Coronavirus disease 2019
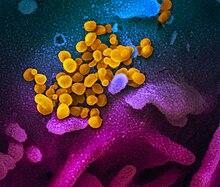
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease was first identified in December 2019 in Wuhan, the capital of China's Hubei province, and has since spread globally, resulting in the COVID-19 pandemic.
Quotes
[edit]- WHAT IS ALREADY KNOWN ABOUT THIS TOPIC?
Risk for severe COVID-19 increases with age, disability, and underlying medical conditions. The SARS-CoV-2 Omicron variant is more infectious but has been associated with less severe disease.
- WHAT IS ADDED BY THIS REPORT?
In-hospital mortality among patients hospitalized primarily for COVID-19 decreased from 15.1% (Delta period) to 4.9% (later Omicron period; April–June 2022), despite high-risk patient groups representing a larger proportion of hospitalizations. During the later Omicron period, the majority of in-hospital deaths occurred among adults aged ≥65 years (81.9%) and persons with three or more underlying medical conditions (73.4%).
- WHAT ARE THE IMPLICATIONS FOR PUBLIC HEALTH PRACTICE?
Vaccination, early treatment, and appropriate nonpharmaceutical interventions remain important public health priorities to prevent COVID-19 deaths, especially among persons most at risk.
- Some people who have been infected with the virus that causes COVID-19 can experience long-term effects from their infection, known as post-COVID conditions (PCC) or long COVID. The working was developed by the Department of Health and Human Services (HHS) in collaboration with CDC and other partners.
- People call post-COVID conditions by many names, including: Long COVID, long-haul COVID, post-acute COVID-19, post-acute sequelae of SARS CoV-2 infection (PASC), long-term effects of COVID, and chronic COVID.
- CDC Long COVID or Post-COVID Conditions (Updated Dec. 16, 2022 Español | Other Languages)
Disease characteristics
[edit]
"If you want to understand what an aerosol is, just think of somebody smoking," Osterholm told CNN. "If you can smell a cigarette in the location you're at, then you're breathing someone else's air that may have the virus in it. ~ Travis Caldwell



Now, even a quick, transient encounter can lead to an infection, Reiner added, including if someone's mask is loose, or a person quickly pulls their mask down, or an individual enters an elevator in which someone else has just coughed.
"This is how you can contract this virus," Reiner said. ~ Christina Maxouris quoting Jonathan Reiner

- Historian John Barry, who wrote the definitive account of the Spanish flu, “The Great Influenza,” noted there are significant differences between Covid infection and transmission and influenza infection and transmission. The incubation period — the time from exposure to illness — is longer with Covid. People are sick for longer; they’re infectious for longer, too.
“This is like influenza moving in very slow motion,” Barry said. Influenza pandemics have abrupt endings to their waves, with transmission dying out in any given location in a matter of weeks. That has not been the case with Covid. Instead, human behavior — societal shutdowns and reopenings — appear to be driving patterns.- John Barry as quoted by Helen Branswell in ”How the Covid pandemic ends: Scientists look to the past to see the future”, STAT, (May 19, 2021)
- "It's a very complicated receptor binding process compared to most virus spike proteins," Benton said. "Flu and HIV have a more simple activation process." The coronavirus is covered in spike proteins, and it's likely only a small fraction of them go through these conformational changes, bind to human cells and infect them, Benton said.
We know that the spike can adopt all these states that we were talking about," said co-lead author Antoni Wrobel, who is also a postdoctoral research fellow at the Francis Crick Institute's Structural Biology of Disease Processes Laboratory. "But whether each of the spikes adopts all of them we can't say because we can see only kind of snapshots."
The spike protein is very quick to change. In the lab, the spike can morph into all of these different conformations in less than 60 seconds, Wrobel told Live Science. But "this will be very different in a real infection; everything will be slower because the receptor will be stuck on the surface of a cell so you have to allow time for the virus to diffuse to this receptor," Benton said.
Why does the spike protein go through this many conformational changes to infect a cell? It "may be a way of the virus protecting itself from recognition by antibodies," Benton said. When the spike protein is in its closed states, it hides the site that binds with the receptor, maybe to avoid antibodies coming in and binding to that site instead, he said.- Donald Benton and Antoni Wrobel as quoted by Yasemin Saplakoglu in ”Coronavirus spike protein morphs into 10 different shapes to invade cells”, Live Science, (September 28, 2020)
- Aerosols containing Covid-19 can travel as easily as the smoke from a cigarette, Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said Friday.
"If you want to understand what an aerosol is, just think of somebody smoking," Osterholm told CNN. "If you can smell a cigarette in the location you're at, then you're breathing someone else's air that may have the virus in it."- Travis Caldwell, “The surge of Covid-19 infections for unvaccinated people is only beginning, experts warn”, CNN, July 31, 2021
- This study was the first study to examine the individual and synergistic effects of AT and RH on coronavirus survival on surfaces. The results show that when high numbers of the surrogates TGEV and MHV are deposited, these viruses may survive for days on surfaces at the ambient AT and wide range of RH levels (20 to 60% RH) typical of health care environments. TGEV and MHV may be more resistant to inactivation on surfaces than previously studied human coronaviruses, such as 229E (28). SARS-CoV has been reported to survive for 36 h on stainless steel, but the reductions in the levels observed were greater than those seen for either TGEV or MHV at 20°C at any RH in this study. However, the AT and RH conditions for the previous experiment were not reported, making comparisons difficult. Rabenau et al. reported much slower inactivation of SARS-CoV on a polystyrene surface (4 log10 reduction after 9 days; AT and RH conditions not reported), consistent with some observations for TGEV and MHV in the present study. There are some similarities with studies of another enveloped virus, human influenza virus, on surfaces in that at higher RH (50 to 60%), the inactivation kinetics are closer to those of TGEV and MHV.
- Lisa M. Casanova, Soyoung Jeon, William A. Rutala, David J. Weber, and Mark D. Sobsey; “Effects of Air Temperature and Relative Humidity on Coronavirus Survival on Surfaces”, Appl Environ Microbiol. 2010 May; 76(9): 2712–2717.
- The survival data for TGEV and MHV suggest that enveloped viruses can remain infectious on surfaces long enough for people to come in contact with them, posing a risk for exposure that leads to infection and possible disease transmission. This risk may also occur for other enveloped viruses, such as influenza virus (3, 4). The potential reemergence of SARS or the emergence of new strains of pandemic influenza virus, including avian and swine influenza viruses, could pose serious risks for nosocomial disease spread via contaminated surfaces. However, this risk is still poorly understood, and more work is needed to quantify the risk of exposure and possible transmission associated with surfaces. Statistical analysis showed that TGEV and MHV do not differ significantly in their inactivation kinetics on surfaces, and both viruses may be suitable models for survival and inactivation of SARS-CoV on surfaces. However, more data on the survival rates and inactivation kinetics of SARS-CoV itself are needed before these relationships with other coronaviruses can be definitively established. However, the findings of this study suggest that TGEV and MHV could serve as conservative surrogates for modeling exposure, transmission risk, and control measures for pathogenic enveloped viruses, such as SARS-CoV and influenza viruses, on health care surfaces.
- Lisa M. Casanova, Soyoung Jeon, William A. Rutala, David J. Weber, and Mark D. Sobsey; “Effects of Air Temperature and Relative Humidity on Coronavirus Survival on Surfaces”, Appl Environ Microbiol. 2010 May; 76(9): 2712–2717.
- For months, scientists have observed trends showing older people and men tend to be more vulnerable. Scientists know something about why children tend to have less serious infections from coronavirus -- they have fewer ACE2 receptors in their noses, and these receptors are how coronavirus gets into our cells. But they can't really explain why older people have such a high death rate from coronavirus -- much higher than from the common flu.
