steps to provide safe abortion services under the permitted criteria, but their success in implementing such laws needs to be assessed. In countries where abortion is permitted on even narrower grounds (to save the life of the mother), access to safe legal abortion is extremely rare: In these countries, women who can afford to pay a private provider may obtain a safe clandestine procedure, but large proportions of abortions continue to be unsafe and to threaten women’s health and survival.
- p.12
- In 2008, an estimated 186 million women in developing countries were pregnant, of whom 123 million gave birth (93 million had intended to conceive, and 30 million had unintended pregnancies), and all of these women needed routine antenatal, delivery and postpartum care and care for their newborns; *28 million had miscarriages (and some needed medical care as a result); and *35 million had induced abortions (including about 20 million who had unsafe abortions and 8.5 million who needed care for complications of unsafe procedures).
However, many of these women did not get the medical care that they needed. There are major gaps in the availability, accessibility and content of maternal health services in the developing world, and variations among regions, subregions and countries are large. These gaps in service provision reflect, in large part, weaknesses in health systems, including inadequate infrastructure and insufficient availability of skilled health personnel. They also reflect, to some degree, economic, social, cultural and personal factors that constrain women’s access to health care. For example, the lack of culturally appropriate care may affect use of services; many families may be unable to pay required charges for services at a health facility or costs of transportation to get there; some societies may place lower value on women’s health than on men’s, thus making the perceived cost of care too high; or a couple may not seek care for an unwanted pregnancy. In addition, having closely spaced pregnancies, becoming pregnant at a very young age or after age 35, being undernourished or having underlying health problems, such as anemia, malaria and other illnesses, makes it difficult for women to have healthy pregnancies, safe deliveries and healthy babies.- pp.21-22
- Tens of millions of women in the developing world have an unmet need for maternal health care, in spite of the progress made over several decades of efforts to make pregnancy safer. Indeed, roughly half of women needing antenatal and facility-based delivery care, and 75% or more of those needing care for obstetric complications, do not receive it. The estimated total numbers of women who did not receive key components of needed pregnancy- related care in 2008 include
* 60 million who made fewer than the recommended minimum of four antenatal visits to a trained provider;
*55 million who did not receive facility-based delivery care;
* 4–6 million who did not receive needed care for each of the four major obstetric complications; and
*three million who needed and were unable to obtain care after an unsafe abortion.- p.23
- As discussed in Chapter 3, if all women at risk of unintended pregnancy used modern contraceptives, the number of women with unintended pregnancies would decline from 75 million to 22 million in the developing world as a whole, and the number of unplanned births would decline from 30 million to about eight million. Reducing unintended pregnancies can make improvements in maternal health care more affordable. Providing medical care related to unintended pregnancies currently costs $2.5 billion (Figure 5.1). However, some women do not receive care, and others receive care that does not meet the recommended standards. If the recommended care were provided to all women who have unplanned births or unsafe abortions, the cost of care for unintended pregnancies would increase to $6.9 billion. But if all women wanting to avoid a pregnancy used modern contraceptives, the resulting decline in unintended pregnancies would reduce the cost of providing all of these women with the recommended standard of maternal and newborn care by $5.1 billion—from $6.9 billion to $1.8 billion. Low-income countries would benefit to an even greater extent than other countries from this large cost saving: These countries would account for 56% of the $5.1 billion in savings, even though they are home to only about 23% of women of reproductive age. As noted in Chapter 3, the cost of providing modern family planning methods to women with unmet need is an additional $3.6 billion. That means that for each additional dollar spent to provide modern contraceptives, $1.40 would be saved in costs of medical care because fewer women would have unintended pregnancies.
- p.26
- While treating postabortion complications currently contributes only 4% of the costs of medical care related to pregnancy, complications from induced abortions account for 13% of maternal deaths and 20% of healthy years of life lost among women because of pregnancy-related conditions. The high levels of abortion-related health complications reflect both the high levels of unintended pregnancy and the poor conditions under which many women have abortions.
If women’s contraceptive needs were fully addressed (and assuming no changes in abortion laws), the reduction in unintended pregnancies would result in very large declines in abortions and related health complications.
The number of induced abortions in the developing world would decline by 70%, from 35 million to 11 million.
The number of unsafe abortions would decline by 73%, from 20 million to 5.5 million.
The number of women needing medical care for complications from unsafe abortion would decline by 73%, from 8.5 million to 2.3 million.
Safe and legal abortions would decline by 66%, from 15 million to 5.1 million.- p.27
- Reducing the number of abortions, particularly those that are unsafe, would have a large impact on various dimensions of the cost of health care services. The cost of providing postabortion care for the approximately 5.5 million women in the developing world who currently receive it is $370 million. This amount would increase to $880 million if the approximately three million women who need and are not receiving postabortion care were to receive it. However, if all women at risk of unin- tended pregnancy used modern contraceptive methods, the resulting declines in unintended pregnancy and unsafe abortion would reduce the cost of postabortion care to about $230 million a year (and to $9 million if all abortions were safe).
If modern contraceptive needs were fully met, the number of maternal deaths due to unsafe abortion would decline by 82%, from an estimated 70,000 to around 10,000, assuming all women who need postabortion care receive it, and assuming no change in abortion laws.- p.27
- Our estimates assume that even when abortions are provided by trained personnel in hygienic and legal settings, 1% of women will experience complications.
- p.27
- Family planning and maternal and newborn health services have substantial, measurable impacts on the health of women and families, as this report has shown. These services save lives, improve long-term prospects for good health, and enhance individuals’ and families’ productivity and well-being. In addition, the services save money in at least two ways. First, when women postpone or avoid unintended pregnancies, fewer resources are needed to provide maternal and newborn health care and to manage complications of unsafe abortion. Second, when all pregnant women and their babies receive the recommended standard of maternal and newborn health care, complications that might incur high costs can be avoided or managed at lower cost.
- Ch.6 Conclusion p.31
- The use of modern family planning methods and maternal and newborn health care already contributes to lower rates of unintended pregnancy, unsafe abortion, and maternal and newborn death and disability. But all of these indicators remain too high in the developing world. Of the 186 million pregnancies that occurred in 2008, about two in five were unintended, and nearly half of these ended in abortions, many of which occurred under unsafe conditions.
- p.31
- Insufficient and unpredictable funding are key factors hindering improvements in the availability and quality of family planning services and maternal and newborn health care. While other constraints also exist and must be dealt with, the solutions will require substantial increases in resources and much stronger political support. Moreover, these solutions will require action at the national, regional and international levels. Weaknesses in health systems that need to be addressed include insufficient physical capacity, weak contraceptive and medical commodity supply systems, poor financial management systems and too few trained health professionals. Nonsystem barriers also hinder improvements in health care, such as stigma among providers toward unmarried, sexually active young people, or toward women who have had unsafe abortions. Moreover, cultural and individual attitudes and behaviors can impede the use of sexual and reproductive health services and will require attention (in the form of increased health information and outreach) at the same time that health systems are strengthened.
- pp.33-34
“Unsafe abortion : global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003” (2007)
[edit]Swett, C. (2007). “Unsafe abortion : global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003” (5th ed.). World Health Organization. ISBN 978-92-4-159612-1. Archived from the original on 7 April 2018. Retrieved 24 March 2018.
- Unsafe abortion continues to be a major public health problem in many countries. A woman dies every eighth minute somewhere in a developing country due to complications arising from unsafe abortion. She was likely to have had little or no money to procure safe services, was young – perhaps in her teens – living in rural areas and had to procure safe services, was young – perhaps in her teens – living in rural areas and had little social support to deal with her unplanned pregnancy. She might have been raped or little social support to deal with her unplanned pregnancy. She might have been raped or she might have experienced an accidental pregnancy due to the failure of the contraceptives she might have experienced an accidental pregnancy due to the failure of the contraceptive method she was using or the incorrect or inconsistent way she used it. She probably first attempted to self-induce the termination and after that failed, she turned to an unskilled, but relatively inexpensive, provider. This is a real life story of so many women in developing countries in spite of the major advancements in technologies and in public health.
- Halfdan Mahler, Preface, 25 September 2007
- This report gives estimates of the number of unsafe abortions and associated mortality for the year 2003. Nearly 20 million unsafe abortions took place that year, 98% of them in developing countries with restrictive abortion laws. These countries often also have low rates of use of modern reversible contraceptives and high levels of unmet need for family planning.
- Abstract
- Methods to terminate an unwanted or unintended pregnancy are known to have existed since ancient times. As far back as 5000 years ago, the Chinese Emperor Shen Nung described the use of mercury for inducing abortion.1 A recent publication lists over 100 traditional methods of inducing abortion, which can be broadly classified into four categories: (1) oral and injectable medicines; (2) vaginal preparations; (3) introduction of a foreign body into the uterus; and (4) trauma to the abdomen. Many of these methods pose serious threats to the woman’s life and well-being.
Each year, throughout the world, approximately 210 million women become pregnant and some 130 million of them go on to deliver live-born infants. The remaining 80 million pregnancies end in stillbirth, or spontaneous or induced abortion. Approximately 42 million pregnancies are voluntarily terminated each year – 22 million within the national legal system and 20 million outside it. In the latter case, the abortions are often performed by unskilled providers or in unhygienic conditions, or both.
Only one in three legal (and mostly safe) abortions take place in developing countries (excluding China), while 98% of unsafe abortions occur there. Over five million or approximately 1 in 4women having an unsafe abortion is likely to face severe complications, which can cause death, and will seek hospital care, putting heavy demand on scarce resources. Unsafe abortion nonetheless remains a neglected health care problem in developing countries.- p.1
- The World Health Organization (WHO) is concerned with the public health aspects of unsafe abortion. As early as 1967, the World Health Assembly passed Resolution WHA20.41, which stated that “abortions ... constitute a serious public health problem in many countries”, and requested the Director-General to “continue to develop the activities of the World Health Organization in the field of health aspects of human reproduction”. WHO defines unsafe abortion as a procedure for terminating an unintended pregnancy carried out either by persons lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both.
The consensus statement of the 1994 International Conference on Population and Development (ICPD) noted that “All Governments and relevant intergovernmental and non-governmental organizations are urged to strengthen their commitment to women’s health, to deal with the health aspect of unsafe abortion as a major public health concern and to reduce the recourse to abortion through expanded and improved family-planning services.”
The above was reiterated in 1999 at the five-year review of the implementation of the ICPD Programme of Action by the UN General Assembly in New York, USA. The Assembly further agreed that, “in circumstances where abortion is not against the law, health systems should train and equip health-service providers and should take other measures to ensure that such abortion is safe and accessible.”- p.1
- The incidence of unsafe abortion is influenced by the legal provisions governing access to safe abortion, as well as the availability and quality of legal abortion services. Restrictive legislation is associated with a high incidence of unsafe abortion.
- p.2
- It has been estimated that almost 40% of pregnancies worldwide are unplanned – the result of non-use of contraception, ineffective contraceptive use or method failure. Unintended pregnancy, and induced abortion, can be prevented and reduced by expanding and improving family planning services and choices, reaching out to communities and underserved population groups, for example sexually active teenagers and unmarried women.
- p.2
- When people are motivated to regulate their fertility, but effective contraception is largely inaccessible or not consistently or correctly used, a large number of unplanned pregnancies occur. Many married women in developing countries do not have access to the contraceptive methods of their choice. The situation is even more difficult for unmarried women, particularly adolescents, who rarely have access to information and counselling on sexual and reproductive health, and are frequently excluded from contraceptive services. An estimated 123 million women have an unmet need for family planning. During rapid transition from high to low fertility, as has been witnessed in several countries, contraceptive services are often unable to meet the growing demand of couples for fertility regulation, resulting in an increased number of unplanned pregnancies, some of which are terminated by induced abortion. Also, where less effective family planning methods are commonly used, unplanned pregnancies and, consequently, abortions are likely to occur. Of course, no contraceptive method is 100% effective. It is estimated that each year 27 million unintended pregnancies occur as a result of method failure or ineffective use; of these, about 6 million occur even though the contraceptive method has been used correctly and consistently.
- pp.2-3
- Each year, an estimated 80 million women have an unplanned pregnancy. Some of these women will decide to continue the pregnancy, while others will consider having an abortion. A number of women who attempt to have an abortion will not be successful, and will carry the unwanted pregnancy to term. The number of women who attempt an unsafe abortion, risking their life and health, is 20–25% higher than the number who succeed. In addition, some women may make repeated attempts to terminate a pregnancy before succeeding, each time risking their health.
- p.4
- When induced abortion is performed by qualified persons using correct techniques and in sanitary conditions, it is a safe surgical procedure. In the USA, for example, the death rate from induced abortion is now 0.6 per 100 000 procedures, making it as safe as an injection of penicillin. In developing countries, however, the risk of death following unsafe abortion may be several hundred times higher. Spontaneous abortion is rarely fatal and seldom presents complications.
The mortality and morbidity risks associated with unsafe induced abortion depend on the facilities and the skill of the abortion provider, the method used, the general health of the woman and the stage of her pregnancy. Unsafe abortion may be induced by the woman herself, by a non-medical person or by a health worker under unhygienic conditions. Abortion attempts may involve insertion of a solid object (root, twig or catheter) into the uterus; a dilatation and curettage procedure performed improperly by an unskilled provider; ingestion of harmful substances; exertion of external force; or misuse of modern pharmaceuticals. In many settings, traditional practitioners vigorously pummel the woman’s lower abdomen to disrupt the pregnancy; this can cause the uterus to burst, killing the woman.- p.5
- One recent study estimated that every year in developing countries five million women are admitted to hospital as a result of unsafe abortion.5 The treatment of abortion complications in hospital consumes a significant share of resources, including hospital beds, blood supply, medications, and often operating theatres, anaesthesia and medical specialists. Thus, the consequences of unsafe abortion place great demands on the scarce clinical, material and financial resources of hospitals in many developing countries, undoubtedly compromising other maternity and emergency services. Major physiological, financial and emotional costs are also incurred by the women who undergo unsafe abortion.
- p.5
- A review of the combined impact of mortality and morbidity due to unsafe abortion estimated that, every year, there are 65 000 to 70 000 deaths and close to five million women with temporary or permanent disability due to unsafe abortion. Of these, more than 3 million suffer from the effects of reproductive tract infection (RTI), and almost 1.7 million will develop secondary infertility. Unsafe abortion accounts for 13% of maternal deaths, and 20 % of the total mortality and disability burden due to pregnancy and childbirth, in terms of disability-adjusted life years (DALYs).
Altogether some 24 million women currently suffer secondary infertility caused by an unsafe abortion. In DALYs, the combined burden of mortality and morbidity per 1000 unsafe abortions is exceptionally high in sub-Saharan Africa, where it is 50 percentage points higher than in Asia and 6 times greater than in Latin America.- p.5
- Where induced abortion is restricted and largely inaccessible, or legal but difficult to obtain, little information is available on abortion practice. In such circumstances, it is difficult to quantify and classify abortion. What information is available is inevitably not completely reliable, because of legal, ethical and moral considerations that hinder reporting. Occurrence tends to be under-reported in surveys, and unreported or under-reported in hospital records. Of course, there are no records on women who do not seek post-abortion care in hospitals. Only the “tip of the iceberg” is, therefore, visible in the number of deaths and the number of women who suffer severe trauma, or who have an infection or severe blood loss and seek medical care.
Whether legal or illegal, induced abortion is generally stigmatized and frequently censured by religious teaching or ideologies. Women are often reluctant to admit to an induced abortion, especially when it is illegal, and under-reporting occurs even where abortion is legal. Whenabortions are clandestine, they may not be reported at all or may be reported as spontaneous abortion (miscarriage). The language used to describe induced abortion reflects this ambivalence: terms include “induced miscarriage” (fausse couche provoquée), “menstrual regulation”, and “regulation of a delayed or suspended menstruation”. For example, in one study 16.6% of women admitted to an abortion; however, only 4.4% said they had terminated a pregnancy, and 12.2% reported that they had “induced menstruation”. It is therefore not surprising that unsafe abortion is one of the most difficult indicators to measure.- pp.6-7
- Induced abortions outside the legal framework are frequently performed by unqualified and unskilled providers, or are self-induced; such abortions often take place in unhygienic conditions, and involve the use of dangerous methods or incorrect administration of medications. Even when performed by a medical practitioner, an abortion that is carried out in secret, outside a recognized facility, generally carries an additional risk: medical back-up is not immediately available in an emergency, the woman may not receive appropriate post-abortion attention and care, and if complications occur, the woman may hesitate to seek care. The relative safety of unsafe abortion differs by country depending on the skills of the providers and the methods used, but is also linked to the de facto application of the law.
- p.7
- Unsafe abortion is negligible in eastern Asia and in some developing countries of other regions where abortion is legal and relatively accessible, in particular Cuba, Singapore, Tunisia, Turkey and Viet Nam. Rates and ratios that exclude these countries therefore provide a better reflection of the situation of unsafe abortion in the region or subregion as a whole.
- p.8
- Unsafe abortion rates close to 30 per 1000 women of reproductive age are seen in both Africa and Latin America; however, because of the higher relative number of births, the unsafe abortion ratio for Africa is only half that for Latin America. However, the range of estimates for Africa is wide: Eastern Africa has the highest incidence rate of any subregion, at 39 per 1000 women aged 15–44, while Southern Africa has among the lowest, at 18 per 1000 (not counting legal abortions of 5 per 1000 women). In Eastern, Western and Middle Africa, where maternal mortality is high, the unsafe-abortion-related mortality ratio is much higher than anywhere else – double that of Asia and more than 5 times that of Latin America. Morbidity is an even more frequent consequence of unsafe abortion, and it is thus not surprising that the total disease burden for Africa is exceptionally high, threatening women’s lives and health, and straining scarce resources.
Middle, Western and Eastern Africa all have a contraceptive prevalence below 25%, with heavy reliance on traditional methods. In Southern and Northern Africa, contraceptive prevalence among married women is around 50%, and there is greater reliance on reversible modern methods (36% and 43%, respectively). This could help explain the moderate abortion rates of around 20 per 1000 women, as compared to 26 to 39 per 1000 in other parts of Africa.- p.15
- The incidence of unsafe abortion for Latin America overall appears to have stabilized, and may have passed its peak. If Cuba is excluded from the calculation, the incidence rate for the Caribbean falls between those for Central America (25 per 1000) and South America (33 per 1000). The prevalence of modern contraceptives ranges from 57% to 66% in Latin America; however, 43–50% is accounted for by sterilization. The moderate 29–38% prevalence of reversible method use could mean that unsafe abortion is being used to space births, to arrive at a total fertility rate of around 2.5 per woman. Improved access to a range of birth-spacing methods could reduce the number of unintended pregnancies and hence the need for abortion. Almost 2000 deaths from unsafe abortion occur, approximately 20 per 100 000 births; this is the lowest among the developing regions, and is attributable to the relatively well functioning health services in Latin America.
- pp.15-16
- South-central Asia has the highest number of unsafe abortions of any subregion, owing to the sheer size of its population; in 2003, there were 6.3 million unsafe abortions, or 18 per 1000 women of reproductive age, which poses a formidable challenge. Use of modern contraceptive methods among married women is modest (42%), and two-thirds of this use relates to sterilization; the high number of unsafe abortions is probably the result of a desire to space births. Nevertheless, among Asia’s subregions, South-eastern Asia has the highest incidence rate, at 27 per 1000 women aged 15–44 (excluding countries with no evidence of unsafe abortion); this rate is similar to those of the Caribbean and Central America. South-eastern Asia has a 51% prevalence of modern family planning methods, almost exclusively reversible methods (43%). It appears, though, that abortion is required to keep fertility low. The unsafe-abortion-related mortality for Asia is 2–3 times that for Latin America, but less than half that for Africa, reflecting the relative standards of health services and infrastructure.
While it is acknowledged that there is a problem of unsafe abortion in Oceania, data are exceptionally scant and, as a consequence, estimates vary.- p.16
- There has been a small reduction in the number of deaths in 2003 due to unsafe abortion compared with the estimate for 2000. This is in line with the assumption that maternal deaths in general may be slowly declining globally, probably as a result of improved maternity services and better cared.Overall, 66 500 maternal deaths were estimated to have been due to unsafe abortion in 2003. Nearly all of these deaths could have been prevented if the need for family planning had been met, and if abortion services had been legally available and affordable everywhere.
