Spanish flu
Spanish flu, also known as the Great Influenza epidemic or the 1918 influenza pandemic, was an exceptionally deadly global influenza pandemic caused by the H1N1 influenza A virus. The earliest documented case was March 1918 in Kansas, United States, with further cases recorded in France, Germany and the United Kingdom in April. Two years later, nearly a third of the global population, or an estimated 500 million people, had been infected in four successive waves. Estimates of deaths range from 17 million to 50 million, and possibly as high as 100 million, making it one of the deadliest pandemics in human history.
"Spanish flu" is a misnomer. The pandemic broke out near the end of World War I, when wartime censors suppressed bad news in the belligerent countries to maintain morale, but newspapers freely reported the outbreak in neutral Spain, creating a false impression of Spain as the epicenter. Limited historical epidemiological data make the pandemic's geographic origin indeterminate, with competing hypotheses on the initial spread.
Quotes
[edit]
If you are up an about, protect healthy persons from infection-don’t spray others with the secretions from your nose and throat in coughing, sneezing, laughing, or talking. Cover the mouth with a handkerchief. Boil your handkerchiefs and other contaminated articles. Wash your hands frequently. Keep away from others as much as possible while you have a cough. ~ Bureau of Medicine and Surgery





The morgues were packed almost to the ceiling with bodies stacked one on top of another. The morticians worked day and night. You could never turn around without seeing a big red truck loaded with caskets for the train station so bodies could be sent home.
We didn’t have the time to treat them. We didn’t take temperatures; we didn’t even have time to take blood pressure.
We would give them a little hot whisky toddy; that’s about all we had time to do. They would have terrific nosebleeds with it. Sometimes the blood would just shoot across the room. You had to get out of the way or someone’s nose would bleed all over you. ~ Naval History and Heritage Command

- The outbreak began in 1918, during the final months of World War I, and historians now believe that the conflict may have been partly responsible for spreading the virus. On the Western Front, soldiers living in cramped, dirty and damp conditions became ill. This was a direct result of weakened immune systems from malnourishment. Their illnesses, which were known as "la grippe," were infectious, and spread among the ranks. Within around three days of becoming ill, many soldiers would start to feel better, but not all would make it.
During the summer of 1918, as troops began to return home on leave, they brought with them the undetected virus that had made them ill. The virus spread across cities, towns and villages in the soldiers' home countries. Many of those infected, both soldiers and civilians, did not recover rapidly. The virus was hardest on young adults between the ages of 20 and 30 who had previously been healthy.- All About History, ”Spanish flu: The deadliest pandemic in history”, Live Science, (March 12, 2020)
- Doctors were at a loss as to what to recommend to their patients; many physicians urged people to avoid crowded places or simply other people. Others suggested remedies included eating cinnamon, drinking wine or even drinking Oxo's meat drink (beef broth). Doctors also told people to keep their mouths and noses covered in public. At one point, the use of aspirin was blamed for causing the pandemic, when it might actually have helped those infected.
June 28, 1918, a public notice appeared in the British papers advising people of the symptoms of the flu; however, it turned out this was actually an advertisement for Formamints, a tablet made and sold by a vitamin company. Even as people were dying, there was money to be made by advertising fake "cures." The advert stated that the mints were the "best means of preventing the infective processes" and that everyone, including children, should suck four or five of these tablets a day until they felt better.
Americans were offered similar advice about how to avoid getting infected. They were advised not to shake hands with others, to stay indoors, to avoid touching library books and to wear masks. Schools and theaters closed, and the New York City Department of Health strictly enforced a Sanitary Code amendment that made spitting in the streets illegal, according to a review published in the journal Public Health Reports.- All About History, ”Spanish flu: The deadliest pandemic in history”, Live Science, (March 12, 2020)
- The Spanish flu remains the most deadly flu pandemic to date by a long shot, having killed an estimated 1% to 3% of the world's population.
The most recent comparable flu pandemic occurred in 2009 to 2010, after a new form of the H1N1 influenza strain appeared. The disease was named the "swine flu" because the virus that causes it is similar to one found in pigs (not because the virus came from pigs).
The swine flu caused respiratory illnesses that killed an estimated 151,700-575,400 people worldwide in the first year, according to the Centers for Disease Prevention and Control. That was about 0.001% to 0.007% of the world's population, so this pandemic was much less impactful than the 1918 Spanish flu pandemic. About 80% of the deaths caused by swine flu occurred in people younger than 65, which was unusual. Typically, 70% to 90% of deaths caused by seasonal influenza are in people older than 65.
A vaccine for the influenza strain that causes swine flu is now included in annual flu vaccines. People still die from the flu every year, but the numbers are far lower, on average, compared to those for the swine flu or Spanish flu pandemics. Annual epidemics of seasonal flu result in about 3 million to 5 million cases of severe illness and about 290,000 to 650,000 deaths, according to the World Health Organization.- All About History, ”Spanish flu: The deadliest pandemic in history”, Live Science, (March 12, 2020)
- Combating a disease of unknown cause is a daunting task. One hundred years ago, a pandemic of poorly understood etiology and transmissibility spread worldwide, causing an estimated 50 million deaths. Initially attributed to Haemophilus influenzae, it was not until the 1930s that an H1 subtype was identified as the causative strain. Subsequent influenza pandemics in 1957, 1968, and 2009 did not approach levels of morbidity and mortality comparable to those of the 1918 “Spanish flu,” leaving unanswered for almost a century questions regarding the extraordinary virulence and transmissibility of this unique strain.
- Belser, JA ; Tumpey, TM. “The 1918 flu, 100 years later”: Science. 2018 Jan. Vol. 359, Issue 6373, pp. 255
- Influenza is “grippe.” It is now spreading over the country in epidemic for. The last extensive epidemic occurred in 1889-90, and the disease was very prevalent for several years after.
The present epidemic disease is plain influenza. The term “Spanish influenza” has been applied because of its recent prevalence in Spain. Influenza occurs every year in the United States, but it is more contagious during an epidemic, and pneumonia is a more frequent complication.