"What is it about age that makes you so much more susceptible to having disease?" Collignon questioned. "We've got the data and we know it's true ... but I don't think we've got all the answers for that."- Peter Collignon, as quoted in “Coronavirus has been with us for a year. Here's what we still don't know”, by Julia Hollingsworth, CNN, (28/12/2020)
- The problem, says Collignon, is that not enough money is spent on answering the basics.
"We spend billions of dollars on vaccines and drugs, but you can't get funding to do research on basics like how effective is this mask versus that mask," he said, adding that was partly because answers to those questions didn't make the problem go away -- they just decreased the risk.- Peter Collignon, as quoted in “Coronavirus has been with us for a year. Here's what we still don't know”, by Julia Hollingsworth, CNN, (28/12/2020)
- SARS-CoV-2 remained viable in aerosols throughout the duration of our experiment (3 hours), with a reduction in infectious titer from 103.5 to 102.7 TCID50 per liter of air. This reduction was similar to that observed with SARS-CoV-1, from 104.3 to 103.5 TCID50 per milliliter (Figure 1A).
SARS-CoV-2 was more stable on plastic and stainless steel than on copper and cardboard, and viable virus was detected up to 72 hours after application to these surfaces (Figure 1A), although the virus titer was greatly reduced (from 103.7 to 100.6 TCID50 per milliliter of medium after 72 hours on plastic and from 103.7 to 100.6 TCID50 per milliliter after 48 hours on stainless steel). The stability kinetics of SARS-CoV-1 were similar (from 103.4 to 100.7 TCID50 per milliliter after 72 hours on plastic and from 103.6 to 100.6 TCID50 per milliliter after 48 hours on stainless steel). On copper, no viable SARS-CoV-2 was measured after 4 hours and no viable SARS-CoV-1 was measured after 8 hours. On cardboard, no viable SARS-CoV-2 was measured after 24 hours and no viable SARS-CoV-1 was measured after 8 hours (Figure 1A).
Both viruses had an exponential decay in virus titer across all experimental conditions, as indicated by a linear decrease in the log10TCID50 per liter of air or milliliter of medium over time (Figure 1B). The half-lives of SARS-CoV-2 and SARS-CoV-1 were similar in aerosols, with median estimates of approximately 1.1 to 1.2 hours and 95% credible intervals of 0.64 to 2.64 for SARS-CoV-2 and 0.78 to 2.43 for SARS-CoV-1 (Figure 1C, and Table S1 in the Supplementary Appendix). The half-lives of the two viruses were also similar on copper. On cardboard, the half-life of SARS-CoV-2 was longer than that of SARS-CoV-1. The longest viability of both viruses was on stainless steel and plastic; the estimated median half-life of SARS-CoV-2 was approximately 5.6 hours on stainless steel and 6.8 hours on plastic (Figure 1C). Estimated differences in the half-lives of the two viruses were small except for those on cardboard (Figure 1C). Individual replicate data were noticeably “noisier” (i.e., there was more variation in the experiment, resulting in a larger standard error) for cardboard than for other surfaces (Fig. S1 through S5), so we advise caution in interpreting this result.
We found that the stability of SARS-CoV-2 was similar to that of SARS-CoV-1 under the experimental circumstances tested. This indicates that differences in the epidemiologic characteristics of these viruses probably arise from other factors, including high viral loads in the upper respiratory tract and the potential for persons infected with SARS-CoV-2 to shed and transmit the virus while asymptomatic.3,4 Our results indicate that aerosol and fomite transmission of SARS-CoV-2 is plausible, since the virus can remain viable and infectious in aerosols for hours and on surfaces up to days (depending on the inoculum shed). These findings echo those with SARS-CoV-1, in which these forms of transmission were associated with nosocomial spread and super-spreading events,5 and they provide information for pandemic mitigation efforts.- Neeltje van Doremalen, Trenton Bushmaker, Dylan H. Morris, Myndi G. Holbrook, Amandine Gamble, Brandi N. Williamson, Azaibi Tamin, Jennifer L. Harcourt, Natalie J. Thornburg, Susan I. Gerber, James O. Lloyd-Smith, Emmie de Wit, Vincent J. Munster; “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1”, N Engl J Med, (April 16, 2020); 382:1564-1567
- There’s no evidence yet to suggest any ethnic group is at greater risk of complications from the coronavirus because of a lack of immunity since the virus is new to all humans, said Dr. Jehan El-Bayoumi, founding director of the Rodham Institute at the George Washington University.
But other social and economic factors — such as nutrition, access to health care and poverty — do increase the risk of complications in indigenous and minority communities, El-Bayoumi said.
“We know that 80 percent of the outcomes related to any illness actually has nothing to do with access to health care, it is really the social determinants of health,” she said. “Those include water that you drink, the air that you breathe, the food that you eat, your education, your economic background, (or) systemic racism.”- Jehan El-Bayoumi as quoted by Linda Givetash, ”'They're so vulnerable': Coronavirus hits tribes of isolated Andaman Islands”, NBC News, (Sept. 2, 2020)
- Thomas Gilbert, an associate professor of chemistry and chemical biology at Northeastern University in Boston, Massachusetts, says coronavirus’s chemical make-up can be disrupted by nothing more specialised than cheap soap and warm water.
“These viruses have membranes that surround the genetic particles that are called lipid membranes, because they have an oily, greasy structure,” he says. “It’s this kind of structure than be neutralised by soap and water.” Dissolving this outer “envelope” breaks the virus cell up, and the genetic material – the RNA which hijacks human cells to make copies of the virus – is swept away and destroyed.
“I’ve heard of nothing yet to make the handwashing time shorter,” says Gilbert. “What you want to be doing is wetting your hands, getting the soap and working up a proper lather and then rubbing your hands for a good 20 seconds and get into all the nooks and crannies.” This gives enough time, Gilbert says, for the chemical reaction to take place between the lipid membrane and the soap. “There are other benefits – it also allows the soap to do a good job getting rid of the material.” And with warm water, Gilbert adds, all that virus fighting “happens a little quicker”.- Thomas Gilbert as quoted by Stephen Dowling in “Is a 20-second handwash enough to kill Covid-19?”, BBC Future, (20th August 2020)
- When SARS hit (the Southern China region) 17 years ago (in 2002-2003), Macau was lucky enough that it recorded only one imported case. But now, the (COVID-19) viral pneumonia coincides with the peak domestic travel season for Chinese New Year across China. That huge passenger traffic means the disease could be spread to each of the Chinese province.
- Ho Iat Seng (2020) cited in "Macau multi-stage response to pandemic risk: city chief" on GGR Asia, 23 January 2020.
- It was important to make the (COVID-19) disease notifiable. Although it did not appear to be as deadly as the previous SARS and MERS strains, there was still much to learn about it.
- Lance Jennings (2020) cited in: "China coronavirus checks: 'Looking for a needle in a haystack'" in RNZ, 27 January 2020.
- If the (COVID-19) infected (patient) droplets were sneezed at you by a patient and enters your eyes, they will eventually be washed from your eyes to your nose, as both are connected through what is known as a nasolacrimal duct.
- Paul Kellam (2020) cited in "Medical Experts Claim Wuhan Virus May Be Transmitted Through Your Eyes Or By Touch Alone" on World of Buzz, 31 January 2020.
- We didn't know until the last 24 hours.