- p.17
- The estimated case-fatality rate (deaths per 100 000 unsafe abortion procedures) ranges from a high of 750 per 100 000 in sub-Saharan Africa to 10 per 100 000 in developed regions, with an average of 350 per 100 000 for developing regions. Table 3 also shows that the global case-fatality rate associated with unsafe abortion is some 550 times higher than the rate associated with legal induced abortions in the USA (0.6 per 100 000 procedures); in sub-Saharan Africa, the rate is well over 1000 times higher. Even in developed countries, the case-fatality rate for unsafe abortion is 20 times higher than that for legal induced abortion.
- p.18
- Major progress has been made in some areas of sexual and reproductive health, most notably in contraceptive use. However, unsafe abortions, though entirely preventable, continue to occur in almost all developing countries. The major public health implications include, but are not limited to, maternal morbidity and mortality. In addition, there are financial costs to women and to health services for treating complications.
Governments need to assess the health impact of unsafe abortion, reduce the recourse to abortion by expanding and improving family planning services, and design abortion policies and interventions to improve women’s health and well-being. Preventing unintended pregnancies and unsafe abortion must continue to be a high priority for improving women’s sexual and reproductive health. Information and services for family planning and abortion care should be readily available, including to young people.
In several countries, the legalization of abortion has not been followed by elimination of unsafe abortion. This may be because women are unaware that safe abortion services are available, or lack the resources, time or decision-making power to use the services, or because the services are inadequate to meet demand. Other factors inhibiting use of safe abortion where it is legal are lack of privacy and confidentiality, poor access, and discouraging attitudes of health care providers.- p.20
“Economic impact of unsafe abortion-related morbidity and mortality: evidence and estimation challenges” (December 2008)
[edit]Vlassoff M, Shearer J, Walker D, Lucas H (December 2008). “Economic impact of unsafe abortion-related morbidity and mortality: evidence and estimation challenges” (PDF). Research Report. Vol. 59. Brighton, UK: Institute of Development Studies.
- Unsafe abortion-related morbidity and mortality (UARMM) exacts a huge price annually in terms of the lives and health of women in developing countries each year. Almost 20 million unsafe abortions occur annually, virtually all in the developing world. More than 5 million of these result in medical complications so serious that they require hospitalisation. The economic cost of UARMM is also enormous, burdening public health systems, the households in which these women live and also the economies of the countries themselves. The empirical data needed to estimate most of these costs are scant and in some cases, practically non-existent, but several studies of direct health-system costs are available in the literature. These data exist in two forms which allow cost estimation using two distinct methodologies, one which uses cost-per-patient data, and one which uses a model of ideal treatment inputs. Examining the cost of UARMM to health systems using both of these methodologies, we find that the total cost to the developing world lies between $375 and $838 million, with a central estimate of around $500 million (2006 US$). Regional cost estimates show that in relation to purchasing power, abortion complications are considerably more expensive to treat in sub-Saharan Africa than in Latin America. Furthermore, millions of other women with serious complications receive no treatment from the health system. If they were able to do so, an additional $375 million or so would be expended, but this estimate rests on scant empirical data. The cost of long-term morbidities, mainly infertility and chronic reproductive tract infections, may cost many billions of dollars annually, while the losses to the economies of developing countries from lower productivity caused by UARMM may be more than $400 million. Out-of-pocket expenses to the women and their families may amount to a further $600 million. Very little data exist to make these latter estimates, but they at least show that the total cost of UARMM would be many times greater than the direct health costs, for which solid evidence does exist.
- p.5
- Unsafe abortion-related morbidity and mortality (UARMM) impacts welfare at the individual, household, community and national levels. Out of an estimated 46 million induced abortions that take place every year in the world, around 19.8 million are unsafe abortions (WHO 2007b). More than 5 million of these abortions result in serious medical complications that require hospital-based treatment (Singh 2006). Of these cases, many suffer long-term effects, including an estimated 1.6 million women who annually suffer secondary infertility and a further 3–5 million women experience chronic reproductive tract infections.
The cost that these figures imply is a matter of importance for public policy. Despite this, little research has gone into estimating UARMM costs or developing an overall framework and costing methodology to arrive at cost estimates. The objectives of this report are to survey the empirical information available on costing unsafe abortion, to develop an analytical framework for cost estimation, to describe the methodological approaches available, given the constraints of the subject matter, and finally to estimate cost ranges within the limitations of data on unsafe abortion.
The complications from unsafe abortion have been listed elsewhere, for instance by Bernstein and Rosenfield (1998) and WHO (1995). Empirical studies on abortion complications, however, show that the list of possible complications is a very long one. Annex Table A1 attempts to organise this long list into three categories: immediate complications, later complications and other complications that are reported only sporadically in the literature. A complete costing of abortion-related complications would need evidence on the prevalence of all the complications listed in the table. When we look at empirical costing studies below, however, we will find that in practice only a few of the major complications are taken into consideration.- 1 Introduction, p.9
- Unsafe abortion generates unnecessary costs to society at a variety of levels. Where abortion is illegal, households will generally finance the costs of the abortion procedure from their own resources. Even where abortions are legal, many women will still have recourse to unsafe procedures for a variety of reasons: the stigma that society still attaches to abortion, the desire of the woman to maintain a cloak of secrecy, or the inadequacy of the health system vis-à-vis abortion procedures. The 19.8 million women who undergo unsafe abortions annually incur a variety of costs to society, the household and the individual. Figure 2.1 presents a framework for analysing these costs in the form of a decision diagram. An unknown proportion of women who have an unsafe abortion will experience serious complications; some of these women will seek care within the formal health system, while many will seek care outside of the formal health system or not seek care at all. Where women seek care determines who bears the direct medical costs. In public facilities, the costs may be shared between households and government if fees are charged. The process of seeking care will also incur direct non-medical costs, such as transport costs, which can be significant (Borghi 2006 a,b).
Women suffering from complications face three possible outcomes: survival with no long-term consequences; survival with long-term consequences, such as chronic pelvic infections, sub-fecundity and infertility; or death. Whether, where and how soon care is sought influences the probability of each outcome. Each outcome generates indirect costs in the form of lost productivity, which will be borne by the households affected, and society more broadly. In economies with large pools of unemployed, however, these costs will be more easily offset at the societal level. Indeed, even at the household level, some proportion of short-term lost productivity would most likely be made up by the individuals themselves or friends and family. However, long-term productivity losses cannot be offset at an individual/household level in the same way they can at societal level. Finally, children from households experiencing a maternal death may also suffer in terms of their future health and education potential (Strong 1992), with further economic implications for the household and society.
The emphasis in this framework is on costs that can be measured in monetary terms, although how to value lost productivity, in the case of indirect costs, is a question that is still open for discussion. Social and psychological costs are difficult to monetise, but are nonetheless real. The stigmatisation that women, who are known to have had an abortion, suffer is a very real cost in some societies. Other psychological traumas that post-abortion women may suffer also may impose great costs on the women, which also may be hard to quantify.
While recognising the multidimensional nature and range of potential economic impacts, the focus of this report is on estimating one component – the health-system cost of treating the consequences of unsafe abortion (see the bold block in Figure 2.1). For other costs, where in general data availability is more problematical, the report discusses methodological issues as well as making some preliminary cost estimates.- 2 Framework of Analysis, pp.9, 11
- Benson and Crane (2005) estimate that 45 per cent of unsafe abortions result in health complications (26 per cent of them being serious complications and 19 per cent of them minor).
- Footnote 2, p.11
- Post-abortion complications (PAC) cover a very wide range of medical problems. The treatments and interventions mentioned in the empirical literature, however, are less extensive. Annex Table A3 provides a list of treatments referred to in published empirical studies of PAC. The following is a summary of the medical procedures and treatments reported on in this literature: Operative procedures
* Colpopuncture
*Colpotomy
*Dilation and curettage
*Hysterectomy
*Intestinal resection
*Laparotomy
*Manual vacuum aspiration
*Resuscitation, intensive care unit
*Surgery (unspecified)
Other procedures
*Blood transfusions
*General anaesthesia
*Intravenous antibiotics
*Intravenous fluids
*Local anaesthesia
*Sedation
Medicine administered
*Abortifacients
*Analgesics
*Antibiotics
*Antimalarial drugs
*Flagyl
*Haematinics
*Tetanus vaccination
*Vitamins
This list is incomplete. For instance, treatment for poisoning, renal failure, psychosis and infertility, inter alia, would require interventions not listed here.- p.13
- It can be observed in Annex Table A2 that costs vary greatly from one study to the next, the range being from $2.34 to $389 (in 2006 US$). It seems obvious that the definitions of what constitutes costs must vary widely from one setting to another. A number of possible explanations can be advanced to explain these differences. Personnel time costs may be estimated according to the actual patient–provider contact time in one study but by dividing the salary cost of personnel by the number of patients attended in another study. Indirect costs such as overhead costs, capital depreciation costs, administrative costs, etc. may be included in one study but excluded in another. Probably the most significant source of variation in costs, however, is the inclusion or exclusion of subsidised costs from study to study. It is scarcely conceivable that PAC costs in Mexico, for instance, could be 15 times the costs in Brazil; two countries with similar social and economic settings. The Mexican cost estimate may include many more of the real costs for post-abortion treatment than does the Brazilian estimate because the latter cost may be highly subsidised, hiding many of the true costs from easy detection. To arrive at reasonable regional or global cost-per-patient estimates, therefore, it will be necessary to make some assumptions about the inclusion/exclusion of certain cost components, all of which are equally valid components of the true cost of PAC, even if some may be more difficult to measure than others. To get a better appreciation of cost measurement issues, we look briefly at two important components of PAC costs that are often reported in costing studies, namely, hospitalization and blood transfusions. Annex Table A4 presents all costing studies that have specific findings regarding hospitalisation of patients as part of PAC. The simple average length of stay (ALOS) across all studies is 85 hours, or a little over three days. Again, there is a very wide variation in hospitalisation, from 9.9 hours in an Ecuadorian study to over 26 days in a Nigerian study. Sample designs differ across these studies. Although all studies observed women coming to hospitals for treatment of complications after experiencing induced abortions, there were some studies that covered only the most severely complicated cases or took place in settings where the overall safety of abortion procedures was extremely low, while other studies covered settings where abortion methods were on average less dangerous.
- 3.2 Data considerations, p.14
- Of the 37 studies reporting hospitalisation data, 25 studies were of the former type and 12 were not. The average stay in studies of the MVA-D&C-comparison type was 35 hours, whereas in the remaining studies the average was 153 hours.
- 3.2 Data considerations, p.14
- Annex Table A5 summarises findings from 14 PAC costing studies that contained data on blood transfusions, an important and expensive component of PAC costs. In these studies, on average, about 8 per cent of women seeking care after induced abortions received blood transfusions. The amount of blood given to women who had transfusions is more difficult to estimate since it often was not reported. The two most recent studies estimated that 1.3 litres were administered per case, whereas the older studies estimated that around 0.6 litres was given per woman (Fortney 1981). It should be noted that some of these studies mentioned that blood transfusions were restricted by the availability of a blood supply in hospitals. The lower figure may therefore be more indicative of supply constraints than of effective demand. The data presented in Annex Tables A3, A4 and A5 clearly show that a wide range of PAC costs are reported in the literature and that cost variability persists within regions and even within single countries.
- 3.2 Data considerations, p.15
- Data on abortion-related complications by severity are limited. One study in South Africa (Kay et al. 1997) has used this categorisation to estimate PAC costs according to severity of complication. Another study in Kenya has also used this framework, although it did not measure costs (Gebreselassie et al. 2005).
- p.15
- The evidence base on the cost of unsafe abortion is limited, and regional or global economic impacts are currently unknown. As the literature review in the previous section has shown, however, a number of empirical studies have examined costs in several developing countries. These studies typically collect data from a specific region of the country or from specific health facilities. Most of the studies estimate costs on a per-case basis. This is most often an overall cost, but at least one study has estimated per-case costs broken down by severity of complication and level of facility (Kay et al. 1997). The full direct cost of treatment includes health-system costs as well as out-of-pocket patient costs such as transportation costs and, depending on the health system, co-payments and fees for specific inputs. Generally, however, patient costs have not been reported on. The direct costs estimated in this section, therefore, refer only to costs to the health system.
- 4 Cost to health system of unsafe abortion: global and regional estimates, p.16
- We use the term ‘global' because our estimates include all unsafe abortions; however, virtually all unsafe abortions occur in developing regions.
- Footnote 11, p.16
- The average cost estimates varies greatly between. Even studies in two broadly comparable countries using what appear to be similar methodologies yielded very different results, e.g. an estimate of $20 per case in Brazil, compared with $320 in Mexico (Fonseca et al. 1997; Brambila 1999). Even within the same country, there were large variations in cost estimates, e.g. Mexico or Peru. The studies identified were often not clear on which resources were included, measured and valued, nor on which populations of PAC cases were being sampled. While most or all of the low cost estimates likely omitted some important categories of cost, it was generally not possible from the information provided to determine where this was the case.
- p.20
- The first row of Table 4.2 shows simple averages taking into account all 72 cost estimates available. In terms of US dollars (2006 US$), the average cost per patient is $86.04. Keep in mind that the data comes preponderantly from the sub-Saharan Africa and Latin America and Caribbean regions, and that, even so, only a few countries within these regions are included. Of the 72 samples, 46 can be categorised as low-severity samples, meaning that the women sampled would be classified as having ‘low’ severity complications using the Kay-Rees severity framework. The other 26 samples included women of all severity categories.
- p.21
- The average cost per patient for treating low-severity complications is $72.07, while the average cost for samples of women with all types of complication is $110.76.
- p.22
- Of the 24 studies, 12 took place in Africa (11 in sub-Saharan Africa) and 12 in Latin America and the Caribbean. Average costs per patient by region are shown in rows 7–10 of Table 4.2. In terms of US dollars (2006 US$), there is little variation by region, from $82.63 in all of Africa to $93.92 in LAC. Since no empirical data are available for either the Asia/Pacific region or for developing countries in Europe, the average of African and LAC costs ($88.28) is used in these regions (row 9). It is interesting to compare costs in terms of international dollars (2006). Even though cost per patient is higher in LAC than in SSA in real terms, in terms of international dollars, the average cost in SSA is substantially higher (c.$228 vs. $161), showing that in relation to purchasing power, abortion complications are considerably more expensive to treat in sub-Saharan Africa than in Latin America, despite the former being the poorer region.
- p.23
- Row 12 shows the costs per patient for the second calculation method, where information about the incidence and cost of treatment by severity level is used. The average cost is calculated to be $114.96 per patient. Two studies (Kay et al. 1997; Gebreselassie 2005) provide information on severity patterns in South Africa and Kenya. Combining the two studies, we assume that low-severity cases are 63.6 per cent, mid-severity cases 15.9 per cent and high-severity cases 20.5 per cent of the total. Using these percentages as weights together with the estimated costs by severity of the South African study, we arrive at an average cost across all levels of severity. This approach is, of course, a crude one, extrapolating the experiences of two SSA countries to the whole developing world. It is worth using this method, nonetheless, because it takes into account available data on the severity pattern of post-abortion complications, even if in a crude way.
- p.23
- Finally, in rows 16–19, average costs using the fourth calculation method are shown. This method assumes that most studies have underestimated the true cost of treatment by omitting certain, hard-to-measure cost components. In particular, overhead and capital costs are frequently omitted. Using information from the five studies which applied the MBP costing model, rough estimates of the shares of overhead and capital costs in total treatment costs were made. Based on these five studies, direct costs are estimated to be 72 per cent, overhead 16 per cent and capital 12 per cent of total costs. Observed costs are then inflated by a factor of 1.38 (1.00/0.72 = 1.38) to take into account overhead and capital. The estimated costs using this method are higher than those from any of the other three methods and so form the upper boundaries of the cost ranges.
- p.23
- Regional and global estimates of health-system costs are presented in Table 4.3 for the four proposed calculation methods. Globally, the total cost estimates range from $383 million to $681 million. The central estimate of global expenditure by health systems for PAC is $555 million. Of the four methods, the first one, which uses low-severity average costs, is the least likely scenario and is included mainly to set lower bounds for the probable cost ranges. Methods 2 and 4 make use of additional data apart from the empirically derived costs per patient. In each case, however, the added information, though theoretically appealing, is scant and necessitates assumptions that only roughly approximate reality. For example, the pattern of severity is maintained constant across all regions for lack of more specific regional data. This limitation probably distorts regional prevalence estimates. For instance, only 19 per cent of all serious complications in the developing world are estimated to occur in sub-Saharan Africa, even though around 43 per cent of all maternal deaths due to unsafe abortion come from that region. Obviously, more data on both severity patterns and omitted cost components should be collected through further research in order to improve the precision of these estimates.
- p.25
- Table 4.5 shows the cost-per-case results of the empirical studies. The overall costs per patient (in 2006 US$) show a lot of variability, from about $10 to $106, under current practice, and from $31 to $213, under ‘standard’ practice. Latin American costs seem to be substantially higher than African costs, as we would have predicted. Also, except for the Ghana study, ‘standard’ costs are substantially higher than current costs. One reason for this may be that current treatment regimes are actually sub-standard in that insufficient resources are being applied to each case. We must not forget the other possibility, however, namely that standard treatment protocols include inflated resource input requirements and that, in practice, requirements are less than the standard protocol, allowing savings to be realised without decreasing service quality.
With only five empirical studies having used the MBP costing spreadsheet, precise estimates of global and regional costs of PAC treatment are not possible. Nonetheless, with three countries covered in sub-Saharan Africa and two in Latin America and Caribbean, rough estimates of the magnitude of PAC costs are possible for those two regions. If we make the simplifying assumption that the per-case costs in the other developing regions are averages of the former two regions, we can make first-approximation estimates for all developing regions. Table 4.6 illustrates the probable magnitude of global and regional costs of treating the complications of unsafe abortion. Roughly speaking, the estimates shown under ‘current’ correspond to expenditures actually made for treatment, whereas those under ‘standard’ correspond to what would be expended if PAC treatment protocols matched the standards recommended by WHO. For the developing world as a whole, we estimate that about $463 million is currently being expended on treating the 5.6 million hospitalisations due to unsafe abortion. If standard WHO-recommended protocols were being followed, however, an estimated $656 million would be expended. Note that these estimates do not include the millions of women who have serious complications but never reach a health facility.
As mentioned, no empirical data exist – using the MBP methodology – for the Asian region, Northern Africa, or developing countries in Europe. We have assumed that simple cost averages for the two regions where data do exist can be used to estimate costs in the other regions. We can perform a simple sensitivity analysis to find a range of estimates for total expenditures by using the lowest cost estimates (from sub-Saharan Africa) to find the lower bound of the range, and the highest cost estimates (from Latin America and Caribbean) to calculate the upper bound of the range. These lower and upper limits are shown in the rightmost four columns of Table 4.6. For actual or ‘current’ expenditures, we see that the range is from $375 million to $550 million, while for WHO ‘standard’ coverage, the total cost ranges from $474 million to $838 million.- p.28
- Benson and Crane (2005) estimates that only around 75 per cent of women needing hospital care after unsafe abortions actually present themselves at hospitals. Kay et al. (1997: 446), however, quoting an older study from Chile, reports that perhaps only ‘10–50% of women who have had unsafe abortions actually receive medical attention'. In this study, the 15–25 per cent range reported by Singh (2006) has been used.
- Footnote 16, p.29
- A major lacuna in abortion macro-analysis is the almost complete lack of information about the prevalence of women with serious complications who fail to receive medical attention from a regular health facility. Some informed estimates put this proportion at between one-third and one-half of those who experience complications in countries where access to abortion is highly restricted (Alan Guttmacher Institute 1999; Benson and Crane 2005). On the basis of very incomplete data, Benson and Crane estimate that 45 per cent of unsafe abortions – 8.9 million – may result in complications annually. Using the estimate of Singh (2006), namely that around 15–25 per cent of women undergoing unsafe abortions suffer untreated complications, we estimate that between 3 and 5 million women have an unmet need for PAC, in addition to the 5.6 million hospitalisations that occur annually.
Some of these women may be treated in non-formal or traditional medical systems and some may receive no treatment at all. Much of the abortion-related mortality takes place in this group of anonymous women. It is also likely that the inadequacies of formal health systems in low-income countries explain a large part of why a significant proportion of such women do not seek care or are unable to access it. Thus, the direct costs to the health system estimated in the previous section do not tell the whole story. If all the unmet demand for PAC were met by the health systems – in other words if the 3–5 million women who presently go untreated were to be treated, in accordance with the main goal of the ICPD – then the direct health-system costs would be much higher than the estimates given in section 4.