Influenza is caused by a germ, the “influenza bacillus”, which lives but a short time outside of the body. Fresh air and sunshine kill the germ in a few minutes.
The disease is spread by the moist secretions from the noses and throats of infected persons.
Protect yourself from infection, keep well, and do not get hysterical over the epidemic.
Beware of those who are coughing and sneezing.
Avoid crowded street cars-walk to the office if possible.
Keep out of crowds-avoids theaters, moving-picture shows, and other places of public assembly.
Do not travel by railroad unless absolutely necessary.
Do not drink from glasses of cups which have been used by others unless you are sure they have been thoroughly cleansed.
You can do much to lessen the danger to yourself by keeping in good physical condition.
Avoid close, stuffy, and poorly ventilated rooms-insist upon fresh air, but avoid disagreeable drafts.
Eat simple, nourishing food and drink plenty of water. Avoid constipation.
Secure at least seven hours sleep. Avoid physical fatigue.
Do not sleep or sit around in damp clothing.
Keep the feet dry.
Influenza usually has a sudden onset with chillness, severe headache, and “aching all over.” At times the disease begins with nausea, vomiting, and abdominal pain. Fever begins early. Frequently catarrhal symptoms do not appear until later. When they do they are the symptoms of a bad cold I the head with a raw throat and dry cough. Weakness and prostration out of proportion to the fever are common. Former epidemics have been characterized by marked mental depression. In the present epidemic many of the cases are having a gradual onset-more like a gradually increasing cold in the head.
Practically, the great danger from influenza is pneumonia, which tends to follow in a considerable percent of the cases.- Bureau of Medicine and Surgery “Circular 1” “Influenza”, Directive from Washington, D.C., regarding treatment and procedures, September 26, 1918, Naval Districts and Shore Establishments.
- For the protection of others, if you are really sick stay at home and remain there until the fever is over. A day in bed at the very beginning may also save you from serious consequences later on.
If you are up an about, protect healthy persons from infection-don’t spray others with the secretions from your nose and throat in coughing, sneezing, laughing, or talking. Cover the mouth with a handkerchief. Boil your handkerchiefs and other contaminated articles. Wash your hands frequently. Keep away from others as much as possible while you have a cough.
If you become ill don’t try and keep on with your work. Fight the disease rationally and do not become unduly alarmed. In the average case recovery from acute symptoms follows in five or six days. To hasten recovery and lessen the danger of complications,, go to bed at once and keep the body a cathartic, such as 2 ½ or 3 grains of calomel, followed by a seidlitz powder or Epsom salts, is useful. Aspirin in 5 grain doses is useful for pain, but do not take large doses of aspirin, phenacetin, or other medicines. Send for the doctor.- Bureau of Medicine and Surgery “Circular 1” “Influenza”, Directive from Washington, D.C., regarding treatment and procedures, September 26, 1918, Naval Districts and Shore Establishments.
- The 1918 influenza pandemic was the most severe pandemic in recent history. It was caused by an H1N1 virus with genes of avian origin. Although there is not universal consensus regarding where the virus originated, it spread worldwide during 1918-1919. In the United States, it was first identified in military personnel in spring 1918. It is estimated that about 500 million people or one-third of the world’s population became infected with this virus. The number of deaths was estimated to be at least 50 million worldwide with about 675,000 occurring in the United States.
- While the 1918 H1N1 virus has been synthesized and evaluated, the properties that made it so devastating are not well understood. With no vaccine to protect against influenza infection and no antibiotics to treat secondary bacterial infections that can be associated with influenza infections, control efforts worldwide were limited to non-pharmaceutical interventions such as isolation, quarantine, good personal hygiene, use of disinfectants, and limitations of public gatherings, which were applied unevenly.
- In India, during the 1918 influenza pandemic, a staggering 12 to 13 million people died, the vast majority between the months of September and December. According to an eyewitness, “There was none to remove the dead bodies and the jackals made a feast.”
- Muara Chhun, “1918 flu pandemic killed 12 million Indians, and British overlords’ indifference strengthened the anti-colonial movement”, “The Conversation”, (April 17, 2020)
- When the first wave of the pandemic arrived, it was not particularly deadly. The only notice British officials took of it was its effect on some workers. A report noted, “As the season for cutting grass began … people were so weak as to be unable to do a full day’s work.”
By September, the story began to change. Mumbai was still the center of infection, likely due to its position as a commercial and civic hub. On Sept. 19, an English-language newspaper reported 293 influenza deaths had occurred there, but assured its readers “The worst is now reached.”
Instead, the virus tore through the subcontinent, following trade and postal routes. Catastrophe and death overwhelmed cities and rural villages alike. Indian newspapers reported that crematoria were receiving between 150 to 200 bodies per day. According to one observer, “The burning ghats and burial grounds were literally swamped with corpses; whilst an even greater number awaited removal.”
But influenza did not strike everyone equally. Most British people in India lived in spacious houses with gardens and yards, compared to the lower classes of city-dwelling Indians, who lived in densely populated areas. Many British also employed household staff to care for them – in times of health and sickness – so they were only lightly touched by the pandemic and were largely unconcerned by the chaos sweeping through the country.
In his official correspondence in early December, the Lieutenant Governor of the United Provinces did not even mention influenza, instead noting “Everything is very dry; but I managed to get two hundred couple of snipe so far this season.”- Muara Chhun, “1918 flu pandemic killed 12 million Indians, and British overlords’ indifference strengthened the anti-colonial movement”, The Conversation, (April 17, 2020)
- The small town of Gunnison, Colorado, lies at the bottom of the valley carved by the Gunnison River into the Rocky Mountains. It is now crossed by the Colorado stretch of U.S. Highway 50, but in 1918 the town was mainly supplied by train and two at best mediocre roads. When the 1918–19 influenza pandemic reached Colorado as an un- welcome stowaway on a train carrying servicemen from Montana to Boulder, the town of Gunnison took decisive action. As the November 1, 1918, edition of the Gunnison News-Champion documents, a Dr. Rockefeller from the nearby town of Crested Butte was “given entire charge of both towns and county to enforce a quarantine against all the world”. He instituted a strict reverse quarantine regime that almost en- tirely isolated Gunnison from the rest of the world. Gunnison became one of the few communities that largely escaped the ravages of the influenza pandemic, at least in the beginning. In an instructive example of the limited human patience for the social, psychological, and economic disruption of quarantine, adherence eventually waned, and the front page of the Gunnison News-Champion’s March 14, 1919, issue reports that the influenza pandemic got to Gunnison, too Nevertheless, Gunni- son had a very lucky escape, of a population of over 6900 (including the county), there were only a few cases and a single death.