- Brian Kemp, governor of Georgia, on that asymptomatic COVID-19 infected individuals can transmit the disease, in a CNN interview recorded in April 2020
- The SARS-CoV-2 virus is genetically closely related to severe acute respiratory syndrome coronavirus (SARS-CoV), the first pandemic threat of a novel and deadly coronavirus that emerged in late 2002 and caused an outbreak of severe acute respiratory syndrome (SARS). SARS-CoV was highly lethal but faded out after intense public health mitigation measures. By contrast, the novel SARS-CoV-2 that emerged in December, 2019, rapidly caused a global pandemic. The SARS 2003 outbreak ceased in June, 2003, with a global total of 8098 reported cases and 774 deaths, and a case fatality rate of 9•7%, with most cases being acquired nosocomially. In comparison, the Middle East respiratory syndrome coronavirus (MERS-CoV)—another deadly coronavirus, but which is currently not presenting a pandemic threat—emerged in 2012, and has caused 2494 reported cases and 858 deaths in 27 countries and has a very high case fatality rate of 34%. Because MERS-CoV is widespread in dromedary camels, zoonotic cases continue to occur, unlike SARS-CoV, which emerged from wildlife and was eliminated from the intermediate host reservoir.
The new coronavirus SARS-CoV-2 is less deadly but far more transmissible than MERS-CoV or SARS-CoV. The virus emerged in December, 2019, and as of June 29, 2020, 6 months into the first pandemic wave, the global count is rapidly approaching 10 million known cases and has passed 500 000 deaths. Because of its broad clinical spectrum and high transmissibility, eradicating SARS-CoV-2, as was done with SARS-CoV in 2003, does not seem a realistic goal in the short term.- Jason T. Ladner, Sierra N. Henson, Annalee S. Boyle, Anna L. Engelbrektson, Zane W. Fink, Fatima Rahee, Jonathan D’ambrozio, Kurt E. Schaecher, Mars Stone, Wenjuan Dong, Sanjeet Dadwal, Jianhua Yu, Michael A. Caligiuri, Piotr Cieplak, Magnar Bjørås, Mona H. Fenstad, Svein A. Nordbø, Denis E. Kainov, Norihito Muranaka, Mark S. Chee, Sergey A. Shiryaev, John A. Altin; “Epitope-resolved profiling of the SARS-CoV-2 antibody response identifies cross-reactivity with endemic human coronaviruses”. Cell Reports Medicine, 2021; 2 (1): 100189 DOI: 10.1016/j.xcrm.2020.100189
- There is nothing in recent history that compares to a contagious crisis of this magnitude, according to historians who study infectious diseases and disasters. The H1N1 flu pandemic in 2009 infected an estimated 60.8 million people in its first year, but the virus wasn’t nearly as severe as Covid-19, killing between 151,700 and 575,400 worldwide, according to the Centers for Disease Control and Prevention. MERS, another coronavirus that emerged in 2012, was much deadlier than Covid but significantly less infectious with only 2,494 reported cases.
- Berkeley Lovelace Jr., “Medical historian compares the coronavirus to the 1918 flu pandemic: Both were highly political”, CNBC, (Sep 28 2020; updated Sep 29 2020)
- China must have realized the epidemic did not originate in that Wuhan Huanan seafood market. The presumed rapid spread of the (COVID-19) virus apparently for the first time from the Huanan seafood market in December (2019) did not occur. Instead, the virus was already silently spreading in Wuhan, hidden amid many other patients with pneumonia at this time of year. The virus came into that marketplace before it came out of that marketplace.
- Daniel Lucey (2020) cited in "Scientists rush to find 'Patient Zero' in a bid to stop the coronavirus" on NZ Herald, 1 February 2020.
- At present (26 January 2020), the rate of development of the (COVID-19) epidemic is accelerating. I am afraid that it will continue for some time, and the number of cases may increase.
- Ma Xiaowei (2020) cited in "Wuhan Coronavirus Can Be Infectious Before People Show Symptoms, Official Claims" on Science Alert, 26 January 2020.
- Virus particles dilute rapidly outdoors. Virginia Tech aerosol expert Linsey Marr has compared it to a droplet of dye in the ocean: "If you happen to be right next to it, then maybe you'll get a whiff of it. But it's going to become diluted rapidly into the huge atmosphere."
- Linsey Marr as quoted by Sheila Mulrooney Eldred, “Coronavirus FAQ: I'm Vaccinated. I Thought I Could Give Up Masks! But Should I?, NPR, (July 26, 2021)
- Martin Michaelis, a professor of molecular science at the University of Kent in the UK, says water on its own is not enough to disable the virus. “When you have olive oil on your fingers when you’re cooking, it’s very hard to get rid of it with just water,” he says. “You need soap.” When it comes to the coronavirus, soap is needed in the same way “to remove that lipid envelope so that all the virus is deactivated”.
- Martin Michaelis as quoted by Stephen Dowling in “Is a 20-second handwash enough to kill Covid-19?”, BBC Future, (20th August 2020)
- If a person infected with the coronavirus sneezes, coughs or talks loudly, droplets containing particles of the virus can travel through the air and eventually land on nearby surfaces. But the risk of getting infected from touching a surface contaminated by the virus is low, says Emanuel Goldman, a microbiologist at Rutgers University.
"In hospitals, surfaces have been tested near COVID-19 patients, and no infectious virus can be identified," Goldman says.
What's found is viral RNA, which is like "the corpse of the virus," he says. That's what's left over after the virus dies.
"They don't find infectious virus, and that's because the virus is very fragile in the environment — it decays very quickly," Goldman says.
Back in January and February, scientists and public health officials thought surface contamination was a problem. In fact, early studies suggested the virus could live on surfaces for days.
It was assumed transmission occurred when an infected person sneezed or coughed on a nearby surface and "you would get the disease by touching those surfaces and then transferring the virus into your eyes, nose or mouth," says Linsey Marr, an engineering professor at Virginia Tech who studies airborne transmission of infectious disease.- Patti Neighmond quoting Emanuel Goldman and Linsey Marr; ”Still Disinfecting Surfaces? It Might Not Be Worth It”, Morning Edition, NPR, (December 28, 2020)
- Scientists now know that the early surface studies were done in pristine lab conditions using much larger amounts of virus than would be found in a real-life scenario.
Even so, many of us continue to attack door handles, packages and groceries with disinfectant wipes, and workers across the U.S. spend hours disinfecting surfaces in public areas like airports, buildings and subways.
There's no scientific data to justify this, says Dr. Kevin Fennelly, a respiratory infection specialist with the National Institutes of Health.
"When you see people doing spray disinfection of streets and sidewalks and walls and subways, I just don't know of any data that supports the fact that we're getting infected from viruses that are jumping up from the sidewalk."- Patti Neighmond quoting Kevin Fennelly, ”Still Disinfecting Surfaces? It Might Not Be Worth It”, Morning Edition, NPR, (December 28, 2020)
- It's still unclear whether that takes place (that COVID-19 can spread before people show signs of being infected). But if it does, that might explain why the disease is spreading so quickly.
- Malik Peiris (2020) cited in "Number of Coronavirus Cases Passes SARS Outbreak" on Learning English, 29 January 2020.
- Dr. Susan Rehm, vice chair at the Cleveland Clinic’s department of infectious diseases, said another reason flu incidences are low is because most people have some innate immunity from prior vaccinations and infections.
“COVID is a novel infection caused by the SARS coronavirus, and no one has any innate immunity to it,” she said. “So the population is probably overall more susceptible to it than maybe to influenza.”- Adrianna Rodriguez quoting Susan Rehm in “Record low flu cases show how COVID-19 is more contagious and 'less forgiving,' experts say”, USA TODAY, (January 11, 2021)
- "At the beginning of this pandemic... we all were taught, you have a significant exposure if you're within six feet of somebody and you're in contact with them for more than 15 minutes. All these rules are out the window," Reiner said. "This is a hyper-contagious virus."