An idea of the magnitude of the increase in costs is shown in Table 5.1. If the cost-per-case method of estimation is used, another $293–$488 million would need to be spent by national health systems. If we use the MBP ‘bottom-up’ approach, an additional $277–$432 million would be needed to meet the unmet demand. Whatever the true size of the expenditure that would be needed to treat this largely unknown group of women, it is surely a sizeable proportion of the actual healthcare expenditures for PAC (Table 5.1) and points up a critical shortcoming in the current delivery of health services in the developing world. With no regional data available, Table 5.1 merely uses global estimates of unmet need to calculate regional costs. However, if regional data were available, it might well show that costs would increase disproportionately in regions such as sub-Saharan Africa where health systems are poorly organised.- 5 Other costs: review of evidence, methods and assumptions pp.29, 33
- Besides the costs to health systems for treatment of the estimated 5.6 million women receiving care in a hospital setting, there are many other women who suffer from minor complications that can be treated at the primary healthcare level or privately. Very little is known about how many of the 19.8 million women experiencing unsafe abortion each year fall into this category. One study (Benson and Crane 2005) has roughly estimated their number at 1 million women, based on their survey of several small-scale country studies. Pain management, treatment for anaemia and counselling are typical treatments that could be delivered at this level of care.
Unfortunately, no empirical study was found that had cost data on minor complications. In lieu of better data, we can hazard a first approximation of the cost of treating minor post-abortion morbidities by assuming that a visit to a primary healthcare post by a woman with a minor post-abortion complication might cost about the same as the average of the other health interventions of the Mother-Baby Package. The costing model developed by the WHO for the MBP has standard default values (which were estimated by a panel of WHO experts and calibrated based on conditions in rural areas of Uganda) that can be used to obtain a proxy value of the cost per case for women attending primary healthcare facilities for MBP interventions. The MBP models basic reproductive healthcare at three service levels including the primary level (‘health posts’ and ‘health centres’).
Table 5.2 gives details of the costs of individual MBP interventions for the available country applications of the MBP costing spreadsheet. Using these results we can calculate average costs of primary healthcare visits across a variety of maternal and newborn interventions for sub-Saharan Africa and Latin America and Caribbean. These averages are shown in the third and fourth columns of Table 5.3. For sub-Saharan Africa, the average MBP-related visit costs $7.58 actually and would cost $14.55 if WHO standard protocols were followed. For Latin America and Caribbean the estimated average costs are $40 and $58, respectively. Since there are no empirical data available for other regions, we assume that average costs in those regions are simple averages of the SSA and LAC regions. Using the Benson-Crane estimate of one million cases of minor post-abortion complications annually, regional shares are calculated to mirror regional proportions for hospital admissions.
For the developing world as a whole, we estimate that minor complications of unsafe abortion cost about $23 million each year. If WHO standards for treatment were followed, the global cost would rise to about $36 million. As a simple test for the sensitivity of these results to different assumptions, we take as lower-bound cost estimates those where all regions except the LAC region have costs per case equivalent to those in the SSA region. Upper-bound cost estimates, likewise, are those where all regions except the SSA region have LAC-level costs per case. As can be seen from Table 5.3, this results in a range of estimated global cost totals of $13.6 to $33.2 million. If countries followed WHO standards, the global-cost range goes from $22.7 to $49.1 million. These costs may be borne by the public healthcare system if primary healthcare is provided without charge to all women, while the costs may represent out-of-pocket expenses to women or households in settings where such care is provided privately. In other situations, these costs might be shared between a partially subsidised public health system and private contributions.- p.33
- One of the most important long-term disabilities associated with unsafe abortion is secondary infertility resulting from serious complications, including acute infections or uterine perforations. The incidence of post-abortion secondary infertility is not well documented, but recent work at WHO has estimated the proportion of women suffering from infertility as a result of unsafe abortion in the range of 3–12 per cent depending on region (Åhman et al. 2005). From these data, it is possible to obtain rough estimates of the numbers of women suffering from post-abortion infertility.
We can safely assume that very few women in developing countries, except those coming from the highest income strata, are able to seek infertility treatment, given the high cost of techniques such as in vitro fertilisation, which, in developed countries, can easily cost several thousands of dollars. Also, in developing countries, infertility treatment within public health systems is virtually unknown. We can conclude with certainty that almost all women who suffer from infertility as a consequence of unsafe abortions belong to the group of women with an unmet need for infertility treatment. However, it has been suggested (IDS 2007) that in some societies and in certain circumstances – e.g. in cases of powerlessness to use contraception – some women may resort to unsafe abortion as a form of contraception, calculating that the procedure may lead to infertility, an outcome that these women desire. Thus, even if we know how many women suffer infertility as long-term sequelae of unsafe abortion, we do not necessarily know the proportion of these women who desire to be treated if such treatment were available to them. Obviously, this is an important question that will need empirical research before it can be answered.
No studies on the cost of infertility treatment in a developing setting have been carried out. In fact, such studies in developed countries are rare. Only one source was found describing costs in a developed country (Finland) of successful in vitro fertilisation (IVF) for infertile couples (Koivurova et al. 2004). In the study, the estimated cost for a successful IVF treatment was 3,291 euros (2003). This cost was reduced to 3,181 euros by excluding the cost of a three-day sick leave, then converted into US dollars (2006), using an exchange rate of 0.90 and an inflation factor of 9.55 per cent over the period (US GDP deflator index). The resulting cost was $3,870. Note that this cost does not include the cost of any unsuccessful IVF treatments. Thus, this average cost underestimates the real cost since it assumes, unrealistically, that all women become pregnant from their first treatment.
From the estimate of infertility morbidity given by Åhman et al. (2005), there may be 1.5 million women annually who become infertile after unsafe abortions. If treatment costs around $4,000 for each of these women, then the potential cost of the global unmet need for infertility treatment could amount to $6 billion each year.17 This estimate would decrease if we could factor in the proportion of infertile women who would not want to be treated, but at the same time it would increase if could estimate the average number of IVF treatments needed before a successful pregnancy occurs.
Even though infertility treatment has almost never been part of the reproductive health services of public health services in the developing world – meaning that only the wealthiest strata can afford treatment – it is nevertheless important to highlight the magnitude of the cost that would be incurred if every case of post-abortion infertility were to receive adequate treatment. Although lack of data prevents precise estimation of this cost, there is no doubt that it is a very substantial amount indeed.- p.34
- In the calculations of health-system costs presented in previous sections of this report no attempt was made to separate costs borne by the public health system from those borne by the patient or the household to which she belongs. Regarding treatment costs, in some cases health systems have a well-defined schedule of co-payments which patients must pay as part of the service. In other, less well-organised systems, many of the costs that are formally contributed by the public system are in fact often borne by the patients themselves. For example, supplies and medicines may be habitually out-of-stock in public hospitals, so individuals must purchase these items on their own prior to receiving treatment. Thus, some double-counting may occur if patients’ out-of-pocket expenses are added to estimated total treatment costs. It is interesting, nonetheless, to examine out-of-pocket expenses on their own, since they may be an onerous cost from the woman’s viewpoint, particularly if her household income is low to begin with.
The out-of-pocket expenses of women seeking PAC are not confined to incidental (or not so incidental) expenses associated with the treatment itself. They also include such expenses as transportation costs to and from the health facility, food and lodging while awaiting treatment, income foregone while seeking treatment, during treatment and after treatment during the recuperation period, as well as any income foregone by other household members while caring for women with post-abortion complications. To date, very little data have been collected on such costs.
The studies that do provide some partial data on out-of-pocket costs are shown in Table 5.4. As can be seen in the table, the ten such studies primarily provide data on out-of-pocket expenses associated with the PAC treatment itself. The same is true of productive days lost: almost all studies have reported time lost in terms of average length of stay, usually in hospitals, while the treatment was administered. Only the 1980 study in Thailand reported on days lost before, during and after treatment. The Cambodia study reported on all three time periods but provided only aggregate results.
The data presented in Table 5.4 are obviously limited in geographical coverage. Eight of the studies took place in sub-Saharan Africa, the other two in Asia. None have been carried out in Latin America and Caribbean, northern Africa or Europe. The quality of the data is also suspect. For example, the Nigerian and Cambodian studies both measured out-of-pocket treatment costs, but in Nigeria these costs amounted to $104 whereas in Cambodia the cost was only about $7. The two sets of studies in Senegal, too, show quite different out-of-pocket cost ranges (e.g. from $16 to $75 for women seeking PAC during the pre-test phase of the studies) even though they employed similar methodologies.
Average-length-of-stay data, on the other hand, show much less variation, with an average of 1.6 days. However, a better estimate of average length of stay (ALOS) may be obtained from a wider set of studies that report ALOS even though they do not report on out-of-pocket expenses. Annex Table A4 compiles ALOS from 38 articles (some of which contained more than one sample), including the ones listed in Table 5.4. The average length of stay over all these studies – which include some studies sampling women with severe complications necessitating longer hospital stays – is 3.3 days.
Given the paucity of data, it is not yet possible to get a complete picture of out-of-pocket costs associated with the treatment of post-abortion complications. We have some data, mainly for parts of sub-Saharan Africa, on treatment expenses borne by the woman herself or her household as well as average length of stay during treatment. African data suggests that SSA total out-of-pocket expenses for PAC treatment may amount to just under $200 million. Except for the dated Thai study, however, we have no information on productive days lost before treatment, transportation, food and lodging costs, or on productive days lost by the woman and other household members during the convalescence period. The Thailand data suggest that the before and after periods may account for the majority of lost income from post-abortion complications compared with the time lost during the treatment itself. Extrapolating the Thai data to all developing countries, foregone income before, during and after treatment may total more than $400 million. With so many missing pieces of information, nevertheless, estimating global or regional out-of-pocket costs is little more than guesswork.- pp.36-37
- The costs of UARMM to public health systems are not the only costs occasioned by post-abortion complications. Certain other costs are borne by the affected women themselves or by the household in which they live. One such indirect cost of abortion-related mortality is the cost of orphanhood. Several studies of orphanhood costs after AIDS-related deaths of parents are available, which could serve as models for costing this aspect of UARMM. Another indirect cost is the negative effect on children’s future prospects, mainly through losing out on educational opportunities, but also via the negative effects of chronic poor health and nutrition. In all these cases, the causal chain would run from either crippling household costs from treatment, or from the death of the mother or from her long-term disability, to reduced expenditure on education, health or food. Finally, there are psychological costs as well. Secondary infertility in many settings is extremely damaging psychologically and stigmatising to the woman. Chronic PID, teratogenicity and dyspareunia can also cause marital stress and lead to psychological trauma.
The costs of orphanhood have been most widely studied, mainly with regard to AIDS. There are some theoretical issues, however, which need to be resolved before including such costs here. Researchers in the HIV/AIDS area have generally used the concept of ‘effective orphanhood’ based on findings that show that a large percentage of children do not live with the father after the death of the mother. In the case of women’s abortion-related deaths, where there would generally be a surviving father, it is not clear that the same approach would be appropriate. Moreover, given the extensive fostering arrangements prevalent in many cultures, it is difficult to say what proportion of such children are really orphaned, since fathers may still be supporting the children via payments to the foster parents. Another conceptual problem is that a child, whether orphaned or not, is a consumer of basic commodities such as food, clothing and education. In this sense, the orphaning of a child does not incur any additional costs. It is only a question of who bears the costs: the family, foster parents or the state. Knowing what extra obligations the state takes on when orphans are created through abortion-related mortality would be interesting from a policy perspective, but better measurement of real orphanhood rates would first need to be made.
Another indirect cost is an intergenerational effect, namely, the lower productivity of children – and hence a lower future income stream – as a result of less education and/or poorer nutrition and health occasioned by UARMM of mothers. At this point, however, no empirical studies linking UARMM with changes in schooling or nutrition of children have been done. If a quantitative linkage could be documented, estimation of this impact on future income would be possible and worthwhile.
The psychological impact of unsafe abortion – another indirect cost – has been studied even less thoroughly despite its obvious importance. Even if the mental health aspect of UARMM had been adequately researched, it might still prove to be an intractable undertaking to translate psychological costs into monetary terms for a costing study such as the present one. Another indirect cost, for which little or no data are available, is the monetary and/or social costs of infertility aside from the treatment costs dealt with earlier. Another indirect cost, which at present can only be speculated upon for lack of data, is the cost in terms of lost productive time to caregivers looking after women with PAC.- p.37
- Death and disability affect a country’s economy chiefly by lowering labour productivity and by lessening savings and investment. Bloom et al. (2005) explains that:
...healthier workers have better attendance rates and are more energetic and mentally robust. Workers in healthy communities, moreover, need to take less time off to care for sick relatives. Body size, which is greatly influenced by one’s health during childhood, has been found to have large impacts on long-term productivity. (Bloom et al. 2005: 32)
Furthermore, they calculate that ... a one-year increase in life expectancy improves labour productivity by 4 per cent. (Bloom 2005 et al.: 32)
Health also impacts the economy through its effect on savings and investment:
Healthier people expect to live longer, so they have a greater incentive to save for retirement. They are also able to work productively for longer, giving them more time to save. Workers and entrepreneurs therefore have a larger capital base to draw on for investment, leading to greater job creation and higher incomes. The savings booms in the East Asian ‘tiger’ economies in the last quarter of the 20th century were largely driven by rising life expectancy and greater savings for retirement. (Bloom 2005 et al.: 32)
In this report, we follow the approach of Bloom et al. (2005) in valuating the gains to the economy through the mechanisms just described. Building on prior work by Weil (Weil 2005), Bloom calculated the gains accruing to better survival through better health: ‘... each extra surviving adult in a group of 1,000 boosts income per capita by 0.119 per cent’ (Bloom et al. 2005: 35).- p.38
- We first look at the impact that abortion-related mortality has on the economy or, conversely, the added economic benefits that would accrue in the absence of abortion-related deaths. Around 66,000 such deaths occur each year in the developing world (see Table 5.5). In order to make use of Bloom’s estimate of gain in per capita income from a reduction in mortality, we must estimate the number of additional women surviving to age 60 if all abortion-related deaths were eliminated.
As an example, if a woman who would have died from an unsafe abortion at age 28 instead does not die, then her future productivity will incrementally add to per capita income. However, not all such women would survive to age 60 (the terminal year that Bloom et al. 2005 use in their calculations). In fact, the number of such women who will live to at least age 60 would be reduced due to the pattern of normal mortality, which can be found in life tables. Once we calculate the number of women who would live to age 60, we can estimate the positive impact on per capita income using the relationship suggested by Bloom et al. (2005).
Thus, the first step in measuring the impact of mortality is to make the simplifying assumption that in each region, all abortion-related deaths occur at the observed average age of unsafe abortion. Data on age patterns are available (Shah 2004) and are shown in column 4 of Table 5.5. Unsafe abortions occur at relatively young ages in Africa, older ages in Asia, and intermediate ages in Latin America. There are no data on the European age patterns. We assume that the Asian pattern of relatively late abortions is followed in Europe. So few abortion-related deaths occur in Europe that the effect of mis-estimating average age at death will in any case be negligible. Notice that we are also assuming that the age pattern of abortion-related deaths mirrors the age pattern of unsafe abortion. Lack of data on the former practically necessitates making this assumption, but it should be recognised as another potential source of error.
We therefore assume that all abortion-related deaths occur at the mean age of unsafe abortion. For Asia, for example, all 28,550 deaths are assumed to occur to women aged 28.87 years. Using survival rates for the various sub-regions within Asia, we then calculate how many of those women, if they had not died from abortion complications , would have survived to age 60. Column 5 of the table shows the number of these hypothetical survivors: about 48,000 of the 66,000 women would survive to age 60 if they did not die from unsafe abortion.
Once we know the number of additional surviving women, it is a simple matter to apply the Bloom et al. (2005) analysis. The impact on income is shown in the last four columns of Table 5.5. As is evident, with such small incremental numbers, per capita income increases by an insignificant amount – only one US cent or less – depending on the region. For all developing regions combined the estimated cost of premature death due to unsafe abortion, in terms of lost productivity, is about $28 million (2006 International dollars). International dollars are constructs using purchasing power parity (PPP) measures that allow better international comparisons. International dollars, however, are far greater than US dollars, especially for low-income countries. The final column of Table 5.5 converts International dollars to US dollars (2006); the total mortality effect on total income thus being reduced to US$9.3 million.- pp.39-40
- Aahman et al. (2005) estimated that 16.5 per cent of women with unsafe abortions develop chronic PID.
- Footnote 26, p.40
- The long-term health consequences of abortion complications have not been well studied. Among those noted in the literature (see Annex Table A1) are secondary infertility, hysterectomy, severe anaemia, and pelvic inflammatory disease (PID). Empirical data on the incidence of these long-term morbidities, however, are almost non-existent. The only source of quantitative information on post-abortion morbidities comes from the World Health Organization. A WHO report (Åhman et al. 2005) gives global estimates for both secondary infertility (see section 5.3 above) and PID. 26 According to this report, between 15 and 30 percent of women having unsafe abortions develop reproductive tract infections (RTI) which can lead to secondary infertility as well as PID. The study estimates the incidence of infertility at 3–12 per cent of these women. Furthermore, from the WHO/World Bank Global Burden of Disease project, disability weights for infertility and chronic RTI are available.
Using these sparse empirical estimates as a starting point, it is possible to approximate the effect that unsafe abortions have in lowering the productivity of women who subsequently suffer long-term morbidities (at least the two that are identified in the Global Burden of Disease (GBD) work). To estimate the indirect cost of decreased functioning, we assume that the disability weights given by the GBD are reasonable proxies of the reduced productivity of women suffering from those disabilities. For example, a woman suffering infertility sequelae has a GBD disability weight of 0.18 (Lopez et al. 2006). In a setting where the woman’s average income is, say, $1,000 per annum, the value of lost income due to her disability would be estimated at $180 per year.
Valuating the income foregone in such circumstances is difficult, since much work done by women is performed within the household and hence its cost is not available to statisticians as would be work performed for formal remuneration. Goldschmidt-Clermont (1993; and Goldschmidt-Clermont and Pagnossin-Aligisakis 1995) found that the value of non-market time, in industrialised countries, is half the value of GDP and that the contribution of non-market production to private consumption amounted to 60 per cent. In developing countries these percentages should be even higher, given the greater importance of non-monetised household production in developing settings. However, to the extent that women having abortions come from lower-income strata (this needs further research), using per capita income would tend to overestimate the total loss of income, since such women would have, on average, lower incomes. On the other hand, if women’s non-monetised productive activities could be valuated and included in the measurement of GDP, per capita GDP would then be much higher than it presently is. Given these offsetting tendencies, we assume here that the value of a woman’s work is equivalent to the national per capita income of the country in which she lives.
Since the empirical evidence on morbidity incidence is weak, we calculate central estimates of the numbers of women suffering long-term disability effects using WHO’s suggested rates, as well as lower-bound and upper-bound estimates to form ranges within which we can be more confident that the true incidence numbers lie. In the case of secondary infertility, WHO assigns incidence rates of 3, 5, 8 and 12 per cent of unsafe abortion cases to specific WHO regions, so we also vary the incident rates by sub-region. For the lower bounds, we use the following rates, respectively: 3 per cent (no change), 4.5 per cent (a drop of 10 per cent), 6.4 per cent (a drop of 20 per cent) and 8.4 per cent (a drop of 30 per cent). This pattern assumes that the higher reported incidence rates, which occur in low-income sub-regions, are the most likely to have been over-estimated. For the upper bounds of infertility incidence, we use, respectively, 4.5 per cent (an increase of 50 per cent), 6.5 per cent (an increase of 30 per cent), 9.2 per cent (an increase of 15 per cent) and 12 per cent (no change). The reasoning behind this pattern is similar: the high reported incidence rates are unlikely to be underestimated, while the low rates are more likely to be. Obviously, the patterns chosen for determining range boundaries are to an extent arbitrary, but will likely include the correct overall incidence rates.
There is even less certainty in the case of the WHO estimates of RTI incidence among women having unsafe abortions, which WHO gives as between 15 and 30 per cent (Åhman et al. 2005). For the central estimates of the numbers of women with this disability, we apply the lower percentage to higher-income sub-regions and the higher percentage to low-income sub-regions. We estimate the lower range boundaries by using an incidence rate of 15 per cent for all sub-regions. For the upper boundaries, we apply a 30 per cent incidence rate across all sub-regions.- pp.40-41
- The GBD disability weight for infertility is 0.180, meaning that on average a women suffering from infertility is physically disabled for 18 per cent of her life post facto. The disability weight for chronic RTI is 0.067 (Lopez 2006).