- Chris von Csefalvay, "Modeling the control of infectious disease: Pharmacological and nonpharmacological interventions", Computational Modeling of Infectious Disease (2023).
- In the end, areas in the north and west of India saw death rates between 4.5% and 6% of their total populations, while the south and east – where the virus arrived slightly later, as it was waning – generally lost between 1.5% and 3%.
Geography wasn’t the only dividing factor, however. In Mumbai, almost seven-and-a-half times as many lower-caste Indians died as compared to their British counterparts - 61.6 per thousand versus 8.3 per thousand.- Muara Chhun, “1918 flu pandemic killed 12 million Indians, and British overlords’ indifference strengthened the anti-colonial movement”, The Conversation, (April 17, 2020)
- The 1918 flu almost certainly didn’t originate in Spain. One popular theory for how it acquired the “Spanish” name posits that Spain was the only country where you could read about the disease. That’s because Spain remained neutral during World War I, and therefore its newspapers weren’t censoring any information deemed harmful to national morale. The disease was also rampaging through other countries, including France, Germany, Britain, and the United States, but those governments suppressed or downplayed reports on the extent of the damage. Accurate and timely information is vital to combating a pandemic, but still, some countries’ first impulses are to cover up the spread of the disease.
- Joshua Keating, Strongman Medicine: Suspicious Numbers and Brutal Quarantines, Slate, (April 02, 2020).
- The origin of this pandemic has always been disputed and may never be resolved. However, the observations of trained observers at that time are worth noting because they may bear on later genomic analysis of the recently resurrected 1918 virus nucleotide fragments and the abortive "swine flu" epidemic of 1976. In Richard Shope's Harvey lecture of 1936, he reviews evidence that in the late summer or early autumn of 1918, a disease not previously recognized in swine, and closely resembling influenza in humans, appeared in the American Middle West. Epidemiologic-epizootiologic evidence strongly suggested that the causative virus was moving from humans to swine rather than in the reverse direction. Similar observations were made on the other side of the world and reported in a little-known paper in the National Medical Journal of China. In the spring of 1918, influenza in humans spread rapidly all over the world and was prevalent from Canton, China, to the most northern parts of Manchuria and from Shanghai to Szechuan. In October 1918, a disease diagnosed as influenza appeared in Russian and Chinese pigs in the area surrounding Harbin. Thus, epidemiologic evidence, fragmentary as it is, appears to favor the spread of virus from humans to swine, in which it remained relatively unchanged until it was recovered more than a decade later by Shope in the first isolation of influenza virus from a mammalian species.
The virus of 1918 was undoubtedly uniquely virulent, although most patients experienced symptoms of typical influenza with a 3- to 5-day fever followed by complete recovery. Nevertheless, although diagnostic virology was not yet available, bacteriology was flourishing and many careful postmortem examinations of patients by academic bacteriologists and pathologists disclosed bacterial pathogens in the lungs. However, this was a time when bacterial superinfection in other virus diseases could lead to death; for example, measles in military recruits was often fatal. This information is important in considering the question of "will there ever be another 1918." To the degree that secondary bacterial infection may contribute to influenza death rates, it should at least be partially controllable by antimicrobial agents, as indeed was the case in 1957.- Kilbourne ED. “Influenza pandemics of the 20th century”. Emerg Infect Dis. 2006 Jan;12(1):9-14.
- Owing to suspected cases of Spanish Influenza on the reservation every one is cautioned to take every care that they do not expose themselves or their neighbors.
And to observe the following rules:
Do not collect in a crowd any place.
Women and children remain at home. Stay in the open air and sunshine.
Keep the home aired out.
Have plenty of fresh air when you sleep
In case of storm keep dry and do not expose yourselves.
Do not mingle with others more than is necessary.
Do not go near where any one is sick or where a white flag is flying.
Do not go to the store unless it is necessary. If you have to go to the store or office your wants will be attended to on the porches.
If you get sick go to bed, in a tent is best, and notify the doctor at once. Lie down flat on your back and stay there.
Only one person in the family should go near the sick person.
Every one help the Superintendent and Doctor all they can by following these instructions and they will do all they can for you.- H D Lawshe, “Notice to occupants of Western Shoshone Agency Nevada, of rules for duration of the flu”, Bureau of Indian Affairs
- “You told people to wash your hands, don’t cough on people, stay at home, stay away from other people,” he said. “It was the patriotic thing to do to not cough on people or stay home if you were sick.”
But the thing that really drew public backlash were mask recommendations. As it turns out, resistance to wearing the face coverings isn’t new. People during the 1918 pandemic called them dirt traps and some clipped holes so they could smoke cigars.
In Europe, the Italian Supreme Command asked residents not to fail their cities by not wearing a mask. Several U.S. cities implemented mandates, describing them as a symbol of “wartime patriotism.” In San Francisco, Mayor James Rolph said, “conscience, patriotism and self-protection demand immediate and rigid compliance,” according to influenzaarchive.org. But some people refused to comply or take them seriously, Markel said.- Berkeley Lovelace Jr.; “Medical historian compares the coronavirus to the 1918 flu pandemic: Both were highly political”, CNBC, (Sep 28 2020; updated Sep 29 2020)
- Unlike today, there was no CDC or national public health department. The Food and Drug Administration existed but consisted of a very small group of men. Additionally, there were no antibiotics, intensive care units, ventilators, IV fluids or vaccines. “You got a bed or maybe nursing care,” Markel said.
But there was an epidemiologist much like Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, who withstood criticism for publicly pressing for safety protocols, according to Forbes.