Now, even a quick, transient encounter can lead to an infection, Reiner added, including if someone's mask is loose, or a person quickly pulls their mask down, or an individual enters an elevator in which someone else has just coughed.
"This is how you can contract this virus," Reiner said.- Christina Maxouris quoting Jonathan Reiner in “The Covid-19 case surge is altering daily life across the US. Things will likely get worse, experts warn”, CNN, January 1, 2022
- The first seropositive samples in our study were already detected during the week of 23 February, one week before the first confirmed case of SARS-CoV-2 in NYC was identified, which suggests that SARS-CoV-2 was probably introduced to the NYC area several weeks earlier than has previously been assumed. This would not be unexpected given the unique diversity and connectivity of NYC and the large numbers of travellers that were arriving from SARS-CoV-2-affected regions of the world in January and February 2020. The antibody titres of initial positive individuals were low, which is consistent with slower seroconversion of perhaps mild cases. Of course, we cannot exclude with absolute certainty that some of the lower positive titres are false positives as the initially low seroprevalence falls within the confidence intervals of the positive predictive value.
Of note, the seroprevalence in the routine care group (as well as the urgent care group at the end of May, after the peak) falls significantly below the threshold for potential community immunity, which has been estimated by one study to require at least a seropositivity rate of 67% for SARS-CoV-24. On the basis of the population of NYC (8.4 million), we estimate that by the week ending 24 May, approximately 1.7 million individuals had been infected with SARS-CoV-2. Taking into account the cumulative number of deaths in the city by 19 May (16,674—this number includes only officially confirmed, not suspected, COVID-19-related deaths), this suggests a preliminary infection fatality rate of 0.97% (with the assumption that both seroconversion and death occur with similar delays). This is in stark contrast to the infection fatality rate of the 2009 H1N1 pandemic, which was estimated to be 0.01–0.001%.- Daniel Stadlbauer, Jessica Tan, Kaijun Jiang, Matthew M. Hernandez, Shelcie Fabre, Fatima Amanat, Catherine Teo, Guha Asthagiri Arunkumar, Meagan McMahon, Christina Capuano, Kathryn Twyman, Jeffrey Jhang, Michael D. Nowak, Viviana Simon, Emilia Mia Sordillo, Harm van Bakel & Florian Krammer; “Repeated cross-sectional sero-monitoring of SARS-CoV-2 in New York City”, Nature, (03 November 2020)
- Both influenza and coronaviruses cause respiratory tract infection that can lead to morbidity and mortality, especially in those who are immunocompromised or who have no existing immunity to the viruses. Indeed, while the COVID-19 should not be taken lightly, influenza is a much bigger problem, but because it is relatively common and has been around for a long time, it does not receive the attention that new viral outbreaks do. The COVID-19 is scary because it is new and we do not know a lot about it yet. New viruses are always scary because we have little to no protective immunity against them and we do not have vaccines. There is work going on to understand and develop preventive strategies to deal with this COVID-19 threat. However, universal precautions to limit its spread are very important right now until a new vaccine or another strategy is available.
- Jeffrey A. Woods, as quoted in “Should, and how can, exercise be done during a coronavirus outbreak? An interview with Dr. Jeffrey A. Woods”, by Weimo Zhu, J Sport Health Sci. (2020 Mar Published online 2020 Feb 4); 9(2): 105–107.
- Many of Arkansas Children’s new COVID-19 patients are also much more ill than before. They’re coming in with wrecked lungs, struggling to breathe; they’re not bouncing back with typical youthful resilience, despite having been very healthy before. “This COVID surge, I’ve never seen anything like it,” Linda Young, a respiratory therapist who’s been on the job for 37 years, told me. “It’s the sickest I’ve ever seen children.” It’s become common for more than half of the kids in the ICU to be on ventilators. A few have been in the hospital for more than a month. “We are not able to discharge them as fast as they are coming,” Abdallah Dalabih, a pediatric critical-care physician, told me. Some parents, Snowden said, are in disbelief. “Many people didn’t believe kids could get this thing,” she said.
- Katherine J. Wu, “Delta Is Bad News for Kids”, The Atlantic, (August 10, 2021)
- Amid all the chaos is perhaps one tentative silver lining for children. The new variant appears to be following the long-standing trend that kids are, on average, more resistant to the coronavirus’s effects. Although Delta is a more cantankerous version of the virus than its predecessors, researchers don’t yet have evidence that it is specifically worse for children, who are still getting seriously sick only a small fraction of the time. Less than 2 percent of known pediatric COVID-19 cases, for instance, result in hospitalization, sometimes far less.
- Katherine J. Wu, “Delta Is Bad News for Kids”, The Atlantic, (August 10, 2021)
- Kids’ bodies can and do fight back, though an explanation for their tenacity remains elusive. One idea posits that kids’ airway cells might be tougher for the coronavirus to break into, Stephanie Langel, an immunologist at Duke University, told me. Another proposes that their immune system is especially adept at churning out an alarm molecule that buttresses the body against infection. Kids, Langel said, might even have a way of marshaling certain antibodies faster than adults, stamping out the virus before it has a chance to infiltrate other tissues.
- Katherine J. Wu, “Delta Is Bad News for Kids”, The Atlantic, (August 10, 2021)
- I say "possibly" (for the SARS-CoV-2 to more dangerous to humans than the other coronaviruses) because so far, not only do we not know how dangerous it is, we can't know. Outbreaks of new viral diseases are like the steel balls in a pinball machine: You can slap your flippers at them, rock the machine on its legs and bonk the balls to the jittery rings, but where they end up dropping depends on 11 levels of chance as well as on anything you do. This is true with coronaviruses in particular: They mutate often while they replicate, and can evolve as quickly as a nightmare ghoul.
- Shi Zhengli (2020) cited in "We Made the Coronavirus Epidemic" on The New York Times, 28 January 2020.
“Covid may no longer be the most 'significant' threat to health, Dr Jenny Harries says” (10 October 2021)
[edit]Danielle Sheridan, Covid may no longer be the most 'significant' threat to health, Dr Jenny Harries says, Telegraph, (10 October 2021).
- Covid may no longer be the most "significant" threat to health, Dr Jenny Harries has said.
- The chief executive of the UK Health Security Agency said today that Covid was possibly no more dangerous than flu.
“The coronavirus is mutating — does it matter?” (9/8/2020)
[edit]Ewen Callaway, “The coronavirus is mutating — does it matter?”, Nature, (08 September 2020; correction 16 September 2020), 585, pp.174-177.



- When COVID-19 spread around the globe this year, David Montefiori wondered how the deadly virus behind the pandemic might be changing as it passed from person to person. Montefiori is a virologist who has spent much of his career studying how chance mutations in HIV help it to evade the immune system. The same thing might happen with SARS-CoV-2, he thought.
In March, Montefiori, who directs an AIDS-vaccine research laboratory at Duke University in Durham, North Carolina, contacted Bette Korber, an expert in HIV evolution and a long-time collaborator. Korber, a computational biologist at the Los Alamos National Laboratory (LANL) in New Mexico, had already started scouring thousands of coronavirus genetic sequences for mutations that might have changed the virus’s properties as it made its way around the world.
Compared with HIV, SARS-CoV-2 is changing much more slowly as it spreads. But one mutation stood out to Korber. It was in the gene encoding the spike protein, which helps virus particles to penetrate cells. Korber saw the mutation appearing again and again in samples from people with COVID-19. At the 614th amino-acid position of the spike protein, the amino acid aspartate (D, in biochemical shorthand) was regularly being replaced by glycine (G) because of a copying fault that altered a single nucleotide in the virus’s 29,903-letter RNA code. Virologists were calling it the D614G mutation.