- Footnote 27, p.41
- Table 5.6 shows estimates of the impact of lower productivity on economic output. Out of 19.8 million women experiencing unsafe abortions annually, around 4.6 million are estimated to suffer from long-term PID and a further 1.6 million from secondary infertility (central estimates). For infertility morbidity, we estimate that the range that likely includes the true incidence figure goes from 1.2 million to 1.8 million women. For RTI/PID incidence, the range is from 3 million to 5 million women. This wide range seems appropriate given the weakness of the incidence rate estimates.
In the two lower panels of Table 5.6 we apply GBD disability weights to the incidence numbers and multiply by per capita income (using GDP per capita as a proxy).29 The middle panel uses International dollars (2006), which are preferable when one wants to make inter-regional comparisons, while the lower panel uses US dollars (2006), which better reflect actual in-country costs. We estimate that infertility morbidity costs between $340 and $495 million over a one-year period, the central estimate being $419 million. For RTI long-term morbidity, the estimated range is $380–$760 million and the central estimate is $503 million. Combining the two long-term morbidities, disability caused by unsafe abortions may cost from $720 million to $1.2 billion in lost income and production measured over one year. However, since we have no data on the extent to which these two disabilities might overlap, adding together the estimated costs of the two quite likely over-estimates the total cost. For example, if 50 per cent of all women suffering from post-abortion infertility also suffered from long-term PID, then the combined range of cost estimates would be lower: $550 million to $1 billion.
In this estimation of costs, we account for only one annual cohort of women undergoing unsafe abortions and evaluate the economic cost over a period of only one year. But each year, about 19 million women suffer the same fate. To the extent that long-term disabilities persist for longer than one year – which is very likely – there would be a multiplier effect of women from previous years whose productivity was still adversely affected by lingering disability. Without better data on how these disabilities persist over time, however, it is not possible at present to include a multiplier in these cost estimates. It is safe to say, however, that the cost estimates presented in Table 5.6 are substantial underestimates of the true cumulative economic costs.
Methodological note. Table 5.6 shows estimates only for the major developing regions. However, since the morbidity patterns of infertility vary significantly within sub-regions, as do per capita income averages, we have performed the calculations described above for 15 sub-regions and then aggregated results to the large regions.- p.43
- The purpose of this report was to develop methodologies to estimate the costs, in monetary terms, of unsafe abortion-related morbidity and mortality in developing countries. We formulated a framework for the analysis of costs related to unsafe abortion and were able to examine a number of specific costs by marshalling the available empirical evidence, scanty though it is in many areas. In the face of empirical data limited both quantitatively and qualitatively, it is important to be able to make reasonable, if imprecise cost estimates since they may be of great use in developing health policy to confront the problem of unsafe abortion.
Most emphasis was placed on estimating costs to health systems of treating the complications arising from unsafe abortion, both because more data exist in this area than in other costing areas and because such estimates are of immediate policy relevance. Even though at least 24 empirical studies are available on these costs, they are unevenly spread across regions, being few in Asia and Europe. Even within regions they tend to be concentrated in a few countries. The most important data limitation, however, is the very wide range of costs reported. Our analysis revealed several probable causes for this variation and the methodology we employed was designed to take these limitations into account. Future research should be more careful to specify clearly which cost components are being measured and which are not. It would also be very useful for future studies to adopt the three-category typology of abortion complications proposed be Kay et al. (1997) and Rees et al. (1997) so that more precise cost estimations may be made. An even better approach would be to collect cost data by each main type of complication.- 6 Conclusions, p.44
- With appropriate caveats for data limitations, global cost estimations were arrived at for several different aspects of the total economic impact of unsafe abortion. Considering only central estimates, these include:
$555 million – health-system costs for PAC (cost-per-patient ‘top-down’ approach)
$463 million – health-system costs for PAC (MBP costing model ‘bottom-up’ approach)
$373 million – notional health-system cost, if unmet need for PAC were to be met
$23 million – cost of treating minor complications of unsafe abortion
$6 billion – possible cost to treat all post-abortion infertility cases
$200 million – out-of-pocket expenses in sub-Saharan Africa for PAC treatment
$400 million – out-of-pocket expenses for income lost before, during and after treatment
$9 million – economic cost, in lower productivity, from mortality due to unsafe abortion
$419 million – economic cost, in lost income, from long-term disability due to infertility caused by unsafe abortion
$503 million – economic cost, in lost income, from long-term disability due to PID caused by unsafe abortion.
With respect to minor complications costs, very little hard data are available to estimate these costs, either in terms of the prevalence of such complications or in terms of the cost-per-case of treatment. We compiled all available data and used results from MBP costing applications to make rough approximations of costs in this area. Despite the dearth of data in this costing area, it seems that this cost component is not of major importance from a policy perspective.
With respect to infertility treatment costs, even though infertility treatment is supposed to be an integral component of reproductive care, in fact it is not. Developing countries in particular do not give it high priority, because treatment is very expensive and because the advanced technology required is often unavailable. The incidence of secondary infertility after unsafe abortion has not been measured with much precision and for treatment costs one has to rely on evidence coming from developed countries. Despite these limitations, it seems clear that addressing this reproductive health issue would be very costly, perhaps even costing more than hospital-based treatment of immediate complications.- pp.44-45
- Besides direct treatment costs, the report also examined indirect costs to the national economy and/or to the income of the household. The total estimated cost of foregone income as well as out-of-pocket expenses are quite large. However, the data underpinning the estimates are largely inadequate, except for data on length of hospital stay. Only one study was found that looked at both the time prior to treatment when the affected woman would be unable to work as well as the time after treatment when the woman would be recuperating and too weak to work. The whole issue of valuating women’s work, especially in developing settings where so much of it is ‘non-market’ employment, is complex and not yet satisfactorily solved. In the estimates in this report, it was assumed that non-market work has the same value as work in the formal sector. Lacking more precise data, we have also assumed that the income pattern of women who have unsafe abortion is the same as the pattern for all women, which may result in overestimating this impact. In the area of economic impact of mortality, we have relied on general health-economics studies, assuming that abortion-related deaths affect the economy in the same way as deaths from other illnesses. Confirmation of this, through UARMM-specific studies, would be desirable. At any rate, the methodology we employed showed that abortion-related deaths do not seem to have a significant impact on the economy through productivity losses.
- pp.45
- These costs of UARMM should not be lumped together, moreover, because the uncertainty of the estimates varies greatly from one to another due to limitations of data and the assumptions that underlie them. The methodologies used to estimate these different costs needed to accommodate several data deficiencies and their accuracy can only be verified once further empirical studies have furnished better information concerning the prevalence of different levels of complication as well as the precise costs of treating those complications. A theoretical issue concerning the valuation of women’s work in non-market settings must also be resolved before greater confidence can be placed in the accuracy of costing the impact of abortion-related morbidity. Despite these limitations, however, the costs presented in this report demonstrate substantial impacts on public health systems as well as for individuals and households.
- p.46
"The cost of post-abortion care in developing countries: a comparative analysis of four studies" (October 2016)
[edit]Michael Vlassoff, Susheela Singh, and Tsuyoshi Onda (October 2016). "The cost of post-abortion care in developing countries: a comparative analysis of four studies". Health Policy and Planning. 31 (8): 1020–1030. doi:10.1093/heapol/czw032. PMC 5013781. PMID 27045001.
- Over the last five years, comprehensive national surveys of the cost of post-abortion care (PAC) to national health systems have been undertaken in Ethiopia, Uganda, Rwanda and Colombia using a specially developed costing methodology—the Post-abortion Care Costing Methodology (PACCM). The objective of this study is to expand the research findings of these four studies, making use of their extensive datasets. These studies offer the most complete and consistent estimates of the cost of PAC to date, and comparing their findings not only provides generalizable implications for health policies and programs, but also allows an assessment of the PACCM methodology. We find that the labor cost component varies widely: in Ethiopia and Colombia doctors spend about 30–60% more time with PAC patients than do nurses; in Uganda and Rwanda an opposite pattern is found. Labor costs range from I$42.80 in Uganda to I$301.30 in Colombia. The cost of drugs and supplies does not vary greatly, ranging from I$79 in Colombia to I$115 in Rwanda. Capital and overhead costs are substantial amounting to 52–68% of total PAC costs. Total costs per PAC case vary from I$334 in Rwanda to I$972 in Colombia. The financial burden of PAC is considerable: the expense of treating each PAC case is equivalent to around 35% of annual per capita income in Uganda, 29% in Rwanda and 11% in Colombia. Providing modern methods of contraception to women with an unmet need would cost just a fraction of the average expenditure on PAC: one year of modern contraceptive services and supplies cost only 3–12% of the average cost of treating a PAC patient.
- Four recent costing studies, which provide the best estimates of the cost of post-abortion care (PAC) to national health systems, show that costs per case vary widely, from I$334 in Rwanda to I$972 in Colombia.
- The components of PAC costs—labor, drugs/supplies, overhead and capital—also differ substantially among the four countries, showing that resource-allocation decisions are important in determining the efficiency with which PAC is provided to clients.
- The financial burden of PAC is considerable: the expense of treating one PAC case is equivalent to around 33% of annual per capita income in Uganda, 25% in Rwanda and 10% in Colombia.
- Providing modern methods of contraception to women with an unmet need would cost just a fraction of the average cost of PAC.
- In 2008, around 21.2 million unsafe induced abortions took place in the developing world (WHO 2011), and between 22 000 and 44 000 women died from abortion-related causes. In 2012, an estimated seven million abortions were cared for in health facilities in developing countries for medical complications that required medical treatment (Singh and Maddow-Zimet 2015). Post-abortion care (PAC) encompasses the treatment of many types of medical complications, the most common one being incomplete abortion, ranging to less common but much more severe ones such as sepsis and uterine perforation. Treating unsafe abortions, while essential for women’s health and survival, diverts health resources from other uses and is a significant burden to the health care systems in developing countries where 98% of all unsafe abortions occur (WHO 2011). At the same, it is a preventable phenomenon depending on access to safe abortion care or effective contraception. Therefore, there is both an interest and a need to estimate the cost of PAC to inform public discussion of unsafe abortion and to help policy makers more efficiently allocate resources (Vlassoff et al. 2009b).
The report Adding it up: the costs and benefits of investing in sexual and reproductive health (Singh et al. 2014) estimates the total health-system cost of providing PAC services in the developing world at US $232 million in 2014. Because many women need PAC but cannot access it—and those who do get medical care may not receive comprehensive quality care—providing all women in need with the WHO recommended standard of care would cost substantially more, an estimated $562 million. Unsafe abortion is a burden not only for health systems but also for women themselves and their households. A study in Uganda, where abortion is common despite being legally restricted and highly stigmatized, found that women having unsafe abortions spent on average US $49 in out-of-pocket expenditures for the procedure as well treatment of complications (Sundaram et al. 2013). For many of these women, similar to much of the developing world where unsafe abortion is prevalent, such expenditures are onerous given the prevailing low levels of income. *Until recently, few studies on the cost of PAC were available and they generally lacked a standard methodology, making their findings difficult to generalize (Vlassoff et al. 2009b; Shearer et al. 2010). In response to this knowledge gap, a coherent methodology has been developed, pilot tested and further refined in four successive country studies. This methodology, the Post-abortion Care Costing Methodology (PACCM), will be described in more detail below. The findings of the studies using PACCM provide the start of a consistent evidence base, comparable across countries and regions. While calculating the cost of unsafe abortion varies according to the frame of reference chosen (Vlassoff et al. 2008), PACCM adopts the perspective of national health systems, focusing on the financial burden that the treatment of post-abortion complications imposes on health systems.
Over the last five years, comprehensive national surveys of the cost of PAC to national health systems have been undertaken in Ethiopia, Uganda, Rwanda and Colombia using the PACCM approach. (Vlassoff et al. 2012; Prada et al. 2013; Vlassoff et al. 2014a,b) This study extends the research findings of these four studies, making use of their extensive datasets to thoroughly exploit the possibilities for comparative analysis. Our objective is to compare empirical results of the health-system costs of treatment of complications resulting from unsafe induced abortion from these country applications of the PACCM methodology. These studies offer the most complete and consistent estimates of the cost of PAC to date, and comparison of their findings not only provides generalizable implications for health policies and programs, but also allows an assessment of the PACCM methodology. - A key feature of PACCM is its coverage of both direct and indirect costs—overhead and infrastructure costs that, while not direct inputs into the provision of specific treatments, are nevertheless necessary for the provision of care in general. Indirect costs, in particular, have rarely been estimated in earlier costing studies (Vlassoff et al. 2009b). However, PACCM studies show that indirect costs are an important component of total PAC costs. Other work, not related to PAC costs, has also highlighted the importance of indirect costs. For example, a United Nations report estimated that in 2009 indirect (also referred to as non-medical) costs made up two-thirds of total reproductive health costs in Sub-Saharan Africa (United Nations, Economic and Social Council 2009).
- In all four countries access to legal abortion is highly restricted. However, in 2005 Ethiopia broadened the grounds for legal abortion and in 2006 new procedural guidelines considerably increased access to abortion de facto (Singh et al. 2010). Colombia also widened access to abortion in 2006 as the result of a ruling by the Constitutional Court of Colombia (Prada et al. 2011). As seen in Table 1, Uganda has a very high abortion rate—one of the world’s highest—while Ethiopia and Rwanda exhibit more moderate abortion rates. Colombia’s abortion rate of 39 induced abortions per 1000 women in 2008 is higher than the Latin American regional average of 32 (Sedgh et al. 2012). Around 23–29% of women undergoing induced abortion were treated for post-abortion complications in Uganda, Rwanda and Colombia, but only 14% in Ethiopia. This proportion depends on two factors: the proportion of induced abortions that result in complications that need medical care in a facility (which in turn depends on the number of abortions carried out in unsafe conditions) and the proportion of women with such complications who are able to access facility-based care. One or both of these factors likely play a role in the low proportion observed in Ethiopia.
The reported distributions of types of post-abortion complications show some variation among the four countries. Incomplete abortion, the least severe of the five complications analyzed, makes up > 85% of all post-abortion complications in Colombia, but only a little over 60% of them in Uganda. Conversely, perforations of the uterus, the most serious complication, are almost absent in Colombia but comprise around 3% of all complications in Uganda. In general, the severity burden is highest in Uganda and lowest in Colombia. Ethiopia and Rwanda fall in between these two extremes. - Two patterns are evident: in Ethiopia and Colombia doctors spend about 30–60% more time with PAC patients than do nurses; in Uganda and Rwanda however nurses spend 220–280% more time with patients than do doctors. These latter countries seem to be more successful at task shifting, although a relative shortage of doctors may also play a part. Also noteworthy is the greater involvement of technical personnel, mainly lab technicians, in Colombia (157 min) compared to the three African countries (<40 min on average). As an economically more developed country, one may speculate that more diagnostic tests are routinely performed.
- The fourth panel of Table 2 combines all the above cost components into estimates of labor costs per PAC case. These range from lower levels in the three sub-Saharan countries (I$42.80–I$58.20) to a much higher level in Colombia (I$301.30). Technical personnel and counselors in Colombia are relatively costly components of labor costs (being 3.3 times more than the four-country average), while nurses are relatively less expensive (1.7 times the average cost). Also noteworthy, doctors comprise 67% of the total labor cost in Ethiopia but only 38% of it in Rwanda. Conversely, nurses contribute 30% to direct labor costs in Ethiopia but 49% in Rwanda. The contribution of technical cadres (such as lab technician, sonographer, etc.) to labor costs is striking: in Ethiopia it amounts to only 2%, while in Colombia it accounts for 14% of labor costs.
- The second major component of direct costs is the set of physical inputs that are consumed in PAC treatments. These include drugs, medical supplies and materials as well as laboratory tests and procedures such as sonograms. Costs per PAC case for these inputs for the four countries, broken down by type of treatment, are shown in the upper panel of Table 3. The average cost of drugs and supplies is lowest in Colombia (I$79) and highest in Rwanda (I$115). In general, cost differentials between countries are not large, compared to differences in labor costs, and it is particularly notable that they are lowest in Colombia, on a purchasing power parity basis.
- Purely in terms of costs, Colombia does well in treatment of cases of incomplete abortion, which comprise the large majority of PAC cases, spending only I$41 per patient on drugs, supplies and tests, compared to I$116 spent in Rwanda and I$100 in Ethiopia. On the other hand, treating patients with shock in Colombia is more than ten times more costly (I$645) compared to Ethiopia where only I$62 is spent on physical inputs. However, from these data it is not possible to tell how far these differences reflect efficiencies in treatment—they may also indicate scarcity in availability of drugs, supplies and lab tests in lower-income settings.8 Overall, PAC in Colombia requires the least expensive bundle of physical inputs (I$79) compared to an average expenditure of I$93 across the four countries. Drilling down into the data on laboratory tests confirms this finding. For example, in Colombia patients being treated for incomplete abortion are given 0.3 hemoglobin tests and 0.3 white blood cell tests on average, whereas in Rwanda and Uganda such patients are given between 1.0 and 1.4 tests.
- Table 4 summarizes the six cost components identified in these studies and presents their estimates of the total cost per PAC case in international dollar terms. At I$972, the cost of treating unsafe abortion in the Colombian health system is by far the costliest. Keep in mind, however, that indirect costs were not calculated in the Ethiopian study. If indirect costs were taken to be the average percentage of total costs across the other three studies (61%), the total cost per case in Ethiopia would amount to I$345, in between the Uganda and Rwanda estimates. Using this estimate for Ethiopia, the average cost per case across the three Sub-Saharan African countries is I$362. Labor and overhead are the major cost drivers in Colombia (together they constitute 81% of the total cost), but less important in Uganda and Rwanda (22% and 46% respectively). The costs of drugs/supplies and the cost of capital, on the other hand, seem to be more important drivers of PAC costs in African settings.
PAC is costly on a per capita basis as seen in the last panel of Table 4. Treating a single PAC patient costs the equivalent of 11% of the annual GDP per capita in Colombia and an astounding 35% in Ethiopia and Uganda. Regardless of who pays and what subsidies exist, fully one third of the average annual productive output on one individual goes to offset the cost of to treating one PAC patient in Ethiopia and Uganda. When we compare cost per PAC case to the average annual expenditure in health, the financial burden of unsafe abortion is put into even starker relief. Treatment for one episode of post-abortion morbidity consumes more than three times the annual per capita expenditure on health in Uganda and more than five times in Ethiopia. Even in Colombia, expenditure on one PAC case is > 100% the average annual per capita spending on health. - In general, PAC costs are substantially higher than the cost of safe abortion procedures. In countries where abortion is legal or administratively permitted such as Colombia or Ethiopia, the differences in costs are worth noting: the average PAC cost per client in Colombia is I$972 versus an average cost of a safe abortion of I$313 (Prada et al. 2013); and in Ethiopia I$345 (PAC) versus I$190 (abortion procedure). A global study of all developing countries estimated that the average cost per PAC case was more than twice the average cost of safe abortion procedures . (Singh et al. 2014)
In many developing countries such a comparison cannot be made because abortion is illegal for the most part. Pregnancies may be terminated by induced abortion, but most unintended pregnancies can be prevented from occurring by using an effective method of family planning. In Table 4 (lower panel) we present estimated total one-year costs of contraception for the four PACCM countries, using data from the latest edition of the Adding It Up study. (Singh et al. 2014) When these costs, which range from I$26 to I$29, are compared to the PAC costs in Table 4, one sees a great advantage to preventing unwanted pregnancies through family planning over treating post-abortion complications, which costs health systems from I$334 to I$972 in these four countries.
Finally, it is worth comparing the cost of PAC to the cost of maternal and newborn health (MNH) in general, since PAC is one component of MNH. The national cost of MNH in Uganda (without PAC costs included) was estimated in 2008 at US$345 million (Vlassoff et al. 2009a), which, when extrapolated to 2012, becomes around I$990 million. The annual national cost of PAC in Uganda was found to be around I$42 million in 2012, a little over 4% of the MNH total (Vlassoff et al. 2014a). On a per case basis, however, an average MNH intervention in Uganda cost I$123 in 2012, while an average PAC case cost I$394 to treat. A similar comparison can be made for Ethiopia using estimates from Sundaram et al. (2010) and Vlassoff et al. (2012). National PAC costs in Ethiopia in 2012 are somewhat >3% of national MNH costs (annually I$54 million and I$1.6 billion, respectively). On the other hand, per case costs were estimated to be I$238 (PAC) compared to I$433 (MNH) in 2012. - In the developing world abortion is still largely prohibited, except for narrow legal indications and is still heavily stigmatized. Research in this subject area is thus fraught with difficulties in gathering reliable and complete data. Data on the cost of medical care to treat abortions complications are likewise scarce. However, more studies of the cost of PAC have recently become available, four of which apply a standardized methodology and well-specified descriptions of the cost components analyzed—two important factors that will allow us to use these four studies to begin building a body of comparable costing estimates.