“At the center of public health efforts in both states was a practical, plainspoken, bespectacled scientist: Dr. Thomas Dyer Tuttle, who became a powerful, if polarizing, figure in the fight against the Spanish flu,” according to Forbes.
Scientists hadn’t even seen a virus under the microscope at that point, said Graham Mooney, a medical historian at Johns Hopkins University School of Medicine. They didn’t have the technology and they knew almost nothing of virology, which was considered a nascent science because viruses are so small, he said. In fact, some scientists thought the 1918 virus was caused by a bacteria called Haemophilus influenzae, he said.- Berkeley Lovelace Jr.; “Medical historian compares the coronavirus to the 1918 flu pandemic: Both were highly political”, CNBC, (Sep 28 2020; updated Sep 29 2020)
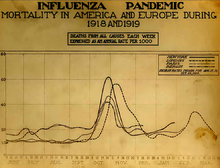
- “Influenza generally has a U shaped mortality curve, meaning it looks like a U, but the tops of the U are the most deadly,” Markel said. “But in 1918 it was a W shaped mortality curve and that upside-down part of the W, the V, was young people between ages 18 and 40 dying like flies. That was odd. That was not typical for previous flu pandemics or subsequent ones.”
It’s also important to consider population when talking about outbreaks or disasters, said Samantha Montano of the Massachusetts Maritime Academy, who studies disasters. In 1918, the world population was much smaller with an estimated 1.8 billion people. Today, there are nearly 8 billion on the planet.
Mooney echoed those remarks, saying, “We’re talking about a global population that is sort of smaller than it is now.” He said the death toll from 1918 virus likely had a great impact on the workforce who were unable to work from home or remotely like we can today.
“You end up having major structural, economic and social readjustments when you have such a massive death toll like that,” he said. “We have social welfare networks ... people travel around the globe. We have different societies and economies.”- Berkeley Lovelace Jr.; “Medical historian compares the coronavirus to the 1918 flu pandemic: Both were highly political”, CNBC, (Sep 28 2020; updated Sep 29 2020)
- I think the biggest lesson is that we can’t predict what influenza will do. In villages in Alaska, for example, the whole village would become sick at once. There would be nobody to provide food, nobody to provide shelter—these things can a make a difference. And even in wealthy nations like the United States, the conclusion at the end of 1918 and 1919 was that the single most important thing that could save your life from flu was good nursing care. Not medicines, not doctors, not hospitals, but good nursing care. When you first read those things you’re likely to say, “That can’t be true, what could they do in those days?” You know, what’s chicken soup going to do? What’s a blanket going to do? I believe the data, they’re strong, and some of the best and smartest physicians, nurses, and other observers said it again and again, "good nursing care."
- David M. Morens, M.D., National Institute of Allergy and Infectious Diseases, National Institutes of Health. Transcript: We Heard The Bells: The Influenza of 1918, Centers for Medicare & Medicaid Services, U.S. Department of Health and Human Services. Writer/Producer: Lisa Laden, December 4, 2009 .
- Spanish Flu victims suffered massive pneumonia and fatal pulmonary complications: they literally drowned in their own body fluids. Lungs filled with fluid and their skin became markedly discolored from the lack of oxygen. Mysteriously, it killed more young than old. The death rate was greatest among ages 15 to 40.
- Naval History and Heritage Command, “Influenza of 1918 (Spanish Flu) and the US Navy”
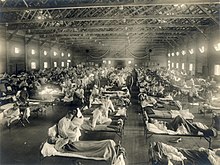
- Navy nurse Josie Brown, who served at Naval Hospital in Great Lakes, Illinois in 1918, later described what happened there and in many hospitals around the country:
The morgues were packed almost to the ceiling with bodies stacked one on top of another. The morticians worked day and night. You could never turn around without seeing a big red truck loaded with caskets for the train station so bodies could be sent home.
We didn’t have the time to treat them. We didn’t take temperatures; we didn’t even have time to take blood pressure.
We would give them a little hot whisky toddy; that’s about all we had time to do. They would have terrific nosebleeds with it. Sometimes the blood would just shoot across the room. You had to get out of the way or someone’s nose would bleed all over you.- Naval History and Heritage Command, “Influenza of 1918 (Spanish Flu) and the US Navy”
- In 1918, Navy and Marine patients totaling 121,225 were admitted at Navy medical facilities with influenza. Of these patients, 4,158 died of the virus, and sick patients spent over one million sick days in these facilities worldwide.
- Naval History and Heritage Command, “Influenza of 1918 (Spanish Flu) and the US Navy”
- The site of origin of the great pandemic of 1918 is unknown, but some choose to think that it was in the United States. Scattered outbreaks of disease were detected during the spring and early summer of 1918. Excess pneumonia-influenza deaths were evident from later tabulations by Wade Hampton Frost, who directed most of the epidemiologic investigations of this pandemic for the US Public Health Service. Many of the early outbreaks occurred in military installations as recruits poured into training camps to respond to the call for troops in Europe. Outbreaks also occurred on troop ships and among the American Expeditionary Forces in France by April 1918. The disease was soon evident among allied forces. A period of quiescence was noted in the United States during the summer. In some areas it was suspected that a reintroduction from Europe occurred in late summer and early autumn. However, in retrospect, it is evident that “seeding” of many geographic areas of the United States had occurred during the previous spring, that transmission was low during the summer but picked up rapidly as schools reopened in September. The first wave of the pandemic reached a crescendo by the end of October 1918. This was followed by a decline and recrudescence in midwinter 1919. The same pattern of occurrence was observed in the United States in 1957 with the next pandemic caused by influenza A (H2N2) (20).
- Glezen W Paul. “Emerging infections: pandemic influenza”. Epidemiol Rev. 1996;18(1):p.65
- The 1918 mortality numbers alone do not adequately describe the disaster. It was not just the weak and infirm who were taken away but the flower and strength of the land. The age-specific mortality curve did not trace the “U” describe above, but resembled a “W” with very high mortality rates in healthy young adults aged 20-40 years as well as in those less than 5 years of age and those aged 65 years and older (figure 1). No adequate explanation of this mortality pattern has been presented. It was wartime and young men were crowded together in military camps, but the mortality has highest in men of the same age who remained at home. Pregnancy was a risk factor, and this may provide some explanation for the high mortality in young women (23, 24). The fulminant nature of the clinical course of the fatal pneumonia casessuggests the the virus itself possessed a virulence not seen before nor since.