In April, Korber, Montefiori and others warned in a preprint posted to the bioRxiv server that “D614G is increasing in frequency at an alarming rate”1. It had rapidly become the dominant SARS-CoV-2 lineage in Europe and had then taken hold in the United States, Canada and Australia. D614G represented a “more transmissible form of SARS-CoV-2”, the paper declared, one that had emerged as a product of natural selection. - Viruses that encode their genome in RNA, such as SARS-CoV-2, HIV and influenza, tend to pick up mutations quickly as they are copied inside their hosts, because enzymes that copy RNA are prone to making errors. After the severe acute respiratory syndrome (SARS) virus began circulating in humans, for instance, it developed a kind of mutation called a deletion that might have slowed its spread.
But sequencing data suggest that coronaviruses change more slowly than most other RNA viruses, probably because of a ‘proofreading’ enzyme that corrects potentially fatal copying mistakes. A typical SARS-CoV-2 virus accumulates only two single-letter mutations per month in its genome — a rate of change about half that of influenza and one-quarter that of HIV, says Emma Hodcroft, a molecular epidemiologist at the University of Basel, Switzerland.
Other genome data have emphasized this stability — more than 90,000 isolates have been sequenced and made public (see www.gisaid.org). Two SARS-CoV-2 viruses collected from anywhere in the world differ by an average of just 10 RNA letters out of 29,903, says Lucy Van Dorp, a computational geneticist at University College London, who is tracking the differences for signs that they confer an evolutionary advantage.
Despite the virus’s sluggish mutation rate, researchers have catalogued more than 12,000 mutations in SARS-CoV-2 genomes. But scientists can spot mutations faster than they can make sense of them. Many mutations will have no consequence for the virus’s ability to spread or cause disease, because they do not alter the shape of a protein, whereas those mutations that do change proteins are more likely to harm the virus than improve it (see ‘A catalogue of coronavirus mutations’). “It’s much easier to break something than it is to fix it,” says Hodcroft, who is part of Nextstrain, an effort to analyse SARS-CoV-2 genomes in real time. - Many researchers suspect that if a mutation did help the virus to spread faster, it probably happened earlier, when the virus first jumped into humans or acquired the ability to move efficiently from one person to another. At a time when nearly everyone on the planet is susceptible, there is likely to be little evolutionary pressure on the virus to spread better, so even potentially beneficial mutations might not flourish. “As far as the virus is concerned, every single person that it comes to is a good piece of meat,” says William Hanage, an epidemiologist at the Harvard T. H. Chan School of Public Health in Boston, Massachusetts. “There’s no selection to be doing it any better.”
- D614G was first spotted in viruses collected in China and Germany in late January; most scientists suspect the mutation arose in China. It’s now almost always accompanied by three mutations in other parts of the SARS-CoV-2 genome — possible evidence that most D614G viruses share a common ancestor.
D614G’s rapid rise in Europe drew Korber’s attention. Before March — when much of the continent went into lockdown — both unmutated ‘D’ viruses and mutated ‘G’ viruses were present, with D viruses prevalent in most of the western European countries that geneticists sampled at the time. In March, G viruses rose in frequency across the continent, and by April they were dominant, reported Korber, Montefiori and their team. - The first team to report pseudovirus experiments on D614G, in June, was led by Hyeryun Choe and Michael Farzan, virologists at the Scripps Research Institute in La Jolla, California5. Several other teams have posted similar studies on bioRxiv (Montefiori’s experiments, and those of another collaborator, appeared in the Cell paper2). The teams used different pseudovirus systems and tested them on various kinds of cell, but the experiments pointed to the same conclusion: viruses carrying the G mutation infected cells much more ably than did D viruses — up to ten times more efficiently, in some cases.
In laboratory tests, “all of us agree that D to G is making the particles more infectious”, says Jeremy Luban, a virologist at the University of Massachusetts Medical School in Worcester. But these studies come with many caveats — and their relevance to human infections is unclear. “What’s irritating are people taking their results in very controlled settings, and saying this means something for the pandemic. That, we are so far away from knowing,” says Grubaugh. The pseudoviruses carry only the coronavirus spike protein, in most cases, and so the experiments measure only the ability of these particles to enter cells, not aspects of their effects inside cells, let alone on an organism. They also lack the other three mutations that almost all D614G viruses carry. “The bottom line is, they’re not the virus,” says Luban. - Some labs are now working with infectious SARS-CoV-2 viruses that differ by only the single amino acid. These are tested in laboratory cultures of human lung and airway cells, and in lab animals such as ferrets and hamsters. For labs with the experience and the biosafety capabilities to manipulate viruses, “this is like bread-and-butter kind of work”, says Sheahan. The first of those studies, led by researchers at the University of Texas Medical Branch in Galveston, was reported in a 2 September preprint6. It found that viruses with the mutation were more infectious than were D viruses in a human lung cell line and in airway tissues, and that mutated viruses were present at greater levels in the upper airways of infected hamsters6.
Even these experiments might not offer absolute clarity. Some studies show that certain mutations to the spike protein in the Middle East respiratory syndrome (MERS) virus can cause more-severe disease in mice — yet other mutations in the protein show very little effect in people or in camels, the likely reservoir for human MERS infections, says Stanley Perlman, a coronavirologist at the University of Iowa in Iowa City. - Grubaugh thinks that D614G has received too much attention from scientists, in part because of the high-profile papers it has garnered. “Scientists have this crazy fascination with these mutations,” he says. But he also sees D614G as a way to learn about a virus that doesn’t have much in the way of genetic diversity. “The virologist in me looks at these things and says it would be a lot of fun to study,” he says. “It creates this whole rabbit hole of different things you can go into.”
- A team led by virologists Theodora Hatziioannou and Paul Bieniasz, at Rockefeller University in New York City, genetically modified the vesicular stomatitis virus — a livestock pathogen — so that it used the SARS-CoV-2 spike protein to infect cells, and grew it in the presence of neutralizing antibodies. Their goal was to select for mutations that enabled the spike protein to evade antibody recognition. The experiment generated spike-protein mutants that were resistant to antibodies taken from the blood of people who had recovered from COVID-19, as well as to potent ‘monoclonal’ antibodies that are being developed into therapies. Every one of the spike mutations was found in virus sequences isolated from patients, report Hatziioannou, Bieniasz and their team — although at very low frequencies that suggest positive selection is not yet making the mutations more common11.
Other scientists are trying to stay ahead of SARS-CoV-2’s evolution by predicting which mutations are likely to be important. Jesse Bloom, an evolutionary virologist at the Fred Hutchinson Cancer Research Center in Seattle, Washington, led a team that created nearly 4,000 mutated versions of the spike protein’s RBD, and measured how the alterations affected the expression of the spike protein and its ability to bind to ACE2. Most of the mutations had no effect on or hindered these properties, although a handful improved them. Some of these mutations have been identified in people with COVID-19, but Bloom’s team found no signs of natural selection for any of the variants. “Probably the virus binds to ACE2 about as well as it needs to right now,” he says. - Studies of common-cold coronaviruses, sampled across multiple seasons, have identified some signs of evolution in response to immunity. But the pace of change is slow, says Volker Thiel, an RNA virologist at the Institute of Virology and Immunology in Bern. “These strains remain constant, more or less.”
- With most of the world still susceptible to SARS-CoV-2, it’s unlikely that immunity is currently a major factor in the virus’s evolution. But as population-wide immunity rises, whether through infection or vaccination, a steady trickle of immune-evading mutations could help SARS-CoV-2 to establish itself permanently, says Sheahan, potentially causing mostly mild symptoms when it infects individuals who have some residual immunity from a previous infection or vaccination. “I wouldn’t be surprised if this virus is maintained as a more common, cold-causing coronavirus.” But it’s also possible that our immune responses to coronavirus infections, including to SARS-CoV-2, aren’t strong or long-lived enough to generate selection pressure that leads to significantly altered virus strains.