While research into the cost of PAC is beginning to attract more attention, important gaps still remain. The most thorough studies available, national-level studies from Ethiopia, Uganda, Rwanda and Colombia, estimated average costs per PAC case of I$345, I$407, I$334 and I$972, respectively. A review of literature in 2007 estimated an overall average of I$414 per PAC case (Shearer et al. 2010). Our review of more recent literature from 2008 to 2013 found that the average cost per PAC case was I$347 for seven studies that included both direct and indirect costs. Thus, a body of consistent cost estimates is emerging. As for regional differences in PAC costs, a comparison of the four PACCM studies shows the cost of PAC to be substantially higher in Colombia than in the three African countries, but this may not be generally true of the Latin American region since earlier regional estimates showed little difference between African and Latin American average costs per case: I$392 and I$430, respectively (Shearer et al. 2010). These various estimates suggest that spending on PAC is an important financial burden. In the four PACCM countries, the cost of treating one post-abortion patient is considerable: around 35% of annual per capita income in Uganda, 29% in Rwanda and 11% in Colombia. This burden is particularly acute in Uganda where facility-based treatment for one PAC patient costs the equivalent of four month’s income for an average person. - The increasing use of medication (typically misoprostol) in treating incomplete abortion, the least severe and most common type of complication, will probably lead to lower PAC costs in the future. Studies citing costs of specific post-abortion treatments indicate that using medication for treating incomplete abortion may be only one-sixth as expensive as MVA (Foster-Rosales et al. 2003; Hu et al. 2010). A model-based study of abortion costs in Uganda found that task shifting could also reduce PAC costs. For instance, the study calculated that by instituting a suite of cost-saving measures, including task shifting and use of lower-level facilities when appropriate for the treatment of particular types of post-abortion complications, costs would be reduced by around 45% (Johnston et al. 2007).
The wide variation in labor costs (both medical and non-medical personnel) seen in the four PACCM studies also point to operational efficiencies which could be made in PAC delivery by sharing experiences across countries. This is particularly the case for Colombia, where doctor salaries are as much as seven times the salaries of their African counterparts, even after adjusting for purchasing power. Task-shifting should be considered in Colombia as well as measures to reduce the total amount of time that medical personnel spend on the various treatments. On the other hand, the study showed little variation in overall expenditure on physical inputs and hence offers no lessons to be learned for this cost component. We found that overhead costs in Colombia were far above those of the three African countries. While it is beyond the scope of this study to speculate on the causes of this large disparity, there does seem to be scope for cost-cutting measures in the case of non-treatment expenditures in Colombia. - One important policy response to high levels of unsafe abortion is to attack its root cause, unintended pregnancy, by promoting family planning. Around 40% of all pregnancies in developing countries are unintended and almost half of all these unintended pregnancies are terminated by abortion (Sedgh et al. 2014). At the same time, substantial rates of unmet need for contraception are reported in virtually all developing countries (Sedgh and Hussain 2014). In the three African PACCM countries, Ethiopia, Rwanda and Uganda, the latest findings on unmet need are 26, 34 and 21% of all women of reproductive ages (ICF International 2012). In Colombia, by contrast, where fertility decline has reached replacement level, unmet need stands at 8%. Providing modern methods of contraception to women with an unmet need for contraception would greatly reduce unintended pregnancies (except for a small number of pregnancies that would occur due to contraceptive method failure). The cost of doing so is just a fraction of the cost of PAC: in Ethiopia one year of modern contraceptive services and supplies is equal to 12% of the average cost of treating a PAC patient, in Rwanda 9%, in Uganda 7% and in Colombia 3%.11 Preventing unintended pregnancies would not only reduce health systems cost of PAC and the cost of abortion procurement to women and households, but would also bring great health benefits in the form of lower maternal morbidity and mortality, better infant health and broader intergenerational improvement. In the four countries with PACCM studies, providing contraceptive services for one year to a woman or couple cost only about one tenth as much as the cost of treating one PAC patient. It is our hope that the cost estimates provided in this article will stimulate policy discussion around these health issues.
In its latest report on unsafe abortion the World Health Organization estimates that 13% of maternal deaths are caused by unsafe abortion (WHO 2011). Policies that reduce unsafe abortion therefore are also important in efforts to lower maternal mortality and morbidity. One line of attack is to advocate for more liberal abortion laws. Even with a more liberal legal framework in place however, persistent value systems and the continued stigmatization of induced abortion may result in large proportions of abortions taking place clandestinely and under unsafe conditions. In Bangladesh, for example, even after more than three decades of national coverage by the government-supported menstrual regulation12 program, about half of all pregnancy terminations are still via the procurement of (illegal) induced abortion rather than through legal menstrual regulation (Singh et al. 2012). - In each of the four countries, we were able to rely on the results of existing studies of the incidence of induced abortion. Even so, some uncertainty exists around questions such as the percentage distribution of post-abortion complications, the proportion of women with post-abortion complications that do not or cannot access the health system and the split between induced and spontaneous abortions.
"Saving Nigerians from risky abortions" (April 7, 2008)
[edit]Andrew Walker (April 7, 2008). "Saving Nigerians from risky abortions". BBC News. Retrieved February 20, 2021.
- When she discovered she was pregnant, Faith stole a few thousand naira - about $40 - from her mother to pay for a secret abortion.
The 21-year-old wasn't ready to have a baby, she said.
She doesn't have enough money to look after a child as she earns only 300 naira per day, just over $2.5 (£1.30).
"They put iron inside me, it pains a lot," she said in a written answer to questions from the BBC.
"I was vomiting, and felt sad."
The "doctor" was not trained to perform abortions, and may not have been qualified at all.
Faith is fortunate to be alive.
Figures show that 10,000 women die every year in Nigeria from unsafe abortions, carried out by untrained people in unsanitary conditions.
That is 27 deaths every day.
According to the US-based Guttmacher Institute, that is one sixth of the total number of women who die worldwide from such procedures. - In Nigeria abortion is illegal unless the life of the woman would be at risk if she were to give birth.
But the Guttmacher Institute estimates that more than 456,000 unsafe abortions are done in Nigeria every year.
Some women go to traditional healers to terminate their pregnancies.
Methods include trying to break the amniotic sack inside the womb with a sharp stick. This causes infection and in extreme cases the tissue inside the body can start to die.
"They're pulling out intestines," says gynaecologist Dr Ejike Oji, of Ipas, an international organisation working to secure reproductive rights for women.
Another method is to pump a toxic mixture of fiercely hot Alligator chilli peppers and chemicals like alum into their bodies.
"The women go into toxic shock and die," Dr Oji said. - "Even if it was possible to get a legal abortion, many women would not be able to get a safe one," said Dr Francis Ohanyido, the president of the International Public Health Forum.
Medical facilities vary widely and it is almost impossible to guarantee quality."
Cultural taboos mean even if there was a clinic in their town, it would be impossible for most women to go there, he said. - About 750,000 women have abortions every year
60% of those are "unsafe"
20% are done by a traditional healer or the woman herself
"Report finds nearly half of all abortions worldwide are unsafe" (27 September 2017)
[edit]Ashley Welch (27 September 2017). "Report finds nearly half of all abortions worldwide are unsafe". CBS News.
- More than 55 million abortions take place globally each year, and nearly half — 25.5 million — are unsafe, according to a new study published in the medical journal The Lancet.
The study authors say the research, led by the World Health Organization (WHO) and the Guttmacher Institute in New York, highlights the need for safe access to abortion for all women to the full extent of the law, and for outdated, unsafe methods to be replaced.
"Even though it's difficult to measure and estimate something like abortion where data is limited, trying to get a handle at least of figuring out what the burden of unsafe abortion might be is important to begin to address the problem," study author Dr. Bela Ganatra, a scientist at the WHO's Department of Reproductive Health and Research, told CBS News. "As long as we keep it invisible, we're not going to be able to find solutions." - The overwhelming majority of unsafe abortions — about 97 percent — take place in Africa, Asia and Latin America.
In North America, 99 percent of procedures were considered safe.
The results also show that countries with high proportions of safe procedures were also more likely to have less restrictive abortion laws. - Ganatra said the less-safe category is seen "largely in regions of the world where women are using medications like mifepristone and misoprostol" — prescriptions drugs for ending a very early pregnancy — "by themselves outside of medical assistance because they don't have access to other ways of having an abortion. Now, these are very safe medicines but in these situations women have to use it without any guarantee about the quality of the drugs, without the appropriate information, or somebody to go to for support."
The least safe abortions were provided by untrained individuals using dangerous methods, including ingestion of caustic substances, insertion of foreign objects, or use of traditional concoctions like roots and herbs. - Globally, between the years of 2010 and 2014, the study found that approximately 55 percent of all abortions were considered safe, 31 percent were considered less safe, and 14 percent fell into the least safe category.
Nearly 88 percent of abortions in developed countries were safe, with the exception of Eastern Europe where the proportion of unsafe abortions was slightly higher, likely because of the use of outdated practices in that region, the researchers said.
In contrast, the proportion of safe abortions in most regions of Africa and Latin America was just 25 percent.
In Latin America, most were classified as less safe, which the authors attribute to the transition from more dangerous, outdated abortion methods to women using misoprostol outside of a health care setting.
The vast majority of abortions in Africa were categorized as least safe and were associated with higher risk of death.
The study's three categories provide "a much more nuanced way of looking at safety and it helps us to begin to think about what interventions might be needed in which region, depending on what type of unsafe abortions are prevalent in that region," Ganatra said. - WHO guidelines recommend that access to a safe abortion should be available to women at the primary-care level.
"It's something that can be provided as basic care by a range of health care workers," Ganatra said. "It's not a high resource, intensive, difficult-to-provide service, and yet because of all the other barriers that exist around this topic unfortunately unsafe abortion is still a problem."
Ganatra said that the findings also back up other research showing that laws restricting access to abortion will not result in fewer women getting abortions.
"Women are going to have abortions when they are faced with the situation where they need it and if they can't get access to safe ones they will go further down the spectrum to less safe and perhaps even dangerous," she said. - In an accompanying editorial published in The Lancet, Kristina Gemzell-Danielsson and Amanda Cleeve of the Department of Women's and Children's Health in the Division of Obstetrics and Gynecology at Karolinska Institutet in Sweden say the findings raise the questions for how WHO can work together with member states to increase access to safe abortion.
"It is remarkable that, despite being preventable, 25.1 million unsafe abortions were estimated to have occurred annually between 2010 and 2014, 97 percent in low-income regions," they write. "… It is time to implement evidence-based policies, programs, and services that promote, protect, and fulfill the sexual and reproductive rights of all individuals worldwide."
“Preventing unsafe abortion”, World Health Organization
[edit]- Around 25 million unsafe abortion were estimated to have taken place worldwide each year, almost all in developing countries.
- Between 2010–2014, on average, 56 million induced (safe and unsafe) abortions occurred worldwide each year.
- There were 35 induced abortions per 1000 women aged between 15–44 years.
- 25% of all pregnancies ended in an induced abortion.
- The rate of abortions was higher in developing regions than in developed regions.
- Among the 25 million unsafe abortions, 8 million were carried out in the least- safe or dangerous conditions.
- Over half of all estimated unsafe abortions globally were in Asia.
- 3 out of 4 abortions that occurred in Africa and Latin America were unsafe.
- The risk of dying from an unsafe abortion was the highest in Africa.
- Each year between 4.7% – 13.2% of maternal deaths can be attributed to unsafe abortion.
- Around 7 million women are admitted to hospitals every year in developing countries, as a result of unsafe abortion.
- The annual cost of treating major complications from unsafe abortion is estimated at US$ 553 million.
- Safe abortion must be provided or supported by a trained person using World Health Organization (WHO) recommended methods appropriate for the pregnancy duration.
- Almost every abortion death and disability could be prevented through sexuality education, use of effective contraception, provision of safe, legal induced abortion, and timely care for complications.
- p.1
- Abortions are safe if they are done with a method recommended by WHO that is appropriate to the pregnancy duration and if the person providing or supporting the abortion is trained. Such abortions can be done using tablets (medical abortion) or a simple outpatient procedure.
Unsafe abortion occurs when a pregnancy is terminated either by persons lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both.
The people, skills and medical standards considered safe in the provision of abortion are different for medical abortion (which is performed with drugs alone), and surgical abortion (which is performed with a manual or electric aspirator). Skills and medical standards required for safe abortion also vary depending upon the duration of the pregnancy and evolving scientific advances.
*Abortions are less safe, when done using outdated methods like sharp curettage even if the provider is trained or if women using tablets do not have access to proper information or to a trained person if they need help.
*Abortions are dangerous or least safe when they involve ingestion of caustic substances or untrained persons use dangerous methods such as insertion of foreign bodies, or use of traditional concoctions.- p.2
- Women, including adolescents, with unintended pregnancies may resort to unsafe abortion when they cannot access safe abortion. Barriers to accessing safe abortion include:
*restrictive laws;
*poor availability of services;
*high cost;
*stigma;
*conscientious objection of health-care providers; and
*unnecessary requirements such as mandatory waiting periods, mandatory counselling, provision of misleading information, third-party authorization, and medically unnecessary tests that delay care.- p.2
- Based on data from 2010-2014, there were approximately 25 million unsafe abortions annually. Of these, one third or approximately 8 million were performed under the least safe conditions by untrained people using dangerous and invasive methods. Unsafe abortions lead to an estimated 7 million complications.
In developed regions, it is estimated that 30 women die for every 100 000 unsafe abortions. That number rises to 220 deaths per 100 000 unsafe abortions in developing regions and 520 deaths per 100 000 unsafe abortions in sub-Saharan Africa.
Mortality from unsafe abortion disproportionately affects women in Africa. While the continent accountsfor 29% of all unsafe abortions, it sees 62% of all abortion-related deaths.- p.2
- Any woman with an unwanted pregnancy who cannot access safe abortion is at risk of unsafe abortion. Women living in low-income countries and poor women are more likely to have an unsafe abortion than more affluent women. Deaths and injuries are higher when unsafe abortion is performed later in pregnancy. The rate of unsafe abortions is higher where access to effective contraception and safe abortion is limited or unavailable.
- p.2
- Following unsafe abortion, women may experience a range of harms that affect their quality of life and well-being, with some women experiencing life-threatening complications. The major life-threatening complications resulting from the least safe abortions are haemorrhage, infection, and injury to the genital tract and internal organs. Unsafe abortions when performed under least safe conditions can lead to complications such as: * incomplete abortion (failure to remove or expel all of the pregnancy tissue from the uterus);
* haemorrhage (heavy bleeding);
* infection;
*uterine perforation (caused when the uterus is pierced by a sharp object);
*damage to the genital tract and internal organs by the insertion of dangerous objects such as sticks, knitting needles, or broken glass into the vagina or anus.- pp.2-3
- An accurate initial assessment is essential to ensure appropriate treatment and prompt referral for complications of unsafe abortion. The critical signs and symptoms of complications that require immediate attention include:
*abnormal vaginal bleeding;
*abdominal pain;
*infection;
*shock (collapse of the circulatory system).
Complications of unsafe abortion can be difficult to diagnose. For example, a woman with an extrauterine or ectopic pregnancy (abnormal development of a fertilized egg outside of the uterus) may have symptoms similar to those of incomplete abortion. It is essential, therefore, for health-care personnel to be prepared to make referrals and arrange transport to a facility where a definitive diagnosis can be made and appropriate care can be delivered quickly.- p.3
- Complications arising from unsafe abortions and their treatments include:
*Haemorrhage: timely treatment of heavy blood loss is critical, as delays can be fatal.
*Infection: treatment with antibiotics along with evacuation of any remaining pregnancy tissue from the uterus as soon as possible.
*Injury to the genital tract and/or internal organs: if this is suspected, early referral to an appropriate level of health care is essential.- p.3
- Health-care providers are obligated to provide life-saving medical care to any woman who suffers abortion-related complications, including treatment of complications from unsafe abortion, regardless of the legal grounds for abortion. However, in some cases, treatment of abortion complications is administered only on condition that the woman provides information about the person(s) who performed the illegal abortion.
The practice of requiring women seeking emergency medical care as a result of illegal abortion to provide information about the practitioner puts women’s lives at risk. The legal requirement for doctors and other health-care personnel to report cases of women who have undergone abortion delays care and increases the risks to women’s health and lives. UN human rights standards call on countries to provide immediate and unconditional treatment to anyone seeking emergency medical care.- p.3
- Unsafe abortion can be prevented through:
*comprehensive sexuality education;
*prevention of unintended pregnancy through use of effective contraception, including emergency contraception; and
*provision of safe, legal abortion.
*In addition, deaths and disability from unsafe abortion can be reduced through the timely provision of emergency treatment of complications.- p.3
- In addition to the deaths and disabilities caused by unsafe abortion, there are major social and financial costs to women, families, communities, and health systems. In 2006, it was estimated that $553 million was spent treating serious consequences of unsafe abortion. An additional $375 million would be required to fully meet the unmet need for treatment of complications from unsafe abortion.
- p.3
"The Prevention and Management of Unsafe Abortion" (April 1992)
[edit]"The Prevention and Management of Unsafe Abortion" (PDF). World Health Organization. April 1992. Archived (PDF) from the original on 30 May 2010. Retrieved 18 October 2017.
- Complications resulting from unsafe abortion are an important cause of maternal mortality and morbidity. On a country-specific basis deaths related to complications of unsafe abortion range from under 10% to almost 60% of maternal deaths. These statistics are all the more compelling as the majority of these deaths are preventable with currently existing, but not universally available, drugs, technologies and management systems.
The World Health Organization has assisted Member States for more than 25 years in addressing the public health concerns surrounding unsafe abortion, including awareness raising, identification of priority areas for intervention, prevention of unsafe abortion through family planning information and services, and training of health workers. At the Twentieth World Health Assembly in 1967, Resolution WHA 20.41, noted that “abortions…constitute a serious public health problem in many countries” and recommended that the Organization continue to work” in the field of health aspects of human reproduction”.- p.2
- An integral objective of the WHO maternal Health and Safe Motherhood Programme is that family planning information and services should be available, accessible and affordable to all. Unfortunately this ideal has not been universally attained. In addition, contraceptive methods may fail. As a result large numbers of women throughout the world continue to rely on abortion as a means to end an unwanted pregnancy. Too often these women are risking their lives and health when the services they find are unsafe. This need to rely on unsafe abortion signals a failure of health systems to provide appropriate care of these women who are seeking a means to control their fertility. Within every health care context when there is a threat to health, a moral obligation exists to assess its impact and to ensure that humane and appropriate care is available and accessible. In the case of unsafe abortion, women’s lives and health are clearly threatened.
The term “Unsafe Abortion” was used by the Technical Working Group to reflect concern for the safety of abortion services, which were the focus of its discussions rather than the legal issues surrounding abortion. Unsafe abortions are characterized by the lack or inadequacy of skills of the provider, hazardous techniques and unsanitary facilities. Unsafe abortion with its man resulting complications is responsible for the deaths and illness of hundreds of thousands of women each year. The legality or illegality of the services, however, may not be the defining factor of their safety. To prevent the deaths of women, the safety of abortion) whether elective induced abortion or the treatment of spontaneous or incomplete abortion) must be considered within both the legal and legally restricted contexts.
An effective mechanism for teaching women more promptly with the care they require for complications of unsafe abortion is for appropriate and timely care to be available as close to women as possible.- p.3
- The legal status of abortion by percentage of the world’s population affected imply the following statistics: 40% have access to abortion on request; 12% have access to abortion on grounds such as social, economic, or fetal indication; 23% have severely restricted access to abortion, usually only in cases such as saving the life of the mother; and for 25% abortion is prohibited through the health services on all grounds.
Even in countries where abortion services are ostensibly available (roughly 50% of the world), services may not be accessible to women or women may be unaware that services are available. As a result a large proportion of the world’s women are without access to safe termination of pregnancy.