- Glezen W Paul. “Emerging infections: pandemic influenza”. Epidemiol Rev. 1996;18(1): p.66
- A mortality study in 17 cities in the USA during the 1918 influenza pandemic found that the cities which implemented mitigation strategies early on had a delayed, flatter epidemic curve, with a 50% lower peak mortality, and a 20% lower overall mortality. Thus, mitigating policies are of paramount importance to ensure that the burden on the health-care system remains manageable.
- Eskild Petersen, Marion Koopmans, Unyeong Go, Davidson H Hamer, Nicola Petrosillo, Francesco Castelli, Merete Storgaard, Sulien Al Khalili, Lone Simonsen; “Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics”, The Lancet, Volume 20, ISSUE 9, e238-e244, (September 01, 2020)
- They found that during the peak of the 1918 influenza outbreak in New York City, a total of 31,589 all-cause deaths (this included death from any cause) occurred among the 5.5 million residents that lived there at the time. The all-cause mortality in the peak of the influenza pandemic in 1918 was 2.8 times higher than during the same months in previous years.
In contrast, for the early 2020 COVID-19 outbreak in New York City, they found that 33,465 deaths from all causes occurred among 8.28 million residents between March 11 and May 11. The all-cause mortality in those months of 2020 were 4.15 times higher than those months between 2017 and 2019.
That means that in the peak of the 1918 influenza pandemic in NYC about 287 per 100,000 people died a month from any cause in NYC, whereas during the early COVID-19 outbreak, about 202 per 100,000 people died a month in the city. So the all-cause mortality during the spring of 2020 was 70% of the all cause mortality during the fall of 1918. "When we do that, we see that COVID-19 really does have the potential and has already unfortunately caused per capita death rates that were in the same ballpark," Faust told Live Science.- Yasemin Saplakoglu, “COVID-19 has the potential to be as deadly as the 1918 flu”, “Live Science”, (August 20, 2020)
- But there's another way to look at the deaths related to each pandemic: comparing deaths during a pandemic to the baseline that you'd expect during a particular time. There were more "excess deaths" during the 1918 flu than the early COVID-19 outbreak. But in relative terms, the COVID-19 outbreak in the spring actually looks worse, because the numbers quadrupled from pre-pandemic times (from a baseline of around 50 deaths per 100,000 people per month), whereas in the peak of the 1918 flu, the numbers less than tripled (from a baseline of around 100 deaths per 100,000 people per month).
"Its a bigger shock to our system, but that's a little bit unfair because we started off at a lower death rate," than there was in 1918, due to advances in hygiene, medicine, public health and safety, Faust said. Really, we don't yet know if the 1918 pandemic or the COVID-19 pandemic is more deadly, he added. Maybe what happened in New York in the spring was a "freak thing," before interventions such as masks and shutdowns took hold; or maybe the numbers will slowly creep up to match the death tolls seen in the 1918 flu until an effective vaccine is found.
One limitation of the study is that it's not possible to directly compare how infectious and harmful the two viruses are to people and it's unknown how many deaths from SARS-CoV-2 were prevented because of modern interventions that weren't available a century ago, the authors wrote.- Yasemin Saplakoglu, “COVID-19 has the potential to be as deadly as the 1918 flu”, “Live Science”, (August 20, 2020)
- Viruses are part of nature. They have attacked human beings—sometimes dangerously—in both distant and recent history. In 1918, the Spanish Flu killed nearly 700,000 in the United States and millions elsewhere.
- Richard D. Wolff, COVID-19 and the Failures of Capitalism (April 6, 2020), CounterPunch.
“Pandemic Influenza—Past, Present, Future: Communicating Today Based on the Lessons from the 1918-1919 Influenza Pandemic” (October 17, 2006)
[edit]“Pandemic Influenza—Past, Present, Future: Communicating Today Based on the Lessons from the 1918-1919 Influenza Pandemic”, U.S. Department of Health and Human Services Centers for Disease Control and Prevention, (October 17, 2006)

“Worry kills more people than the disease itself,” a Chicago public health official was quoted as saying. Other quotes were: “Don’t get scared,” and “The so-called Spanish influenza is nothing more or less than old fashioned grippe.”
Communication was rarely honest, because honesty would hurt morale. One of the first newspapers that started telling the truth in Milwaukee saw its editor jailed, so they stopped telling the truth. In Philadelphia, after a public health official finally closed all public gatherings and public funerals, the newspaper said, “This is not a public health measure.”


- No one really knows how many people died, but the first contemporary estimates put deaths at 21 million worldwide. That estimate is often still quoted, but it was certainly far worse than that. MacFarlane Burnett spent much of his life studying influenza, and he concluded that the worldwide death toll (from the 1918–1919 pandemic) was a minimum of 50 million, possibly 100 million. He may well have been right.
If you adjust for population, that could be 300 million today. In three weeks, it killed more people than AIDS has in 24 years. In the U.S., a reasonable estimate starts at 500,000 deaths. Personally, I am inclined toward a higher estimate of 700,000.
There was 15–53% morbidity. In San Antonio, over 90% of households had at least one family member with the illness. Most of the deaths occurred in healthy adults. In Army camps, the death toll was routinely over 5%, sometimes as much as 10%, and in some communities as high as 30%.- John Barry, p.5
- A big problem was you never knew if you were going to have the lethal kind, or normal flu. Regardless, it was gruesome. There were many with broken ribs from violent coughs. Air pockets also formed outside the lungs, and when you’d move these people it would sound like popping bubble wrap. Nose bleeds were common, less common was bleeding from mouth, and even bleeding from the eyes and ears.