Worrisome mutations could also become more common if antibody therapies aren’t used wisely — if people with COVID-19 receive one antibody, which could be thwarted by a single viral mutation, for example. Cocktails of monoclonal antibodies, each of which can recognize multiple regions of the spike protein, might lessen the odds that such a mutation will be favoured through natural selection, researchers say. Vaccines arouse less concern on this score because, like the body’s natural immune response, they tend to elicit a range of antibodies.
“Similarities and Differences between Flu and COVID-19”
[edit]CDC, “Similarities and Differences between Flu and COVID-19”
- COVID-19 seems to spread more easily than flu and causes more serious illnesses in some people. It can also take longer before people show symptoms and people can be contagious for longer.
- Because some of the symptoms of flu and COVID-19 are similar, it may be hard to tell the difference between them based on symptoms alone, and testing may be needed to help confirm a diagnosis.
- COVID-19 seems to cause more serious illnesses in some people. Other signs and symptoms of COVID-19, different from flu, may include change in or loss of taste or smell.
- While COVID-19 and flu viruses are thought to spread in similar ways, COVID-19 is more contagious among certain populations and age groups than flu. Also, COVID-19 has been observed to have more superspreading events than flu.
“Profile of a killer: the complex biology powering the coronavirus pandemic” (04 May 2020)
[edit]David Cyranoski, “Profile of a killer: the complex biology powering the coronavirus pandemic”, Nature, (04 May 2020), 581, pp.22-26


These differences have led to some confusion about the lethality of SARS-CoV-2. Some experts and media reports describe it as less deadly than SARS-CoV because it kills about 1% of the people it infects, whereas SARS-CoV killed at roughly ten times that rate. But Perlman says that’s the wrong way to look at it. SARS-CoV-2 is much better at infecting people, but many of the infections don’t progress to the lungs. “Once it gets down in the lungs, it’s probably just as deadly,” he says.

Rambaut, too, doubts that the virus will become milder over time and spare its host. “It doesn’t work that way,” he says. As long as it can successfully infect new cells, reproduce and transmit to new ones, it doesn’t matter whether it harms the host, he says.
- In 1912, German veterinarians puzzled over the case of a feverish cat with an enormously swollen belly. That is now thought to be the first reported example of the debilitating power of a coronavirus. Veterinarians didn’t know it at the time, but coronaviruses were also giving chickens bronchitis, and pigs an intestinal disease that killed almost every piglet under two weeks old.
The link between these pathogens remained hidden until the 1960s, when researchers in the United Kingdom and the United States isolated two viruses with crown-like structures causing common colds in humans. Scientists soon noticed that the viruses identified in sick animals had the same bristly structure, studded with spiky protein protrusions. Under electron microscopes, these viruses resembled the solar corona, which led researchers in 1968 to coin the term coronaviruses for the entire group.
It was a family of dynamic killers: dog coronaviruses could harm cats, the cat coronavirus could ravage pig intestines. Researchers thought that coronaviruses caused only mild symptoms in humans, until the outbreak of severe acute respiratory syndrome (SARS) in 2003 revealed how easily these versatile viruses could kill people. - Of the viruses that attack humans, coronaviruses are big. At 125 nanometres in diameter, they are also relatively large for the viruses that use RNA to replicate, the group that accounts for most newly emerging diseases. But coronaviruses really stand out for their genomes. With 30,000 genetic bases, coronaviruses have the largest genomes of all RNA viruses. Their genomes are more than three times as big as those of HIV and hepatitis C, and more than twice influenza’s.
Coronaviruses are also one of the few RNA viruses with a genomic proofreading mechanism — which keeps the virus from accumulating mutations that could weaken it. That ability might be why common antivirals such as ribavirin, which can thwart viruses such as hepatitis C, have failed to subdue SARS-CoV-2. The drugs weaken viruses by inducing mutations. But in the coronaviruses, the proofreader can weed out those changes.
Mutations can have their advantages for viruses. Influenza mutates up to three times more often than coronaviruses do, a pace that enables it to evolve quickly and sidestep vaccines. But coronaviruses have a special trick that gives them a deadly dynamism: they frequently recombine, swapping chunks of their RNA with other coronaviruses. Typically, this is a meaningless trading of like parts between like viruses. But when two distant coronavirus relatives end up in the same cell, recombination can lead to formidable versions that infect new cell types and jump to other species, says Rambaut. - Estimates for the birth of the first coronavirus vary widely, from 10,000 years ago to 300 million years ago. Scientists are now aware of dozens of strains3, seven of which infect humans. Among the four that cause common colds, two (OC43 and HKU1) came from rodents, and the other two (229E and NL63) from bats. The three that cause severe disease — SARS-CoV (the cause of SARS), Middle East respiratory syndrome MERS-CoV and SARS-CoV-2 — all came from bats. But scientists think there is usually an intermediary — an animal infected by the bats that carries the virus into humans. With SARS, the intermediary is thought to be civet cats, which are sold in live-animal markets in China.
The origin of SARS-CoV-2 is still an open question (see ‘Family of killers’). The virus shares 96% of its genetic material with a virus found in a bat in a cave in Yunnan, China4 — a convincing argument that it came from bats, say researchers. But there’s a crucial difference. The spike proteins of coronaviruses have a unit called a receptor-binding domain, which is central to their success in entering human cells. The SARS-CoV-2 binding domain is particularly efficient, and it differs in important ways from that of the Yunnan bat virus, which seems not to infect people5.
Complicating matters, a scaly anteater called the pangolin showed up with a coronavirus that had a receptor-binding domain almost identical to the human version. But the rest of the coronavirus was only 90% genetically similar, so some researchers suspect the pangolin was not the intermediary5. The fact that both mutations and recombinations are at work complicates efforts to draw a family tree. - Although the known human coronaviruses can infect many cell types, they all mainly cause respiratory infections. The difference is that the four that cause common colds easily attack the upper respiratory tract, whereas MERS-CoV and SARS-CoV have more difficulty gaining a hold there, but are more successful at infecting cells in the lungs.
SARS-CoV-2, unfortunately, can do both very efficiently. That gives it two places to get a foothold, says Shu-Yuan Xiao, a pathologist at the University of Chicago, Illinois. A neighbour’s cough that sends ten viral particles your way might be enough to start an infection in your throat, but the hair-like cilia found there are likely to do their job and clear the invaders. If the neighbour is closer and coughs 100 particles towards you, the virus might be able get all the way down to the lungs, says Xiao.
These varying capacities might explain why people with COVID-19 have such different experiences. The virus can start in the throat or nose, producing a cough and disrupting taste and smell, and then end there. Or it might work its way down to the lungs and debilitate that organ. How it gets down there, whether it moves cell by cell or somehow gets washed down, is not known, says Stanley Perlman, an immunologist at the University of Iowa in Iowa City who studies coronaviruses. - Clemens-Martin Wendtner, an infectious-disease physician at the Munich Clinic Schwabing in Germany, says it could be a problem with the immune system that lets the virus sneak down into the lungs. Most infected people create neutralizing antibodies that are tailored by the immune system to bind with the virus and block it from entering a cell. But some people seem unable to make them, says Wendtner. That might be why some recover after a week of mild symptoms, whereas others get hit with late-onset lung disease. But the virus can also bypass the throat cells and go straight down into the lungs. Then patients might get pneumonia without the usual mild symptoms such as a cough or low-grade fever that would otherwise come first, says Wendtner. Having these two infection points means that SARS-CoV-2 can mix the transmissibility of the common cold coronaviruses with the lethality of MERS-CoV and SARS-CoV. “It is an unfortunate and dangerous combination of this coronavirus strain,” he says.