In developed countries where safe abortion is readily available, abortion-related mortality is extremely low, at less than 1/100,000 procedures. In less optimal settings when women are only able to find unsafe abortion, mortality can be high.- p.4
- Exact numbers of deaths from unsafe abortion are difficult to determine, in large part because it is almost impossible to estimate accurately a) abortion rates (i.e. number of abortion per women of reproductive age) and b) case fatality rates (i.e. the number of abortion deaths per total abortions).
Data are usually derived from several sources, including hospital-based data, civil registration, and community-based data. Each of these sources can present a challenge to researchers for a variety of reasons, including lack of specificity of the cause of deaths, misclassification of the deaths, or reluctance to provide complete information.
Given the data available, however, a range of estimates emerges, from a minimum of 50,000 to 150,000 abortion-related deaths annually. Some researchers believe that the often quoted 200,000 abortion-related deaths per year, which may have been true several years ago, is now in fact lower. This potential decline in annual abortion-reated deaths may be attributable to safer abortion care being more widely available. Whatever the number, the fact is that our health systems continue to fail women by letting preventable deaths occur.- pp.4-5
- Care for complications of unsafe abortion must be extended throughout the health care system, particularly to the primary care level. Currently, many primary care centres do not provide any emergency stabilization or intervention for women with abortion complications prior to referral. Decentralization of services is essential, bringing with it more immediate life-saving care and preventing unnecessary deterioration in the woman’s condition when referral and transport is required.
A critical step in the process of expanding access to care is the creation of a continuous chain of care, with providers at each level understanding their role in this chain. Providers, particularly at the primary and first referral levels of care, must receive training which clearly identifies their essential role in the prevention of maternal mortality and morbidity from abortion complications.
Personnel at every level of care must recognize that complications from unsafe abortion are potentially life-threatening. Many women seeking care encounter health care providers who view this serious medical problem as a lower priority than other disorders. Training about the serious nature of abortion complications can help change these attitudes.- p.5
- The management of unsafe abortion has been neglected as an area of research. Needs for additional research were considered in the context of clinical research needs and operations research needs. It was the consensus that there are few needs for clinical research in the treatment of abortion complications. However, there are many areas of need for operations research in implementing improved service delivery throughout the health care system.
- p.8
- Throughout much of the developing world women who have experienced complications of an unsafe abortion, whether or not they have been fortunate enough to reach a health facility for treatment, often receive no contraceptive information or services. These cases represent one group of women at high risk of unwanted pregnancy and repeat unsafe abortion. When the health system fails to provide appropriate family planning services it must be counted as a missed opportunity to assist women in the safe regulation of their fertility.
A majority of both the clinical and service delivery studies which have been done with regard to post-abortion contraception have focused on issues unrelated to the specific circumstances of women who have been treated for complications of an unsafe abortion. Much of the clinical literature dates from the seventies and early eighties and, therefore, does not take into account newly developed or refined methods of contraception (e.g. Norplant, NET microspheres, new injectables, and multiphasic pills). In the area of the health system and its delivery of contraceptive information and services immediately following abortion, most of the existing literature is devoted to information and services following elective induced abortion.- p.13
- While barrier methods were considered generally acceptable following an unsafe abortion, the universal concern about condoms as a male method over which women have little decision-making power was reiterated.
In regard to IUDs, a specific concern is the possibility of increasing the risk or severity of infection. As many incomplete abortions are of uncertain safety and in many other cases infection is readily apparent, the Technical Working Group concluded that IUDs should not be recommended immediately following treatment of an unsafe abortion unless no other alternative exists. However, where the possibility of increasing the risk of severity of an infection appears to be minimal the IUD may be considered an acceptable method.
The Technical Working Group considered sterilization immediately following treatment for complications of unsafe abortion and arrived at the following consensus. There is considerable potential for later regret if a woman chooses a permanent method at the time of abortion. The Group acknowledged that delaying a sterilization procedure could (a) present interference with fully informed consent due to stress and/or physical impairment related to the circumstances of the unsafe abortion, and (b) limit the potential for coercion by the health care provider. The other side of the coin, however, is that women wanting sterilization must wait for it. Interest was expressed in gaining a clearer understanding of the optimal timing for delay of sterilization following an unsafe abortion to minimize regret.
All hormonal methods were considered acceptable for use following an unsafe abortion, and can be started following treatment, before the woman leaves the health facility.- p.14
- The causes of unsafe abortion are rooted in a complex set of circumstances which are not easily solved. Nevertheless, practical strategies are available to us now to prevent much of the maternal mortality which results from unsafe abortion. Clinical treatment protocols, appropriate technologies, and management systems can be combined and tested to find the most effective solutions for any health system. Assessing women’s preferences in the design of family planning services, including information and services following treatment of abortion complications, will identify mechanisms that more effectively meet women’s needs. This step can correct failures in existing programmes, preventing many unwanted pregnancies.
- p.17
Safe Abortion: Technical and Policy Guidance for Health Systems” (2003)
[edit](Abortion: Technical and Policy Guidance for Health Systems”. World Health Organization. (2003).
- The causes of maternal deaths are multiple. Women die because complications during labour and delivery go unrecognized or are inadequately managed. They die from diseases such as malaria, that are aggravated by pregnancy. They die because of complications arising early in pregnancy, sometimes even before they are aware of being pregnant, such as ectopic pregnancy. And they die because they seek to end unwanted pregnancies but lack access to appropriate services. Achieving the Millennium Development Goal of improved maternal health and reducing maternal mortality requires actions on all these fronts.
Despite dramatically increased use of contraception over the past three decades, an estimated 40-50 million abortions occur annually, nearly half of them in circumstances that are unsafe. Globally, approximately 13% of all maternal deaths are due to complications of unsafe abortion. In addition to some 70,000 women who die each year, tens of thousands suffer long-term health consequences including infertility. Even where family planning is widely accessible, pregnancies occur due to contraceptive failure, difficulties with use, non use or as a result of incest or rape. Pregnancy may pose a threat to the woman’s life or to her physical and mental health. In recognition of such circumstances, nearly all countries in the world have passed laws that permit termination of pregnancy under specified conditions. In some settings, abortion is legal only to save the woman’s life; in others, abortion is allowed upon request by the woman. Health systems need to respond accordingly.- p.7
- An estimated 46 million pregnancies end in induced abortion each year. Nearly 20 million of these are estimated to be unsafe.
- About 13 percent of pregnancy-related deaths have been attributed to complications of unsafe abortion, and probably number about 67,000 deaths annually.
- In developing countries, the risk of death following complications of unsafe abortion procedures is several hundred times higher than that of an abortion performed professionally under safe conditions.
- Complications resulting from unsafe abortion contribute to serious sequelae for women’s health such as infertility.
- Since no contraceptive is 100 per cent effective, there will continue to be unwanted pregnancies which women may seek to end by induced abortion.
- In almost all countries the law permits abortion to save the woman’s life and in most countries abortion is allowed to preserve the physical and mental health of the woman.
- Safe abortion services, as provided by law, therefore need to be available, provided by well-trained health personnel supported by policies, regulations and a health systems infrastructure, including equipment and supplies, so that women can have rapid access to these services.
- Chapter 1 Safe abortion services: the public health challenge, p.10
- On the subject of abortion in particular, at the Cairo Conference, Governments of the world recognized unsafe abortion as a major public health concern, and pledged their commitment to reducing the need for abortion through expanded and improved family planning services, while at the same time recognizing that, in circumstances where not against the law, abortion should be safe (United Nations 1995, paragraph 8.25). One year later, the Beijing Conference affirmed these agreements and also called for Governments to consider reviewing laws containing punitive measures against women who have undergone illegal abortions *United Nations 1996, paragraph 106).
The United Nations General Assembly review and appraisal of the implementation of ICPD in 1999 (ICPD + 5) further agreed that, “in circumstances where abortion is not against the law, health systems should train and equip health-service providers and should take other measures to ensure that such abortion is safe and accessible. Additional measures should be taken to safeguard women’s health.” (United Nations 1999, paragraph 63.iii)- Background, p.11
- Even if all contraceptive users were to use methods perfectly all the time, there would still be nearly six million accidental pregnancies annually. Thus, even with high rates of contraceptive use, unwanted pregnancies will occur which women may seek to end by induced abortion.
An unsafe abortion is “a procedure for terminating an unwanted pregnancy either by persons lacking the necessary skills or in an environment lacking the minimal medical standards, or both”(world Health Organization 1992). About 20 million, or nearly half, of the induced abortions annually are estimated to be unsafe. Ninety-five per cent of these occur in developing countries (World Health Organization 1998). Globally, there is a ratio of one unsafe abortion for every seven live births (World Health Organization 1998). Globally, there is a ratio of one unsafe abortion for every seven live births (World Health Organization 1998), but in some regions the ratio is much higher. For instance, in Latin America and the Caribbean, there is more than one unsafe abortion for every three lives births (World Health Organization 1998).- Unsafe abortion, p.12
- About 13 per cent of pregnancy-related deaths have been attributed to complications of unsafe abortion (World Health Organization 1998); when applied to the most recent estimate of maternal deaths worldwide (i.e. 515,000 for the year 1995); World Health Organization 2001), this percentage corresponds to about 67,000 deaths annually. In addition, unsafe abortion is associated with considerable morbidity. For instance, studies indicate that at least one in five women who have an unsafe abortion suffer a reproductive tract infection as a result. Some of these are serious infections leading to infertility (World Health Organization 1998).
Where access to abortion services is legally restricted, or where the law provides for abortion on many grounds but services are not fully available or are of poor quality, women who have money are nonetheless often able to buy medically competent services from the private sector. But many other women who have unwanted pregnancies are at particular risk of unsafe abortion. They include women who are poor, live in isolated areas, are in vulnerable circumstances (such as refugees or internally displaced women) or are adolescents, especially those who are not married. These women have less access to reproductive health information and services, they are often highly vulnerable to sexual coercion and violence, they may delay seeking abortion, and they are thus more likely to have to rely on unsafe abortion methods and unskilled providers (Bott 2001, Gardner and Blackburn 1996, Mundigo and Indriso 1999)- Unsafe abortion, p.14
- Almost all the deaths and complications from unsafe abortion are preventable Procedures and techniques for early induced abortion are simple and safe. When performed by trained health care providers with proper equipment, correct technique and sanitary standards, abortion is one of the safest medical procedures. In countries where women have access to safe services, their likelihood of dying as a result of an abortion performed with modern methods is no more than one per 100,000 procedures (Alan Guttmacher Institute 1999). In developing countries, the risk of death following complications of unsafe abortion procedures is several hundred times higher than that of an abortion performed professionally under safe conditions (World Health Organization 1998). Properly provided services for early abortion save women’s lives and avoid the often substantial costs of treating preventable complications of unsafe abortion (Fortney 1981, Shibangu et al. 1984, Figa-Talamanca et al. 1986, Mpangile et al. 1999).
- Safe abortion, p.14
- In almost all countries, the law permits abortion to save the woman’s life (Figure 1.1). In more than three-fifths of countries, abortion is also allowed to preserve the physical and mental health of the woman, and, in about 40 per cent, abortion is permitted in cases of rape or incest or fetal impairment. One-third of countries allow abortion on economic or social grounds, and at least one-quarter allow abortion on request (United Nations Population Division 1999). Thus, virtually all countries should have accessible and safe services in place to provide abortion where the law permits.
- Legal, policy and contextual considerations, p.14-15
- Making abortion safe and accessible to the full extent of the law requires training health personnel so that they are conversant with national laws and regulations as well as with technical procedures, ensuring equipment and supplies, and designing protocols, regulations and policies that promote access to quality abortion services.
- The challenge-making safe services available, p.16
- b) What is the incidence of legal abortion and of the complications of unsafe abortion? Who is using the current services, and who is not obtaining access?
Estimating the incidence of unsafe abortion, and the numbers of legal abortions currently carried out may be difficult, especially in situations where access to legal abortion is restricted. In almost all situations, however, social science studies often furnish data which can help to establish a general picture of the situation (Mundingo and Indriso 1999). Health service statistics can provide estimates of legal abortions and numbers of hospital admissions for complications of unsafe abortion. Survey data, for instance from DHS, may exist on the extent of unwanted or ill-time pregnancy. Where available, data on the age, marital and socio-economic status of women using legal abortions services and women suffering complications from unsafe abortions will give an indication of which women are currently using services. These data can then be used to tailor programme design.
*For example, if information about women treated for the complications of unsafe abortion reveals that they are in the under-25 age group, policy-makers an programme planners will need to develop strategies to provide young people with information and education about sexual and reproductive health and about availability of contraceptive and abortion services. Additional information about health providers’ attitudes may suggest further training for them to be open and non-judgmental with adolescents and young people.- pp.56-57
- Unsafe abortion is one of the main causes of maternal mortality and morbidity even though it is legal for a variety of circumstances in almost all countries. This is because safe abortions services are frequently not available even when it would be legal to provide them. The ICPD + 5 review and appraisal process agreed that, in circumstances where abortion is not against the law, “health systems should train and equip health service providers and take other measures to ensure that such abortion is safe and accessible”. Understanding the circumstances under which abortion is not against the law, and the related policy considerations, is crucial for implementing this mandate.
- Chapter 4 Legal and policy considerations, p.82
- The great majority of the deaths from unsafe abortion occur in developing countries where abortion is severely restricted by law (Alan Guttmacher Institute 1999). In develpig regions (excluding China), 330 deaths occur per 100,000 abortions, a mortality rate that is hundred sof times higher than the rate in developed countries. The rate is highest - an estimated 680 deaths per 1000,000 procedures - in Africa (Alan Guttmacher Institute 1999, World Health Organization 1998).
Most Governments have ratified legally-binding international treaties and conventions that protect human rights, including the right to the highest attainable standard of health, the right to non-discrimination, the right to life, liberty and security of the person, the right to be free from inhuman and degrading treatment, and the right to education and information.
In consideration of these rights, Governments ageed in the ICPD + 5 review and appraisal process that “…in circumstnaces where abortion is not against the law, health systems should train and equip healthservice providers and should take other measures to ensure that such abortion is safe and accessible. Additional measures should be taken to safeguard women’s health.” (United Nations 1999, paragraph 63.iii). A clear understanding of laws on abortion as well as related policy considerations is required to ensure that all women eligible under the law have access to safe services. Further, the majority of the world’s Governments at the 1995 Fourth World Conference on Women agreed they should “…consider reviewing laws containing punitive measures against women who have undergone illegal abortions.” (United Nations 1996, paragraph 106).- Women’s health and international agreements, p.83
- If official and “informal” fees for legal, safe abortion are high, they will increase the risk of recourse to unsafe abortion especially by poor women and others, such as adolescents, who do not have access to cash. Where fees for services and other charges are necessary, these should be kept as low and affordable as possible, and subsidies should be provided for those unable to pay. For public health services, the costs will likely be more than offset by the savings achieved by reducing unsafe abortion and the burden that complications of unsafe abortion impose on health systems.
- Service fees, p.89
"Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" "Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (2007)
[edit]"Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003" (PDF). World Health Organization. (2007).
- This report gives estimates of the number of unsafe abortions and associated mortality for the year 2003. Nearly 20 million unsafe abortions took place that year, 98% of them in developing countries with restrictive abortion laws. These countries often also have low rates of use of modern reversible contraceptives and high levels of unmet need for family planning. Regional and global estimates of the incidence rate of unsafe abortion (per 1000 women aged 15–44 years) and unsafe abortion ratios (per 100 live births) are presented. The report identifies areas where data on unsafe abortion are particularly scarce and estimates therefore tenuous. Trends in the estimated incidence of unsafe abortion are examined, and relevant background information is provided on the legal context of abortion, fertility transition, unplanned pregnancy, family planning and contraceptive method mix. The health consequences of unsafe abortion and their global burden for women and for society are discussed. This is the fifth update of this document since the first edition was published by WHO in 1990.
- Abstract
- Methods to terminate an unwanted or unintended pregnancy are known to have existed since ancient times. As far back as 5000 years ago, the Chinese Emperor Shen Nung described the use of mercury for inducing abortion. A recent publication lists over 100 traditional methods of inducing abortion, which can be broadly classified into four categories: (1) oral and injectable medicines; (2) vaginal preparations; (3) introduction of a foreign body into the uterus; and (4) trauma to the abdomen. Many of these methods pose serious threats to the woman’s life and well-being.
Each year, throughout the world, approximately 210 million women become pregnant and some 130 million of them go on to deliver live-born infants. The remaining 80 million pregnancies end in stillbirth, or spontaneous or induced abortion. Approximately 42 million4 pregnancies are voluntarily terminated each year – 22 million within the national legal system and 20 million outside it. In the latter case, the abortions are often performed by unskilled providers or in unhygienic conditions, or both.
Only one in three legal (and mostly safe) abortions take place in developing countries (excluding China), while 98% of unsafe abortions occur there. Over five million or approximately 1 in 4 women having an unsafe abortion is likely to face severe complications, which can cause death, and will seek hospital care, putting heavy demand on scarce resources. Unsafe abortion nonetheless remains a neglected health care problem in developing countries. Unsafe abortion is characterized by the inadequacy of the provider’s skills and use of hazardous techniques and unsanitary facilities. Women who resort to clandestine facilities or unqualified providers put their health and life at risk.
The World Health Organization (WHO) is concerned with the public health aspects of unsafe abortion. As early as 1967, the World Health Assembly passed Resolution WHA20.41, which stated that “abortions ... constitute a serious public health problem in many countries”, and requested the Director-General to “continue to develop the activities of the World Health Organization in the field of health aspects of human reproduction”. WHO defines unsafe abortion as a procedure for terminating an unintended pregnancy carried out either by persons lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both.
The consensus statement of the 1994 International Conference on Population and Development (ICPD) noted that “All Governments and relevant intergovernmental and non-governmental organizations are urged to strengthen their commitment to women’s health, to deal with the health aspect of unsafe abortion as a major public health concern and to reduce the recourse to abortion through expanded and improved family-planning services.”
The above was reiterated in 1999 at the five-year review of the implementation of the ICPD Programme of Action by the UN General Assembly in New York, USA. The Assembly further agreed that, “in circumstances where abortion is not against the law, health systems should train and equip health-service providers and should take other measures to ensure that such abortion is safe and accessible.” In spite of these calls for action, and a rise in contraceptive use globally, unsafe abortion continues to be common, especially in developing countries.- Introduction p.1
- The incidence of unsafe abortion is influenced by the legal provisions governing access to safe abortion, as well as the availability and quality of legal abortion services. Restrictive legislation is associated with a high incidence of unsafe abortion.
- 2. Legal framework of abortion, p.2
- Abortion laws are diverse and can be complex. There may be discrepancies between the wording of the law (de jure) and its application (de facto), which means that common practice can help or hinder the procurement of legal abortion. Even where it is legally permitted, safe abortion may not be easily accessible; there may be additional requirements regarding consent and counselling, and countries often impose a limit on the period during which abortion may be performed. In addition, the attitudes of medical staff may be discouraging, and abortion services may be insufficient to meet the demand, unevenly distributed or of poor quality. Finally, women themselves may be unaware of the availability of abortion services or their right to access them within the legal framework.
- 2. Legal framework of abortion, p.2
- It has been estimated that almost 40% of pregnancies worldwide are unplanned – the result of non-use of contraception, ineffective contraceptive use or method failure. Unintended pregnancy, and induced abortion, can be prevented and reduced by expanding and improving family planning services and choices, reaching out to communities and underserved population groups, for example sexually active teenagers and unmarried women.
- 3. Fertility transition and unplanned pregnancy, p.2
- When people are motivated to regulate their fertility, but effective contraception is largely inaccessible or not consistently or correctly used, a large number of unplanned pregnancies occur. Many married women in developing countries do not have access to the contraceptive methods of their choice. The situation is even more difficult for unmarried women, particularly adolescents, who rarely have access to information and counselling on sexual and reproductive health, and are frequently excluded from contraceptive services. An estimated 123 million women have an unmet need for family planning. During rapid transition from high to low fertility, as has been witnessed in several countries, contraceptive services are often unable to meet the growing demand of couples for fertility regulation, resulting in an increased number of unplanned pregnancies, some of which are terminated by induced abortion. Also, where less effective family planning methods are commonly used, unplanned pregnancies and, consequently, abortions are likely to occur. Of course, no contraceptive method is 100% effective. It is estimated that each year 27 million unintended pregnancies occur as a result of method failure or ineffective use; of these, about 6 million occur even though the contraceptive method has been used correctly and consistently.