- John Barry, p.5
- Context: We were at war. It was the first total war. It was the first time the government tried to fully control the public. The pandemic was known as Spanish flu, but we know it did not start in Spain. It was called Spanish Flu because Spain was not at war, so there was a free press. Most of Europe had a censored press. The U.S. press was more open, but still the new Sedition Act was passed. This was a law that made the Patriot Act look like it was written by the ACLU (American Civil Liberties Union). To enforce the law, the Justice Department issued badges to the “American Protective League” (APL), who was identified as Secret Service. Within a year, the attorney general said 200,000 APL members were operating in 1,000 communities. In Chicago, a “flying squad” of league members and police trailed, harassed, and beat members of the International Workers of the World (IWW). In Arizona, league members and vigilantes locked 1,200 IWW members and their “collaborators” into box cars and left them on a siding across the state line in the New Mexico desert. Throughout the country, the league's American Vigilance Patrol targeted “seditious street oratory,” sometimes calling upon the police to arrest speakers for disorderly conduct, sometimes acting more directly. Everywhere, the league spied on neighbors, investigated “slackers” and “food hoarders,” and demanded to know why people didn't buy—or didn't buy more—liberty bonds. At the same time, states outlawed the teaching of German. In Providence, Rhode Island, the Providence Journal carried a banner warning that “every German or Austrian in the United States unless known by years of association should be treated as a spy.” The problem was that the single largest ethnic group in the United States was German. 1918 was a time when there was a well-run propaganda machine. The government created the Committee for Public Information (CPI). It was intended to create one white-hot mass of determination. A quote by Arthur Bullard (who directed the CPI's Russian Division) summarizes the tenets of propaganda at the time, “Truth and falsehood are arbitrary terms... There is nothing in experience to tell us that one is always preferable to the other... There are lifeless truths and vital lies... The force of an idea lies in its inspirational value. It matters very little if it is true or false.”
Part of the propaganda machine included the energetic direction of Mississippi newspaper editor George Creel, an advisor to President Wilson. Under Creel, the CPI churned out national propaganda through diverse media. Creel organized the “Four-Minute Men,” a virtual army of volunteers who gave brief speeches wherever they could get an audience. There were 150,000 of the Four-Minute Men, who would propagandize for “four minutes” prior to any kind of public gathering. These men were charged with creating fear in the population because it was “an important element to be bred in the civilian population. It is difficult to unite a people by talking only on the highest ethical plain. To fight for an ideal, perhaps, must be coupled with thoughts of self-preservation.”- pp.6-7
- A pandemic meets the propaganda machine: During this time at least 25% of doctors and nurses were in the military. Additionally, national, local, and state officials all operated in the same way. At best, they communicated half-truths, or even out-right lies. As terrifying as the disease was, the officials made it more terrifying by making little of it, and they often underplayed it. Local officials said things like “if normal precautions are taken, there is nothing to fear” but then they would close all businesses.
“Worry kills more people than the disease itself,” a Chicago public health official was quoted as saying. Other quotes were: “Don’t get scared,” and “The so-called Spanish influenza is nothing more or less than old fashioned grippe.”
Communication was rarely honest, because honesty would hurt morale. One of the first newspapers that started telling the truth in Milwaukee saw its editor jailed, so they stopped telling the truth. In Philadelphia, after a public health official finally closed all public gatherings and public funerals, the newspaper said, “This is not a public health measure.”- p.7
- At the L.H. Shattuck Company, 45.9% of the workers stayed home. At the George A. Gilchrist shipyard 54.3% stayed home. At Freeport Shipbuilding 57% stayed home. At Groton Iron Works 58.3% stayed home. Even in an industry that was crucial to the war effort, absenteeism was high. Fear and terror was akin to the Black Plague. An internal American Red Cross report concluded, “A fear and panic of the influenza, akin to the terror of the Middle Ages regarding the Black Plague, [has] been prevalent in many parts of the country.”
- p.8
- It is important to understand that it was a special time in our history. WWI was at a crisis. It wasn’t clear that the war was about to end. Spanish Flu showed up right at the time that the German lines were breaking.
- Richard Hatchett, p.8
- 1918 case fatality rates in one-to-four year-olds is equivalent to what it would take now for 15–16 years of fatalities.
- Richard Hatchett, p.9
- Maternal mortality rates peaked in 1918 with 916 per 100,000 births. That means one per 1,000 births. The multiplying factor is enormous. There is not, however, a lot of specific data about pregnancy during that time.
- Richard Hatchett, p.9
- There is a tremendous amount of wishful thinking that the virus won’t come here. In 1918 the shaping of the cognitive environment varied dramatically from location to location some places elected officials and public officials locked arms on some things. Some tentative evidence shows that social distancing interventions did help. However, Baltimore is a case example of how to do it wron g (e.g., not close the schools). In Baltimore there were fights between elected officials and public health officials. Another example of doing it wrong was Pittsburgh. In Pittsburgh, the Mayor actually told the public to ignore the public health officials.
- Richard Hatchett, p.10
- I can say that often death notices for doctors and nurses showed up in tiny print in the newspapers. In many places the rates were high; morbidity over 50%. Logic suggests that social distancing measures helped, but I am not convinced that those interventions had an effect that was anything more than random. One can’t really generalize, because morbidity and mortality rates varied so much from community to community.
- John Barry p.10
- Los Angeles introduced interventions during the first few weeks of the epidemic, much earlier than New York, so they did not suffer the types of problems New York experienced. Baltimore newspapers published appeals to the public to minimize the use of telephones, but even at the height of the pandemic the phone system did not fail. Chicago attempted to estimate absenteeism. They estimated absenteeism averaged about 5% over a two-month period, not quite double thnormal average. Absenteeism peeked on October 22. However, the aggregate impact of absenteeism was significantly reduced. Economic impacts were modest, below 5%, when averaged out. A major recession did not ensue. Retail sales did decline in October, but they rebounded in November. New York City transit use, the Dow Jones, and business failures were indiscernible and modest when compared to the volatility of the period. Because of the short duration of the pandemic and human resiliency, it was characterized as a hit-and-run disease that only produced brief slowdowns.