- The virus’s ability to infect and actively reproduce in the upper respiratory tract was something of a surprise, given that its close genetic relative, SARS-CoV, lacks that ability. Last month, Wendtner published results8 of experiments in which his team was able to culture virus from the throats of nine people with COVID-19, showing that the virus is actively reproducing and infectious there. That explains a crucial difference between the close relatives. SARS-CoV-2 can shed viral particles from the throat into saliva even before symptoms start, and these can then pass easily from person to person. SARS-CoV was much less effective at making that jump, passing only when symptoms were full-blown, making it easier to contain.
These differences have led to some confusion about the lethality of SARS-CoV-2. Some experts and media reports describe it as less deadly than SARS-CoV because it kills about 1% of the people it infects, whereas SARS-CoV killed at roughly ten times that rate. But Perlman says that’s the wrong way to look at it. SARS-CoV-2 is much better at infecting people, but many of the infections don’t progress to the lungs. “Once it gets down in the lungs, it’s probably just as deadly,” he says. - What it does when it gets down to the lungs is similar in some respects to what respiratory viruses do, although much remains unknown. Like SARS-CoV and influenza, it infects and destroys the alveoli, the tiny sacs in the lungs that shuttle oxygen into the bloodstream. As the cellular barrier dividing these sacs from blood vessels break down, liquid from the vessels leaks in, blocking oxygen from getting to the blood. Other cells, including white blood cells, plug up the airway further. A robust immune response will clear all this out in some patients, but overreaction of the immune system can make the tissue damage worse. If the inflammation and tissue damage are too severe, the lungs never recover and the person dies or is left with scarred lungs, says Xiao. “From a pathological point of view, we don’t see a lot of uniqueness here.”
And as with SARS-CoV, MERS-CoV and animal coronaviruses, the damage doesn’t stop with the lungs. A SARS-CoV-2 infection can trigger an excessive immune response known as a cytokine storm, which can lead to multiple organ failure and death. The virus can also infect the intestines, the heart, the blood, sperm (as can MERS-CoV), the eye and possibly the brain. Damage to the kidney, liver and spleen observed in people with COVID-19 suggests that the virus can be carried in the blood and infect various organs or tissues, says Guan Wei-jie, a pulmonologist at the Guangzhou Institute of Respiratory Health at Guangzhou Medical University, China, an institution lauded for its role in combating SARS and COVID-19. The virus might be able to infect various organs or tissues wherever the blood supply reaches, says Guan.
But although genetic material from the virus is showing up in these various tissues, it is not yet clear whether the damage there is being done by the virus or by a cytokine storm, says Wendtner. “Autopsies are under way in our centre. More data will come soon,” he says. - SARS-CoV-2 is uniquely equipped for forcing entry into cells. Both SARS-CoV and SARS-CoV-2 bind with ACE2, but the receptor-binding domain of SARS-CoV-2 is a particularly snug fit. It is 10–20 times more likely to bind ACE2 than is SARS-CoV9. Wendtner says that SARS-CoV-2 is so good at infecting the upper respiratory tract that there might even be a second receptor that the virus could use to launch its attack.
- Scientists think that the involvement of furin could explain why SARS-CoV-2 is so good at jumping from cell to cell, person to person and possibly animal to human. Robert Garry, a virologist at Tulane University in New Orleans, Louisiana, estimates that it gives SARS-CoV-2 a 100–1,000 times greater chance than SARS-CoV of getting deep into the lungs. “When I saw SARS-CoV-2 had that cleavage site, I did not sleep very well that night,” he says.
The mystery is where the genetic instructions for this particular cleavage site came from. Although the virus probably gained them through recombination, this particular set-up has never been found in any other coronavirus in any species. Pinning down its origin might be the last piece in the puzzle that will determine which animal was the stepping stone that allowed the virus to reach humans. - Some researchers hope that the virus will weaken over time through a series of mutations that adapt it to persist in humans. By this logic, it would become less deadly and have more chances to spread. But researchers have not yet found any sign of such weakening, probably because of the virus’s efficient genetic repair mechanism. “The genome of COVID-19 virus is very stable, and I don’t see any change of pathogenicity that is caused by virus mutation,” says Guo Deyin, who researches coronaviruses at Sun Yat-sen University in Guangzhou.
Rambaut, too, doubts that the virus will become milder over time and spare its host. “It doesn’t work that way,” he says. As long as it can successfully infect new cells, reproduce and transmit to new ones, it doesn’t matter whether it harms the host, he says.
But others think there is a chance for a better outcome. It might give people antibodies that will offer at least partial protection, says Klaus Stöhr, who headed the World Health Organization’s SARS research and epidemiology division. Stöhr says that immunity will not be perfect — people who are reinfected will still develop minor symptoms, the way they do now from the common cold, and there will be rare examples of severe disease. But the virus’s proofreading mechanism means it will not mutate quickly, and people who were infected will retain robust protection, he says.
“By far the most likely scenario is that the virus will continue to spread and infect most of the world population in a relatively short period of time,” says Stöhr, meaning one to two years. “Afterwards, the virus will continue to spread in the human population, likely forever.” Like the four generally mild human coronaviruses, SARS-CoV-2 would then circulate constantly and cause mainly mild upper respiratory tract infections, says Stöhr. For that reason, he adds, vaccines won’t be necessary. - The OC43 coronavirus offers a model for where this pandemic might go. That virus also gives humans common colds, but genetic research from the University of Leuven in Belgium suggests that OC43 might have been a killer in the past11. That study indicates that OC43 spilled over to humans in around 1890 from cows, which got it from mice. The scientists suggest that OC43 was responsible for a pandemic that killed more than one million people worldwide in 1889–90 — an outbreak previously blamed on influenza. Today, OC43 continues to circulate widely and it might be that continual exposure to the virus keeps the great majority of people immune to it.
- Many scientists are reserving judgement on whether the tamer coronaviruses were once as virulent as SARS-CoV-2. People like to think that “the other coronaviruses were terrible and became mild”, says Perlman. “That’s an optimistic way to think about what’s going on now, but we don’t have evidence.”
“Mounting evidence suggests coronavirus is airborne — but health advice has not caught up” (08/07/2020)
[edit]Dyani Lewis, “Mounting evidence suggests coronavirus is airborne — but health advice has not caught up”, Nature, (08 July 2020; update 23 July 2020), 583, pp.510-513.


- On 6 July, Morawska and aerosol scientist Donald Milton at the University of Maryland, College Park, supported by an international group of 237 other clinicians, infectious-disease physicians, epidemiologists, engineers and aerosol scientists, published a commentary in the journal Clinical Infectious Diseases that urges the medical community and public-health authorities to acknowledge the potential for airborne transmission. They also call for preventive measures to reduce this type of risk.
The researchers are frustrated that key agencies, such as the World Health Organization (WHO), haven’t been heeding their advice in their public messages.
In response to the commentary, the WHO softened its position. At a 7 July press conference, Benedetta Allegranzi, technical leader of the WHO task force on infection control said: “We have to be open to this evidence and understand its implications regarding the modes of transmission, and also regarding the precautions that need to be taken.”
On 9 July, the WHO issued a scientific brief on viral transmission. It maintains that more research is needed “given the possible implications of such [a] route of transmission”, but acknowledges that short-range aerosol transmission cannot be ruled out in crowded, poorly ventilated spaces. (The WHO told Nature that it had been working on this brief for a month, and that it was not a result of the commentary.) - For months, the WHO had steadfastly pushed back against the idea that there is a significant threat of the coronavirus being transmitted by aerosols that can accumulate in poorly ventilated venues and be carried on air currents. The agency maintains that the virus is spread mainly by contaminated surfaces and by droplets bigger than aerosols that are generated by coughing, sneezing and talking. These are thought to travel relatively short distances and drop quickly from the air.