- pp.2-3
- Application of statistical models shows that an increase in contraceptive prevalence and in use of effective contraceptive methods will reduce the incidence of abortion. The validity of this model was recently demonstrated using data from developed countries. The latter study also showed that, when fertility starts to decline, both abortion and contraceptive use can rise simultaneously. The authors’ explanation for this is that contraceptive use alone is unable to meet the growing demand for fertility regulation. As early as 1962, these trends were observed in Santiago, Chile. Current estimates of unsafe abortion and contraceptive use by fertility level in developing countries show similar trends. An aggregated analysis of the association between use of contraception and unsafe abortion by region indicates that women may resort to unsafe abortion to space births before terminating childbearing through sterilization. (Sterilization is the most common modern contraceptive method in some parts of the world, such as Latin America and South-central Asia.) It is therefore essential, not only to make family planning available, but also to offer an appropriate choice of contraceptive methods to meet the individual needs to space or limit births.
- p.3
- Each year, an estimated 80 million women have an unplanned pregnancy. Some of these women will decide to continue the pregnancy, while others will consider having an abortion. A number of women who attempt to have an abortion will not be successful, and will carry the unwanted pregnancy to term. The number of women who attempt an unsafe abortion, risking their life and health, is 20–25% higher than the number who succeed. In addition, some women may make repeated attempts to terminate a pregnancy before succeeding, each time risking their health.
- 4. Abortion attempts, p.4
- A recent survey of 2400 women in Madhya Pradesh, India, found that 32% of women aged 35–39 years had attempted abortion at some time, and 23% had had an abortion, indicating that roughly one in four women who attempted abortion did not succeed. Self-reported morbidity was higher in rural areas (57%) than in urban areas (45%). Severe complications were also more common in rural areas (35% vs. 16%), showing that higher risks are associated with abortions in underserved rural areas. Not unexpectedly, only 9% of the women knew that abortion was legal, 49% thought that abortion was illegal, and 36% did not know its legal status; the remaining 6% reported knowing that abortion was legal, but their knowledge of the period within which it was legal was incorrect.
In Pakistan, of 1214 women interviewed, 100 (8.2%) reported seeking an abortion to terminate an unplanned pregnancy at least once; 89 of these women were successful. In Teheran, Islamic Republic of Iran, 38% of 6394 pregnant women reported that the pregnancy was unwanted; 12% of these (297) resorted to abortion. Some women make several unsafe attempts to end an unintended pregnancy, even where medical services are available. For example, although menstrual regulation (MR) is available in Bangladesh, a comprehensive study in 1996–97 showed that only 40% of 143 women seeking abortion-related care had turned first to health facilities; others had seen two or three untrained providers. Four of the women had to be referred to the district hospital with serious complications, and one died. The untrained practitioners included traditional birth attendants, homoeopaths, herbalists, religious healers, village doctors and relatives.
Many abortions are self-induced: in Cambodia, where abortion is legally available on request, women often attempt to abort themselves before turning to hospital. In a study in health facilities in Nigeria, it was found that 30% of women seeking abortion care had first attempted to stop the pregnancy themselves, or had turned to an untrained person. A recent survey of over 3000 women aged 15–49 years in eight states in Nigeria found that 28% had had at least one unwanted pregnancy; 58% of these had tried to terminate a pregnancy, and 84% of women who attempted had succeeded. In another study of 1516 women aged 15–44 years in Jos and Ife (Nigeria), 20% reported having had an unwanted pregnancy; 58% of them stated that they had terminated the pregnancy, whereas 9% had failed; the remaining women had not taken any action. In a survey of 999 women in Bamako, Mali, 122 of 144 women who reported having attempted an abortion had succeeded. In rural villages in Mali, 28% of women surveyed reported having had an undesired pregnancy; 19% had attempted an abortion, but fewer than half of them were successful.
Where almost all abortions are legal, overall success rates reflect this, e.g. the 1998 Reproductive Health Survey in Mongolia reported that, among the 64% of women who had attempted to stop an unplanned pregnancy, only 2–3% had failed.- 4. Abortion attempts, p.4
- When induced abortion is performed by qualified persons using correct techniques and in sanitary conditions, it is a safe surgical procedure. In the USA, for example, the death rate from induced abortion is now 0.6 per 100 000 procedures, making it as safe as an injection of penicillin. In developing countries, however, the risk of death following unsafe abortion may be several hundred times higher. Spontaneous abortion is rarely fatal and seldom presents complications. The mortality and morbidity risks associated with unsafe induced abortion depend on the facilities and the skill of the abortion provider, the method used, the general health of the woman and the stage of her pregnancy. Unsafe abortion may be induced by the woman herself, by a non-medical person or by a health worker under unhygienic conditions. Abortion attempts may involve insertion of a solid object (root, twig or catheter) into the uterus; a dilatation and curettage procedure performed improperly by an unskilled provider; ingestion of harmful substances; exertion of external force; or misuse of modern pharmaceuticals. In many settings, traditional practitioners vigorously pummel the woman’s lower abdomen to disrupt the pregnancy; this can cause the uterus to burst, killing the woman.
- 5. Health consequences of unsafe abortion and impact on health services, p.5
- The outcome of complications of unsafe abortion depends not only on the availability and quality of post-abortion care, but also on women’s willingness to turn to medical services, and the readiness of medical staff to deal promptly with the complications. The cases of incomplete abortion, post-abortion sepsis, haemorrhage and genital trauma that reach hospital, and the abortion deaths, are the visible consequences of restrictive legal codes. For every identified hospital case, there are many other women who have had an unsafe abortion, but who do not seek medical care, either because they do not have sufficiently worrying complications or because they fear abuse, ill-treatment or legal reprisals.
One recent study estimated that every year in developing countries five million women are admitted to hospital as a result of unsafe abortion. The treatment of abortion complications in hospital consumes a significant share of resources, including hospital beds, blood supply, medications, and often operating theatres, anaesthesia and medical specialists. Thus, the consequences of unsafe abortion place great demands on the scarce clinical, material and financial resources of hospitals in many developing countries, undoubtedly compromising other maternity and emergency services. Major physiological, financial and emotional costs are also incurred by the women who undergo unsafe abortion.
A review of the combined impact of mortality and morbidity due to unsafe abortion estimated that, every year, there are 65 000 to 70 000 deaths and close to five million women with temporary or permanent disability due to unsafe abortion. Of these, more than 3 million suffer from the effects of reproductive tract infection (RTI), and almost 1.7 million will develop secondary infertility. Unsafe abortion accounts for 13% of maternal deaths, and 20 % of the total mortality and disability burden due to pregnancy and childbirth, in terms of disability-adjusted life years (DALYs). Altogether some 24 million women currently suffer secondary infertility caused by an unsafe abortion.
In DALYs, the combined burden of mortality and morbidity per 1000 unsafe abortions is exceptionally high in sub-Saharan Africa, where it is 50 percentage points higher than in Asia and 6 times greater than in Latin America.- p.5
- The age pattern of unsafe abortion is critical to a better understanding of the barriers to access and to tailoring interventions by age group. A recent review found that two-thirds of unsafe abortions occur among women aged between 15 and 30 years. More importantly from a public health perspective, 2.5 million, or almost 14%, of all unsafe abortions in developing countries are among women under 20 years of age. Figure 2 illustrates the age pattern of unsafe abortions, which differs markedly from region to region. The proportion of women aged 15–19 years in Africa who have had an unsafe abortion is higher than in any other region; almost 60% of unsafe abortions in Africa are among women aged less than 25 years and almost 80% are among women below 30. This contrasts with Asia, where 30% of unsafe abortions are in women under 25 and 60% are in women under 30. In Latin America and the Caribbean, women aged 20–29 years account for more than half of all unsafe abortions, with almost 70% of unsafe abortions being carried out on women below 30, demonstrating an age pattern between those for Africa and Asia. Interventions need to be tailored according to the specific regional age pattern of unsafe abortion, though prevention of unsafe abortion at all ages should remain a high priority.
- pp.5-6
- Abortion is not a marginal practice in the Congo. However, measuring it is difficult, because of a number of circumstances surrounding it. Censured by practically all religions and subject to particularly restrictive legislation, abortion is usually carried out clandestinely and, as a result, is not amenable to full registration.” This quotation, translated from the 2005 Demographic and Health Survey (DHS) of Congo,summarizes the abortion situation in much of the developing world, and points to the key problems related to estimating its extent.
- 6. Estimating unsafe abortion, p.6
- Where induced abortion is restricted and largely inaccessible, or legal but difficult to obtain, little information is available on abortion practice. In such circumstances, it is difficult to quantify and classify abortion. What information is available is inevitably not completely reliable, because of legal, ethical and moral considerations that hinder reporting. Occurrence tends to be under-reported in surveys, and unreported or under-reported in hospital records. Of course, there are no records on women who do not seek post-abortion care in hospitals. Only the “tip of the iceberg” is, therefore, visible in the number of deaths and the number of women who suffer severe trauma, or who have an infection or severe blood loss and seek medical care.
Whether legal or illegal, induced abortion is generally stigmatized and frequently censured by religious teaching or ideologies. Women are often reluctant to admit to an induced abortion, especially when it is illegal, and under-reporting occurs even where abortion is legal. When abortions are clandestine, they may not be reported at all or may be reported as spontaneous abortion (miscarriage). The language used to describe induced abortion reflects this ambivalence: terms include “induced miscarriage” (fausse couche provoquée), “menstrual regulation”, and “regulation of a delayed or suspended menstruation”. For example, in one study 16.6% of women admitted to an abortion; however, only 4.4% said they had terminated a pregnancy, and 12.2% reported that they had “induced menstruation”. It is therefore not surprising that unsafe abortion is one of the most difficult indicators to measure.- pp.6-7
- Where induced abortion is restricted or illegal, its occurrence can be estimated only indirectly, using the available incomplete information on incidence and mortality.
- p.7
- Abortion-related mortality occurs mainly as a result of unsafe abortion, since spontaneous abortion only rarely causes death. Commencing with abortion deaths as a percentage of all maternal deaths, unsafe abortion-related mortality is related to the estimated number of maternal deaths, to calculate the numbers of unsafe abortion deaths.
- p.7
- Induced abortions may be performed either within the law, or outside the national legal framework. The medical standards of abortion procedures vary, whether performed within or outside the law.
When performed within the legal framework, the safety of the procedure will depend on the requirements of the law, and the resources and medical skills available. In some countries, lack of resources and possibly skills may mean that even abortions that meet the legal and medical requirements of the country would not necessarily be considered sufficiently safe in high-resource settings.
Induced abortions outside the legal framework are frequently performed by unqualified and unskilled providers, or are self-induced; such abortions often take place in unhygienic conditions, and involve the use of dangerous methods or incorrect administration of medications. Even when performed by a medical practitioner, an abortion that is carried out in secret, outside a recognized facility, generally carries an additional risk: medical back-up is not immediately available in an emergency, the woman may not receive appropriate post-abortion attention and care, and if complications occur, the woman may hesitate to seek care. The relative safety of unsafe abortion differs by country depending on the skills of the providers and the methods used, but is also linked to the de facto application of the law.
The estimates given in this document are intended to reflect induced abortions that carry greater risks than those carried out officially for reasons accepted in the laws of a country.- 6.1 Operational definition of unsafe abortion, p.7
- Unsafe abortion rate: The unsafe abortion rate is the annual number of unsafe abortions per 1000 women aged 15–44 years. This measure describes the level of unsafe abortion in a population. Unsafe abortion ratio: The unsafe abortion ratio is the number of unsafe abortions per 100 live births (as a proxy for pregnancies). The unsafe abortion ratio indicates the likelihood that a pregnancy will end in unsafe abortion rather than a live birth. Unsafe abortion mortality ratio: The unsafe abortion mortality ratio is the number of deaths due to unsafe abortion per 100 000 live births. This is a subset of the maternal mortality ratio and measures the risk of a woman dying due to unsafe abortion relative to the number of live births. Unsafe abortion case-fatality: The unsafe abortion case-fatality expresses the estimated number of deaths per 100 000 unsafe abortion procedures; it is sometimes expressed per 100 procedures. This rate shows the mortality risk associated with unsafe abortion. Percentage of maternal deaths due to unsafe abortion: The percentage of maternal deaths due to unsafe abortion is the number of abortion deaths per 100 maternal deaths. When maternal mortality is relatively low and where other causes of maternal death have already been substantially reduced, a small number of unsafe abortion deaths may account for a significant percentage of maternal deaths. This measure is, therefore, not particularly suitable for comparison purposes.
- 6.2 Unsafe abortion incidence and mortality rates and ratios, p.8
- Unsafe abortion is negligible in eastern Asia and in some developing countries of other regions where abortion is legal and relatively accessible, in particular Cuba, Singapore, Tunisia, Turkey and Viet Nam.
- 6.3 Selecting the denominator for rates and ratios: all countries vs countries with evidence of unsafe abortion, p.8
- Aggregated estimates are quite robust; nevertheless, estimates of the incidence of unsafe abortion and the resulting mortality necessarily have some degree of uncertainty. They should be considered only as best estimates given the information currently available. It is likely that the true incidence of unsafe abortion and the related mortality rate are higher than estimated.
- 6.4 Estimating subregional, regional and global incidence of unsafe abortion and associated mortality p.9
- Worldwide, the estimates indicate that almost 20 million unsafe abortions were carried out in 2003, i.e. one in ten pregnancies ended in an unsafe abortion, giving a ratio of one unsafe abortion to about seven live births. For the period around 2000, 19 million unsafe abortions per year were estimated.
Globally, 19–20 million unsafe abortions are estimated to have occurred each year from 1993 to 2003, as the transition to low fertility has advanced; contraceptive prevalence has increased, but so has unmet need for family planning as smaller families become the norm. However, caution is needed when comparing estimates of unsafe abortion for different periods, in view of the limitations of the estimates and the increasing knowledge base, which may mean that earlier estimates were too low.- 7.1 Global and regional estimates and research; p.14
- The current figures for Africa are higher than the previous cautious estimates, better reflecting the actual situation. It is nevertheless encouraging to note that the 1996 change of law in South Africa is now having a positive effect in reducing the number of unsafe abortions in the subregion. Unsafe abortion numbers are also lower in South-central Asia, and Asia as a whole, as the most recent assessment of abortion in India shows fewer procedures that do not meet national requirements. Recent research and improved access to data for South America have led to estimates indicating that the number of unsafe abortions in the region may have stabilized.
There is still room for further research, as well as assessments of abortion incidence and mortality, in the regions mentioned. At the same time, major information gaps exist for other parts of the world. For example in Oceania, abortion numbers reported are usually well within what would be expected for women hospitalized for miscarriage, while the abortion debate goes on and the local press covers the legal proceedings of prosecutions for illegal abortion. Information is scant and estimates remain guarded for several countries of Northern Africa and Western Asia. Reports suggest that unsafe abortions may be increasing in several of the newly independent states (formerly part of the Soviet Union), as a result of increased fees and fewer services for legal abortions, but there are, as yet, insufficient data or research to confirm this.- 7. Regional and global incidence of unsafe abortion and associated mortality, p.14
- The global figures show the full effect of the smaller denominator: the 19.7 million unsafe abortions correspond to 22 or 14 per 1000 women aged 15–44, and to 20 or 15 per 100 live births. For developing countries, the incidence rate increases from 16 to 24 per 1000 women of reproductive age, when the denominator is restricted. The few developing countries with liberal abortion laws and no evidence of unsafe abortion all fall in the group of “other developing countries”, leading to a marked difference in the incidence rate and ratio. The group of least developed countries shows a high unsafe abortion rate of 25 per 1000 women of reproductive age.
- 7.2 Rate and ratio calculations including only countries with evidence of unsafe abortion, p.15
- Over 60% of the world population lives in countries where induced abortion is allowed for a wide range of reasons; nevertheless, some of these countries have a high incidence of unsafe abortion. The estimates show that only about 40% of women of reproductive age live in countries where abortion is legally available on request and there is no evidence of unsafe abortion (Annex 1); 1 in 4 births take place in these countries. On the other hand, there are a number of countries, mainly in the Eastern Europe region, that allow abortion on broad grounds, but where unsafe abortions still occur outside the legal framework, because of the cost of legal abortion and other social factors.
Unsafe abortion rates close to 30 per 1000 women of reproductive age are seen in both Africa and Latin America; however, because of the higher relative number of births, the unsafe abortion ratio for Africa is only half that for Latin America. However, the range of estimates for Africa is wide: Eastern Africa has the highest incidence rate of any subregion, at 39 per 1000 women aged 15–44, while Southern Africa has among the lowest, at 18 per 1000 (not counting legal abortions of 5 per 1000 women). In Eastern, Western and Middle Africa, where maternal mortality is high, the unsafe-abortion-related mortality ratio is much higher than anywhere else – double that of Asia and more than 5 times that of Latin America. Morbidity is an even more frequent consequence of unsafe abortion, and it is thus not surprising that the total disease burden for Africa is exceptionally high, threatening women’s lives and health, and straining scarce resources.
Middle, Western and Eastern Africa all have a contraceptive prevalence below 25%, with heavy reliance on traditional methods. In Southern and Northern Africa, contraceptive prevalence among married women is around 50%, and there is greater reliance on reversible modern methods (36% and 43%, respectively). This could help explain the moderate abortion rates of around 20 per 1000 women, as compared to 26 to 39 per 1000 in other parts of Africa.- 7.3 Regional estimates, p.15
- The incidence of unsafe abortion for Latin America overall appears to have stabilized, and may have passed its peak. If Cuba is excluded from the calculation, the incidence rate for the Caribbean falls between those for Central America (25 per 1000) and South America (33 per 1000). The prevalence of modern contraceptives ranges from 57% to 66% in Latin America; however, 43–50% is accounted for by sterilization (Fig. 1). The moderate 29–38% prevalence of reversible method use could mean that unsafe abortion is being used to space births, to arrive at a total fertility rate of around 2.5 per woman.23 Improved access to a range of birth-spacing methods could reduce the number of unintended pregnancies and hence the need for abortion. Almost 2000 deaths from unsafe abortion occur, approximately 20 per 100 000 births; this is the lowest among the developing regions, and is attributable to the relatively well functioning health services in Latin America.
- pp.15-16
- South-central Asia has the highest number of unsafe abortions of any subregion, owing to the sheer size of its population; in 2003, there were 6.3 million unsafe abortions, or 18 per 1000 women of reproductive age, which poses a formidable challenge. Use of modern contraceptive methods among married women is modest (42%), and two-thirds of this use relates to sterilization; the high number of unsafe abortions is probably the result of a desire to space births. Nevertheless, among Asia’s subregions, South-eastern Asia has the highest incidence rate, at 27 per 1000 women aged 15–44 (excluding countries with no evidence of unsafe abortion); this rate is similar to those of the Caribbean and Central America. South-eastern Asia has a 51% prevalence of modern family planning methods, almost exclusively reversible methods (43%). It appears, though, that abortion is required to keep fertility low. The unsafe-abortion-related mortality for Asia is 2–3 times that for Latin America, but less than half that for Africa, reflecting the relative standards of health services and infrastructure. While it is acknowledged that there is a problem of unsafe abortion in Oceania, data are exceptionally scant and, as a consequence, estimates vary.
- pp.15-16
- The new research evidence from Africa shows higher rates of unsafe abortion in 2003 than in 2000. However, the apparent increase may be related to the better coverage as a result of new studies. In any case, the 2003 estimates more accurately reflect the situation in Africa.
Estimates for South-central Asia reflect improvements in service provision that have taken place over a number of years. Rates for South-eastern Asia have changed little, while the trend in Western Asia is unclear, since the data available are insufficient and of uncertain quality.
For Latin America, an increased availability of data has improved the precision of the estimates. Unsafe abortion rates in South America appear to be stabilizing, while in the Caribbean there may well have been an increase. This is possibly related to the rapid transition to low fertility in the Caribbean region, which now has the lowest TFR of all the developing subregions. The TFR for Central America fell by 0.8 over the past 10 years and by 0.3 over the past 5 years – the largest decrease in the Latin America region. This suggests that the rise in the unsafe abortion rate may be temporary.- 7.4 Trends in unsafe abortion rates, p.16
- There has been a small reduction in the number of deaths in 2003 due to unsafe abortion compared with the estimate for 2000. This is in line with the assumption that maternal deaths in general may be slowly declining globally, probably as a result of improved maternity services and better care. Overall, 66 500 maternal deaths were estimated to have been due to unsafe abortion in 2003. Nearly all of these deaths could have been prevented if the need for family planning had been met, and if abortion services had been legally available and affordable everywhere.