- Richard Hatchett, p.13
- Cities were more isolated from each other. The pattern of the spread of the virus 1918 was related to troop movements. There has been a considerable amount of work on modeling from Department of Transportation (DOT) looking at connectivity of major urban centers to estimate how infectious diseases would spread now. In recent work looking at real world data, the geographic diffusion process is driven more by work-related travel.
- Richard Hatchett, p.14
- As bad as a bout of real seasonal influenza is, the H1 strain was far worse. It killed two percent or more of those stricken. In 1918, postmortem examinations helped understand if it was a case of flu. The performance of those autopsies was harrowing. Influenza defiled the lungs with bloody, frothy fluid. Instead of floating, the lungs plummeted to the bottom of water buckets during autopsies. The bronchials were fluid-filled, which explains the air hunger patients experienced. They frequently died from suffocation within 24–48 hours of developing symptoms. Some died later from secondary infections.
- Howard Markel p.17
- Thomas Wolfe wrote a literary masterpiece about the death of his brother. More fabled is how influenza altered the decision-making abilities of President Woodrow Wilson and his chief aide, Colonel Edward House. Both were in Europe to attend the Paris Peace Conferences—the famed gathering where Wilson hoped to sell his Points and establish a League of Nations. Colonel House, who arrived in Europe just weeks before the Armistice, contracted a severe bout of flu as he was negotiating with the other nations. In late February, as he was recuperating from his serious illness, Colonel House noted that, “When I fell ill in January, I lost the thread of affairs and I am not sure that I have ever gotten fully back.” To make matters worse, when Wilson was in Paris in mid-March, to work with the Big Four in the final stages of a comprehensive peace treaty, he, too, was stricken by influenza. Volumes have been written on how influenza may have altered the terms and negotiations of the Treaty of Versailles as it ravaged the bodies and thoughts of Woodrow Wilson and Edward House, among others.
While social historians of medicine warn against focusing too heavily on the illnesses of great men or the landmark cures of great doctors, the fact remains that when a world leader is struck down by influenza, in the midst of a pandemic that is accompanied by other global crises, the microbes’ power can be amplified above and beyond the symptoms it produces or the death it causes.- Howard Markel p.18
- In 1918, the childhood mortality rate for children under five-years-old was one in five. Every household knew of a child who died at a very young age, often of a contagious disease or dehydration issues. Back then, the care of the ill was almost exclusively at home. Today, death has been taken out of the household. Very few people have seen someone die today. In 1918, it was probably 90%. Death issues need to be talked about. For example, what should we do if public gatherings for funerals are cancelled? How will that affect people? There are social effects of quarantine, although now we have some resources to mitigate the effects. Public health departments (municipal, state, and federal) are all funded very differently. Post 9-11, bioterrorism preparedness efforts have been good for public health, because they are not mutually exclusive problems. Whether man-made or ecological, the strategies we need to use to address these problems are not that different.
- Howard Markel, p.19
- There are two great tragedies: The death of a child, or the death of a young child’s parent. Society saw a lot of both in 1918. There were many orphans in 1918. Several states put together orphan trains for adoption stops, which led to the establishment of the Child Welfare Department.
- John Barry, p.19
“Readiness for Responding to a Severe Pandemic 100 Years After 1918” (Deccember 2018)
[edit]Jester, B; Uyeki, T; Jernigan, D. “Readiness for Responding to a Severe Pandemic 100 Years After 1918”: American Journal of Epidemiology. Volume 187, Issue 12, (December 2018), pp. 2596–2602
- The 1918 influenza pandemic offers the worst-case planning scenario for public health officials because it resulted in unparalleled numbers of deaths. The virus, an A(H1N1) subtype, may have infected half the world’s population and caused at least 50 million deaths, according to estimates; 675,000 deaths are thought to have occurred in the United States. The source of the 1918 H1N1 virus is unknown; avian and swine origins have been proposed. Although 3 later pandemics, in 1957, 1968, and 2009, resulted in much lower estimated rates of morbidity and death, the threat of a 1918-like severity pandemic remains, because reports of human infections with novel influenza A viruses (generally of avian or swine origin) that pose pandemic potential have increased in recent years. In particular, Asian lineage avian influenza A (H7N9) viruses caused 1,557 reported human infections and at least 605 deaths during 5 epidemics in China during 2013–2017. Now, 100 years after the 1918 pandemic, is an important time to recall the significant impact of the pandemic and to reflect on the current state of readiness to respond to the next influenza pandemic.
- The world situation in 1918 exacerbated the effects of the pandemic. Wartime conditions combined with the intrinsic pathogenicity of the virus to cause tremendous morbidity and death rates. Poor sanitation, overcrowding, and limited health services during World War I facilitated disease transmission. Wartime overcrowding was rampant. Camps for troops, hastily built to accommodate 36,000, were soon housing 45,000 young and immunologically naïve soldiers. Each day in the summer of 1918, an average of 10,000 US soldiers crammed onto ships bound for France. Civilians flooding to cities in support of war industries quickly exceeded available housing capacity. With 30% of US physicians engaged in military service, medical personnel were in short supply when the pandemic struck.
- Treatment for influenza and its complications was mostly supportive care. Palliatives from pharmacies and vendors were encouraged, if not presented as cures. No antivirals or antibiotics were available; penicillin was not discovered until 1928. One potentially effective therapy for reducing the risk of death was use of convalescent sera collected from patients after their infection and administered to patients with current infection. Many more physicians, however, attempted to treat patients with “vaccines”. At the time, Haemophilus influenzae was the presumed etiologic agent for influenza, referred to as Pfeiffer’s bacillus. Vaccines were made from culture of the bacillus and may have been effective at reducing some secondary bacterial coinfections.