Globally, the proportion of maternal deaths due to unsafe abortion has remained close to 13% over time, although there have been regional variations. The percentage of maternal deaths due to unsafe abortion is relatively difficult to interpret. In countries where maternal mortality is relatively low and other causes of maternal death have already been substantially reduced, a small number of deaths due to unsafe abortion may account for a significant percentage of maternal deaths. This is, for example, the case in some countries of Latin America. On the other hand, in the least developed countries, 10% of all maternal deaths are due to unsafe abortion, but the ratio of maternal deaths to live births is high, at 90 per 100 000, while in other developing countries, 15% of maternal deaths are due to unsafe abortion but the ratio of maternal deaths to live births is 50 to 100 000 births – just over half that in the least developed countries. Clearly, when maternal mortality from all causes is high, the percentage of these deaths caused by unsafe abortion is relatively low. Therefore, the ratio of unsafe abortion deaths per 100 000 live births is a better measure of the relative risk of maternal death due to unsafe abortion.- 7.5 Unsafe abortion mortality, p.17
- In Eastern, Middle and Western Africa, 100 or more maternal deaths per 100 000 live births are due to unsafe abortion. In no other subregion does unsafe abortion lead to so many maternal deaths. Within Africa, Northern and Southern Africa have ratios as low as those found in Latin American subregions, which are among the lowest in the developing countries.
- 7.5 Unsafe abortion mortality, p.17
- The estimated case-fatality rate (deaths per 100 000 unsafe abortion procedures) ranges from a high of 750 per 100 000 in sub-Saharan Africa to 10 per 100 000 in developed regions, with an average of 350 per 100 000 for developing regions. Table 3 also shows that the global case-fatality rate associated with unsafe abortion is some 550 times higher than the rate associated with legal induced abortions in the USA (0.6 per 100 000 procedures); in sub-Saharan Africa, the rate is well over 1000 times higher. Even in developed countries, the case-fatality rate for unsafe abortion is 20 times higher than that for legal induced abortion.
- 7.6 Risk of death due to unsafe abortion, p.18
- The differences in the risk of death associated with unsafe abortion across subregions of the developing world can be seen in Figure 7. The risks associated with unsafe abortion reflect the procedures used, and the availability, access and quality of services for management of complications. At the high end of the spectrum are the African subregions, where high-risk abortion methods, failing infrastructure, and poor public health facilities result in case-fatality rates of over 800 per 100 000 procedures. At the opposite end, South and Central America have case-fatality rates of less than 100 per 100 000 procedures. For Southern and Northern Africa and South-eastern Asia, the rates appear low but are still almost 200 times higher than that associated with a legal abortion in the USA.
The risk of death due to unsafe abortion is highest in three subregions of sub-Saharan Africa– Middle, Western and Eastern Africa – at 800–900 deaths per 100 000 unsafe abortions, followed by South-central Asia. Latin America and the Caribbean, on the other hand, is the developing region with the lowest case-fatality rate.- 7.6 Risk of death due to unsafe abortion, p.18
- To explore the pattern of maternal deaths due to unsafe abortion by age, we applied the regional age distributions of the incidence of unsafe abortion to the estimated unsafe abortion deaths. This assumes that each age group has the same risk of death due to unsafe abortion. Any difference in risk in the different age groups is difficult to quantify because of a lack of data. It can, however, be assumed that women in the youngest age group are likely to have a higher risk of morbidity and mortality from unsafe abortion, as they are biologically more vulnerable and likely to have fewer resources to acquire a less risky unsafe abortion.
Table 4 shows the estimated number of deaths from unsafe abortion by age group for the developing regions. Almost half of the deaths occur among adolescents and adults under 25 years. The percentage distributions of unsafe abortions and of unsafe abortion deaths by age are shown in Figure 8. For developing regions the estimated case-fatality rate in the youngest age group is 440 per 100 000 procedures, declining by increasing age to 280 in the age group 40 and over.- 7.7 Maternal death by age, p.18
- Research and collection of data on unsafe abortion need to be strengthened to cover the range of relevant critical issues. Better information will support a more informed scientific discourse, and help set in motion the processes to put unsafe abortion on the political agenda. Needed research should cover, but not be limited to, the incidence of unsafe abortion and associated mortality, post-abortion complications, sociodemographic characteristics of women who have abortion, gestation and parity at abortion, decision-makers and decision-making processes relating to having an abortion, place and circumstances of abortion, abortion providers, unmet need for family planning, and method mix of family planning.
Major progress has been made in some areas of sexual and reproductive health, most notably in contraceptive use. However, unsafe abortions, though entirely preventable, continue to occur in almost all developing countries. The major public health implications include, but are not limited to, maternal morbidity and mortality. In addition, there are financial costs to women and to health services for treating complications.
Governments need to assess the health impact of unsafe abortion, reduce the recourse to abortion by expanding and improving family planning services, and design abortion policies and interventions to improve women’s health and well-being. Preventing unintended pregnancies and unsafe abortion must continue to be a high priority for improving women’s sexual and reproductive health. Information and services for family planning and abortion care should be readily available, including to young people.
In several countries, the legalization of abortion has not been followed by elimination of unsafe abortion. This may be because women are unaware that safe abortion services are available, or lack the resources, time or decision-making power to use the services, or because the services are inadequate to meet demand. Other factors inhibiting use of safe abortion where it is legal are lack of privacy and confidentiality, poor access, and discouraging attitudes of health care providers.
Women who wish to terminate their pregnancy should have ready access to reliable information, compassionate counselling and, in parallel, services for the prevention of subsequent unintended pregnancy and management of complications. It is vital that governments and intergovernmental and nongovernmental organizations deal openly with unsafe abortion as a major public health concern.- 8. Conclusions, pp.20-21
“Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008” (2011)
[edit]World Health Organisation (2011). “Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008”, (PDF). (6th ed.). World Health Organisation. ISBN 978-92-4-150111-8. Archived (PDF) from the original on 28 March 2014.
- Deaths due to unsafe abortion remain close to 13% of all maternal deaths. Unsafe abortion-related deaths have, however, reduced to 47 000 in 2008 from 56 000 in 2003 and 69 000 in 1990; corresponding to the decline in the overall number of maternal deaths to 358 000 in 2008 from 546 000 in 1990. Although unsafe abortions are preventable, they continue to pose undue risks to women’s health and lives.
- p.1
- Each year, throughout the world, approximately 210 million women become pregnant and over 135 million of them deliver liveborn infants. The remaining 75 million pregnancies end in stillbirth, or spontaneous or induced abortion. It was estimated that in 2003 approximately 42 million pregnancies were voluntarily terminated: 22 million safely and 20 million unsafely. Unsafe abortions are frequently performed by providers lacking qualifications and skills to perform induced abortion, and some abortions are self-induced. Unsafe induced abortions do not meet officially prescribed circumstances and safeguards; they are aggravated by unhygienic conditions, dangerous interventions or incorrect administration of medication. Although unsafe abortions are preventable, they continue to pose undue risks to a woman’s health and may endanger her life.
- p.2
- Close to 20% of women aged 15–44 years live in countries where abortion is not legally permitted at all or restricted to saving the woman’s life, and 57% live in countries where induced abortion has fewer legal restrictions and women could request an abortion for a variety of reasons; nevertheless, unsafe abortions take place along the whole legal spectrum. Only 36% of women of reproductive age live in countries where there is no evidence of unsafe abortion, while 39% of women aged 15–44 years live in countries where abortion is available on request. These two groups of countries largely coincide, however, there are countries that do not allow abortion on request (for example, in the United Kingdom abortion is not permitted on the grounds of rape or incest, and in New Zealand not for socioeconomic reasons). India where abortion was legalized in 1971 presents the opposite situation: abortion is available on all grounds (although not on request), nevertheless, unsafe abortions take place. In a number of countries in eastern Europe and countries of the former Soviet Union that allow abortion on broad grounds or on request, some unsafe abortions occur outside the legal framework because of poor access to safe abortion services, for example in rural areas of the countries. In most countries where the law is less restrictive but services are unevenly distributed, for example in rural areas, unsafe abortions still take place. Other countries such as Cambodia, Guyana, Nepal, South Africa and, most recently, Ethiopia are in the process of implementing less-restrictive abortion laws with varying success and therefore show unsafe abortions in parallel with safe and legal services.
- pp.4-5
- Worldwide, unsafe abortions are estimated to be between 21 million and 22 million in 2008, almost 2 million more than the number estimated for 2003. There were approximately 210 million pregnancies in 2008; therefore around one in 10 pregnancies ends in an unsafe abortion worldwide. Nevertheless, the global rate at 14 per 1000 women aged 15–44 years remains unchanged since 2003; the increase in numbers of unsafe abortion therefore is mainly an effect of the increasing numbers of women of reproductive age in the world.
- p.8
- Reviewing 20 years of estimates for unsafe abortion incidence, rates and ratios show that unsafe abortion continues playing an important role in developing country regions. The numbers, rate and ratio show that women all over the world are likely to resort to an unsafe abortion when faced with an unwanted pregnancy and provisions for safe abortions are unavailable or inaccessible; and that in subregions with low fertility the ratio is relatively high.
- p.26
- Globally, the proportion of maternal deaths due to unsafe abortion has remained close to 13% over time. Contrary to the global percentage of maternal deaths due to unsafe abortion, the averages by subregions and regions are distinct and, furthermore, the percentage varies extensively between countries within each subregion, reflecting country specific circumstances of unsafe abortion incidence and access to care. Even as such variation is absorbed in averages, the aggregated regional and global numbers are more robust.
- p.27
- The global case–fatality rate (220 per 100 000) associated with unsafe abortion is some 350 times higher than the rate associated with legal induced abortions in the USA (0.6 per 100 000 procedures); in sub-Saharan Africa, the rate is more than 800 times higher. Even in developed countries, the case–fatality rate for unsafe abortion is 40 times higher than that for legal induced abortion.
- p.30
- Unsafe abortion and deaths due to complications of unsafe abortion continue to afflict the lives of many women, mostly in developing countries. Unsafe abortion is the cause of serious complications and disability for millions of women each year and is a prominent cause of maternal death. Despite efforts to achieve Millennium Development Goal 5 Target 5A – reduce by three quarters the maternal mortality ratio between 1990 and 2015 – the percentage of maternal deaths due to unsafe abortion remains unchanged at 13%. Numbers of unsafe abortions have risen with the increase in the number of women of reproductive age. This trend may continue unless women’s access to safe abortion and contraception – and support to empower women (including their freedom to decide whether and when to have a child) – are put in place and further strengthened.
Unsafe abortions, though entirely preventable, continue to occur in almost all developing countries and in Eastern Europe. The evidence suggests that a reliance on abortion can be greatly reduced when:
* women can plan pregnancies through effective contraception;
* counselling and services meet the unmet need for family planning, and appropriate method mix of contraception is offered to all women, including both married and unmarried women; and
* safe abortion services are available and accessible.- p.31
"Facts on Induced Abortion Worldwide" (January 2012)
[edit]"Facts on Induced Abortion Worldwide" (PDF). World Health Organization. January 2012. Archived (PDF) from the original on 9 March 2021. Retrieved 9 May 2021.
- Between 1995 and 2008, the rate of unsafe abortion worldwide remained essentially unchanged, at 14 abortions per 1,000 women aged 15-44.
- p.2
- In 2008, more than 97% of abortions in Africa were unsafe. Southern Africa is the subregion with the lowest proportion of unsafe abortions (58%). Close to 90% of women in the subregion live in South Africa, where abortion was liberalized in 1997.
- p.2
- In Latin America, 95% of abortions were unsafe, a proportion that did not change between 1995 and 2008. Nearly all safe abortions occurred in the Caribbean, primarily in Cuba and several other islands where the law is liberal and safe abortions are accessible.
- p.2
- In Asia, the proportion of abortion that are unsafe varies widely by subregion, from virtually none in eastern Asia to 65% in South Central Asia.
- p.2
- The estimated annual number of deaths from unsafe abortion declined from 56,000 in 2003 to 47,000 in 2008. Complications from unsafe abortion accounted for an estimated 13% of all maternal deaths worldwide in both years.
- p.2
- In the United States, legal induced abortion results in only 0.6 deaths per 100,000 procedures. Worldwide, unsafe abortion accounts for a death rate that is 350 times higher (220 per 100,000), and, in Sub-Saharan Africa, the rate is 800 times higher, at 460 per 100,000.
- p.2
- Unsafe abortion is a significant cause of ill-health among women in the developing world. Estimates for 2005 indicate that 8.5 million women annually experience complications from unsafe abortion that require medical attention, and three million do not receive the care they need.
- p.3
- Treating medical complications from unsafe abortion places a significant financial burden on public health care systems in the developing world. According to a 2009 study, the minimum annual estimated cost of providing postabortion care in the developing world is $431 million.
- p.3
"Worldwide, an estimated 25 million unsafe abortions occur each year" (28 September 2017)
[edit]"Worldwide, an estimated 25 million unsafe abortions occur each year". World Health Organization. 28 September 2017. Archived from the original on 29 September 2017. Retrieved 29 September 2017.
- “Increased efforts are needed, especially in developing regions, to ensure access to contraception and safe abortion,” says Dr Bela Ganatra, lead author of the study and a scientist in the WHO Department of Reproductive Health and Research.
“When women and girls cannot access effective contraception and safe abortion services, there are serious consequences for their own health and that of their families. This should not happen. But despite recent advances in technology and evidence, too many unsafe abortions still occur, and too many women continue to suffer and die.” - In countries where abortion is completely banned or permitted only to save the woman’s life or preserve her physical health, only 1 in 4 abortions were safe; whereas, in countries where abortion is legal on broader grounds, nearly 9 in 10 abortions were done safely. Restricting access to abortions does not reduce the number of abortions.
- Among developing regions, the proportion of abortions that were safe in Eastern Asia (including China) was similar to developed regions. In South-Central Asia, however, less than 1 in 2 abortions were safe. Outside of Southern Africa, less than 1 in 4 abortions in Africa were safe. Of those unsafe abortions, the majority were characterized as “least safe.”
In Latin America, only 1 in 4 abortions were safe, though the majority were categorized as “less safe,” as it is increasingly common for women in the region to obtain and self-administer medicines like misoprostol outside of formal health systems. This has meant that this region has seen fewer deaths and fewer severe complications from unsafe abortions. Nevertheless, this type of informal self-use of medication abortion that women have to resort to secretly does not meet WHO’s safe abortion standards.
"Abortion". www.who.int. Retrieved 19 April 2019.
[edit]- Abortion is a common health intervention. It is safe when carried out using a method recommended by WHO, appropriate to the pregnancy duration and by someone with the necessary skills.
- Around 45% of all abortions are unsafe, of which 97% take place in developing countries.
- Unsafe abortion is a leading – but preventable – cause of maternal deaths and morbidities. It can lead to physical and mental health complications and social and financial burdens for women, communities and health systems.
- Lack of access to safe, timely, affordable and respectful abortion care is a critical public health and human rights issue.
- When carried out using a method recommended by WHO appropriate to the pregnancy duration, and by someone with the necessary skills, abortion is a safe health care intervention.
However, when people with unintended pregnancies face barriers to attaining safe, timely, affordable, geographically reachable, respectful and non-discriminatory abortion, they often resort to unsafe abortion.
Global estimates from 2010–2014 demonstrate that 45% of all induced abortions are unsafe. Of all unsafe abortions, one third were performed under the least safe conditions, i.e., by untrained persons using dangerous and invasive methods.
Developing countries bear the burden of 97% of all unsafe abortions. More than half of all unsafe abortions occur in Asia, most of them in south and central Asia. In Latin American and Africa, the majority (approximately 3 out of 4) of all abortions are unsafe. In Africa, nearly half of all abortions occur under the least safe circumstances. - Lack of access to safe, affordable, timely and respectful abortion care, and the stigma associated with abortion, pose risks to women’s physical and mental well-being throughout the life-course.
Inaccessibility of quality abortion care risks violating a range of human rights of women and girls, including the right to life; the right to the highest attainable standard of physical and mental health; the right to benefit from scientific progress and its realization; the right to decide freely and responsibly on the number, spacing and timing of children; and the right to be free from torture, cruel, inhuman and degrading treatment and punishment.
Each year, 4.7–13.2% of maternal deaths can be attributed to unsafe abortion. In developed regions, it is estimated that 30 women die for every 100 000 unsafe abortions. In developing regions, that number rises to 220 deaths per 100 000 unsafe abortions. Estimates from 2012 indicate that in developing countries alone, 7 million women per year were treated in hospital facilities for complications of unsafe abortion. - Physical health risks associated with unsafe abortion include:
incomplete abortion (failure to remove or expel all pregnancy tissue from the uterus);
haemorrhage (heavy bleeding);
infection;
uterine perforation (caused when the uterus is pierced by a sharp object); and
damage to the genital tract and internal organs as a consequence of inserting dangerous objects into the vagina or anus. - Estimates from 2006 show that complications of unsafe abortions cost health systems in developing countries US$ 553 million per year for post-abortion treatments. In addition, households experienced US$ 922 million in loss of income due to long-term disability related to unsafe abortion. Countries and health systems could make substantial monetary savings by providing greater access to modern contraception and quality induced abortion.
- Evidence shows that restricting access to abortions does not reduce the number of abortions; however, it does affect whether the abortions that women and girls attain are safe and dignified. The proportion of unsafe abortions are significantly higher in countries with highly restrictive abortion laws than in countries with less restrictive laws.
Barriers to accessing safe and respectful abortion include high costs, stigma for those seeking abortions and health care workers, and the refusal of health workers to provide an abortion based on personal conscience or religious belief. Access is further impeded by restrictive laws and requirements that are not medically justified, including criminalization of abortion, mandatory waiting periods, provision of biased information or counselling, third-party authorization and restrictions regarding the type of health care providers or facilities that can provide abortion services.
"Preventing unsafe abortion"
[edit]"Preventing unsafe abortion". www.who.int. Retrieved 6 August 2019.
- Abortions are safe when they are carried out with a method that is recommended by WHO and that is appropriate to the pregnancy duration, and when the person carrying out the abortion has the necessary skills. Such abortions can be done using tablets (medical abortion) or a simple outpatient procedure.
An abortion is unsafe when it is carried out either by a person lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both. The people, skills, and medical standards considered safe in the provision of induced abortions are different for medical abortion (which is performed with drugs alone), and surgical abortion (which is performed with a manual or electric aspirator). Skills and medical standards required for safe abortion also vary depending upon the duration of the pregnancy and evolving scientific advances. - Based on data from 2010–2014, approximately 45% of all abortions worldwide were unsafe.
Of all unsafe abortions, one third were performed under the least safe conditions, i.e. by untrained persons using dangerous and invasive methods.
In Latin American and Africa, the majority (approximately 3 out of 4) of all abortions are unsafe.
Estimates from 2012 indicate that in developing countries alone, an estimated 7 million women per year were treated in hospital facilities for complications of unsafe abortion. - In Africa, nearly half of all abortions happen in the least safe circumstances. Moreover, mortality from unsafe abortion disproportionately affects women in Africa. While the continent accounts for 29% of all unsafe abortions, it sees 62% of unsafe abortion-related deaths (2).
- Health-care providers are obligated to provide life-saving medical care to any woman who suffers abortion-related complications, including treatment of complications from unsafe abortion, regardless of the legal grounds for abortion. However, in some cases, treatment of abortion complications is administered only on the condition that the woman provides information about the person(s) who performed the illegal abortion.
The practice of extracting confessions from women seeking emergency medical care as a result of illegal abortion puts women's lives at risk. The legal requirement for doctors and other health-care personnel to report cases of women who have undergone abortion, delays care and increases the risks to women’s health and lives. UN human rights standards call on countries to provide immediate and unconditional treatment to anyone seeking emergency medical care. - In addition to the deaths and disabilities caused by unsafe abortion, there are major social and financial costs to women, families, communities, and health systems.
Estimates from 2006 show that, in developing countries, the yearly cost for health systems include:
*US$ 553 million for treating complications from unsafe abortion.
*US$ 6 billion for treating post-abortion infertility.
*A need for an additional US$ 373 million, if unmet needs for treating complications from unsafe abortion were to be met. - Unsafe abortion can also lead to short- and long-term financial costs for women and ultimately entire families and communities. Annual cost estimates for developing countries include:
* US$ 200 million in out-of-pocket expenses of individuals and households, for the treatment of post-abortion complications, in sub-Saharan Africa alone.
*US$ 922 million in loss of income as a result of long-term disability, due to infertility or pelvic inflammatory disease caused by unsafe abortion.