- The virulence of the 1918 H1N1 virus intensified the situation. Epidemiologic parameters of the 1918 pandemic, which include an attack rate of 28% and an estimated basic reproduction number of 1.8, were similar in subsequent influenza pandemics of 1957 and 1968. However, the estimated case fatality proportion of 1.7% in the 1918 pandemic was more than 10 times higher than in the 1957 and 1968 pandemics. Pandemic influenza in 1918 often presented with an unusually severe and swift clinical course. Disease frequently progressed to extensive organ involvement, primary viral pneumonia, and secondary bacterial pneumonia and empyema. Some military physicians reported a rapid clinical course, with death occurring within 24–48 hours after hospital admission. Pneumonia was the cause of death for the vast majority of the deceased. The unprecedented death rate exceeded the capacity of many morgues and funeral homes, and bodies were often “stacked like cord wood” in the halls of both military and civilian hospitals. Ultimately, the death toll, particularly among previously healthy young adults, reduced life expectancy in the United States by 12 years.
“The 1918 influenza pandemic: 100 years of questions answered and unanswered” (24 Jul 2019)
[edit]Jeffery K. Taubenberger et al., “The 1918 influenza pandemic: 100 years of questions answered and unanswered”, Science Translational Medicine, 24 Jul 2019: Vol. 11, Issue 502

- The founding 1918 pandemic virus is truly the “mother” of all subsequent influenza pandemics, and we are still in its “pandemic era” today. Its descendants are still evolving, still killing tens of thousands of people every year, with no end in sight.
- The pandemic (a geographically widespread or global infection in people) appeared in all but the remotest places on Earth, causing symptomatic disease in at least one-third of the world’s population. Whereas most sick persons had self-limiting influenza, indistinguishable from influenza as seen today, an unexpectedly high number went on to die of pneumonia. U.S. case fatality ratios were approximately 0.5 to 1%, but case fatality was much higher in many developing countries and in many crowded environments, from urban slums to Western military training camps. The global mortality will never be known with certainty, but estimates range from 50 million to as high as 100 million in the first pandemic year.
- The 1918 pandemic occurred in an era when viruses, as we know them today, were largely theoretical conceptualizations. Back in 1918, the extraordinarily high pandemic mortality, especially in young adults, frustrated physicians and scientists, who were unable to identify an etiological agent and thus were unable to diagnose and successfully treat the disease it caused. As virology matured as a scientific discipline, influenza A viruses were eventually isolated from pigs (1930) and from humans (1933). Serological data from the 1930s first suggested that the 1930s “classical” swine virus and the 1918 pandemic virus were closely related antigenically (23). This was later verified by viral genetic sequence analysis and by antigenic and pathogenesis studies. The subsequent pandemics, beginning with the 1957 H2N2 pandemic, revealed that new pandemic viruses could arise from previous pandemic viruses through genetic reassortment (Fig. 1). But where the 1918 virus had come from and what the basis of its severity had been remained among the most discussed medical mysteries throughout most of the 20th century. Solving that mystery was often referred to as a scientific “Holy Grail,” and few believed that it would ever be found. In 1976, historian Alfred Crosby (1931–2018) wrote that “It has been the dream of scientists working on influenza for over a half century to somehow obtain specimens of the virus of Spanish influenza, but only something as unlikely as a time capsule could provide them”.
- Remarkably, miniscule degraded viral RNA fragments recovered from just a few of the pandemic’s many millions of victims are now yielding, a century after their deaths, new insights into influenza virus biology and pathogenesis and are providing important lines of investigation into the prevention, treatment, and control of future pandemics.
- Pinpointing the origin of the 1918 pandemic virus, including discovering exactly how, where, and when it emerged to initiate sustained human-to-human pandemic transmission, will likely never be possible. Because human-adapted influenza A viruses are only moderately contagious and moderately fatal, it is the nature of influenza pandemics that many weeks, and more likely many months, must pass between the emergence of a pandemic and its detection. During this time, there would be relatively few deaths, given (relatively) low influenza case fatality, and those deaths that occurred would be difficult or impossible to recognize beneath the background of deaths from seasonal influenza and from other prevalent respiratory agents. It remains important to seek genomes of additional influenza viruses from the months and years before May 1918, when the earliest virally confirmed fatal 1918 case occurred. The hope is that new viral sequences identified from before 1918 will help to answer fundamental questions about the origin of the 1918 pandemic virus and population immunity before the pandemic, but the viral evolutionary and host adaptational sequences of events that bridge wild waterfowl gene constellations and pandemic viral genomes occur inside a “black box” that currently remains largely invisible to science. We have information about the genome of the 1918 virus at a very early stage of its emergence, but we do not yet know anything about evolutionary steps that may have occurred before it became adapted to human hosts.
- The bacteria most frequently associated with secondary infections after influenza in 1918–1919 were the pneumopathogens Streptococcus pneumoniae, Streptococcus pyogenes, and Staphylococcus aureus. Almost all of the tens of millions of deaths worldwide during the 1918 pandemic were associated with secondary bacterial infections, primarily with Gram-positive bacteria. Had it not been for secondary bacterial pneumonias caused by these and other pneumopathogens, the 1918 pandemic likely would have been associated with a far lower mortality. Increased susceptibility to secondary bacterial pneumonias in persons with influenza should be considered an intrinsic property of influenza virus pathogenicity, and this is likely to be the case for other pathogenic influenza viruses.
- A unique epidemiological feature of the 1918 influenza virus, related to its origin, was infection of both humans and swine. Influenza was first recognized as a clinical entity in swine in the United States in autumn 1918, concurrent with the spread of the pandemic in humans, having apparently been transmitted from humans to pigs. This host switch split the virus off into two independent viral lineages, one human and the other porcine. After 1918, the epizootic disease became widespread among herds of swine in the U.S. midwest. Epizootic viruses appeared annually thereafter, leading to Shope’s 1930 isolation of the first influenza virus, A/swine/Iowa/30, 3 years before the first human isolation of a descendant of the parent 1918 virus, A/WS/33. The two 1918 viral H1N1 lineages, one human and the other porcine, evolved and antigenically drifted at different rates until 2009. In the 2009 pandemic, the human-adapted H1N1 descendant was replaced by a different H1N1 virus that was also a 1918 viral descendant, ironically one that had been circulating enzootically in pigs. The original 1918 classical swine lineage still circulates enzootically today.
See also
[edit]External links
[edit] Media related to Spanish flu on Wikimedia Commons
Media related to Spanish flu on Wikimedia Commons