This type of guidance has hampered efforts that could prevent airborne transmission, such as measures that improve ventilation of indoor spaces and limits on indoor gatherings, say the researchers in the commentary: “We are concerned that the lack of recognition of the risk of airborne transmission of COVID-19 and the lack of clear recommendations on the control measures against the airborne virus will have significant consequences: people may think that they are fully protected by adhering to the current recommendations, but in fact, additional airborne interventions are needed for further reduction of infection risk.” - Since the 1930s, public-health researchers and officials have generally discounted the importance of aerosols — droplets less than 5 micrometres in diameter — in respiratory diseases such as influenza. Instead, the dominant view is that respiratory viruses are transmitted by the larger droplets, or through contact with droplets that fall on surfaces or are transferred by people’s hands. When SARS-CoV-2 emerged at the end of 2019, the assumption was that it spread in the same way as other respiratory viruses and that airborne transmission was not important.
The WHO is following the available evidence, and has moderated its earlier opposition to the idea that the virus might spread through aerosols, Allegranzi says. She says that although the WHO acknowledges that airborne transmission is plausible, current evidence falls short of proving the case. She adds that recommendations for physical distancing, quarantine and wearing masks in the community are likely to go some way towards controlling aerosol transmission if it is occurring. - When SARS-CoV-2 emerged, health officials recommended frequent hand washing and maintaining a physical distance to break droplet and contact transmission routes. And some researchers and clinicians say these approaches are enough. Contact-tracing data support those measures, says Kate Grabowski, an infectious-disease epidemiologist at Johns Hopkins University in Baltimore, Maryland. “The highest-risk contacts are those that are individuals you share a home with or that you’ve been in a confined space with for a substantial period of time, which would lead me to believe it’s probably driven mostly by droplet transmission,” she says, although she says that aerosol transmission might occur on rare occasions.
But other researchers say that case studies of large-scale clusters have shown the importance of airborne transmission. When the news media reported large numbers of people falling ill following indoor gatherings, that caused Kim Prather, an aerosol scientist at the University of California, San Diego, to begin questioning the adequacy of the social-distancing recommendations from the US Centers for Disease Control and Prevention (CDC), which call for people to stay 6 feet (1.8 metres) apart. The indoor spread suggested the virus was being transmitted in a different way from how health authorities had assumed. “For an atmospheric chemist, which I am, the only way you get there is you put it in the air and everybody breathes that air,” says Prather, who joined the commentary. “That is the smoking gun.” - Laboratory studies going back to the 1930s and 1940s concluded that droplets expelled through talking or coughing are larger than aerosols. These bigger droplets, more than 5 micrometres in diameter, drop out of the air quickly because they are too heavy to ride on light air currents.
But more-sensitive experiments are now painting a more complex picture that points to the importance of aerosols as a transmission route. A study published in May used laser-light scattering to detect droplets emitted by healthy volunteers when speaking. The authors calculated6 that for SARS-CoV-2, one minute of loud speaking generates upwards of 1,000 small, virus-laden aerosols 4 micrometres in diameter that remain airborne for at least 8 minutes. They conclude that “there is a substantial probability that normal speaking causes airborne virus transmission in confined environments”.
Another study7 published by Morawska and her colleagues as a preprint, which has not yet been peer reviewed, found that people infected with SARS-CoV-2 exhaled 1,000–100,000 copies per minute of viral RNA, a marker of the pathogen’s presence. Because the volunteers simply breathed out, the viral RNA was probably carried in aerosols rather than in the large droplets produced during coughing, sneezing or speaking. - One of the problems researchers face in studying virus viability in aerosols is the way that samples are collected. Typical devices that suck in air samples damage a virus’s delicate lipid envelope, says Julian Tang, a virologist at the University of Leicester, UK. “The lipid envelope will shear, and then we try and culture those viruses and get very, very low recovery,” he says.
- A few studies, however, have successfully measured the viability of aerosol-borne virus particles. A team at the US Department of Homeland Security Science and Technology Directorate in Washington DC found that environmental conditions play a big part in how long virus particles in aerosols remain viable. SARS-CoV-2 in mock saliva aerosols lost 90% of its viability in 6 minutes of exposure to summer sunlight, compared with 125 minutes in darkness10. This study suggests that indoor environments might be especially risky, because they lack ultraviolet light and because the virus can become more concentrated than it would be in outdoor spaces.
- Tang, who contributed to the commentary, says the bar of proof is too high regarding airborne transmission. “[The WHO] ask for proof to show it’s airborne, knowing that it’s very hard to get proof that it’s airborne,” he says. “In fact, the airborne-transmission evidence is so good now, it’s much better than contact or droplet evidence for which they’re saying wash [your] hands to everybody.”
Ultimately, says Morawska, strong action from the top is crucial. “Once the WHO says it’s airborne, then all the national bodies will follow,” she says. - Governments have started to move on their own to combat airborne transmission. In May, the guidance from the German department of health changed to state explicitly that “Studies indicate that the novel coronavirus can also be transmitted through aerosols … These droplet nuclei can remain suspended in the air over longer periods of time and may potentially transmit viruses. Rooms containing several people should therefore be ventilated regularly.” The CDC doesn’t mention aerosols or airborne transmission, but it updated its website on 16 June to say that the closeness of contact and the duration of exposure are important.
A spokesperson for the United Kingdom’s Scientific Advisory Group for Emergencies says there is weak evidence for aerosol transmission in some situations, but the group nonetheless recommends “that measures to control transmission include those that target aerosol routes”. When the United Kingdom reviewed its social-distancing guidelines, it advised people to take extra precautions in situations where it isn’t possible to stay 2 metres apart. The advice includes recommendations to wear a face mask and to avoid face-to-face interactions, poor ventilation and loud talking or singing. - This is not the first time during the pandemic that clinicians and researchers have criticized the WHO for being slow to update guidelines. Many had called on the agency early on to acknowledge that face masks can help to protect the general public. But the WHO did not make an announcement on this until 5 June, when it changed its stance and recommended the wearing of cloth masks when social distancing wasn’t possible, such as on public transport and in shops. Many countries were already recommending or mandating their use. On 3 April, the CDC issued recommendations to use masks in areas where transmission rates are high. And evidence backs up those actions: a systematic review found ten studies of COVID-19 and related coronaviruses — predominantly in health-care settings — that together show that face masks do reduce the risk of infection11.
Allegranzi acknowledges that, regarding the WHO’s position on masks, “the previous [advice] maybe was less clear or more cautious”. She says that emerging evidence that a person with SARS-CoV-2 is able to pass it on before symptoms have started (pre-symptomatic) or without ever showing symptoms (asymptomatic), factored into the decision to change the guidance. Other research — commissioned by the WHO — showing that cloth face masks are an effective barrier, was also an important factor.
“COVID-19 rarely spreads through surfaces. So why are we still deep cleaning?” (29/1/2021)
[edit]Dyani Lewis, “COVID-19 rarely spreads through surfaces. So why are we still deep cleaning?”, Nature, (29 January 2021), 590, pp.26-28

- The focus on fomites — rather than aerosols — emerged at the very beginning of the coronavirus outbreak because of what people knew about other infectious diseases. In hospitals, pathogens such as methicillin-resistant Staphylococcus aureus, respiratory syncytial virus and norovirus can cling to bed rails or hitch a ride from one person to the next on a doctor’s stethoscope. So as soon as people started falling ill from the coronavirus, researchers began swabbing hospital rooms and quarantine facilities for places the virus could be lurking. And it seemed to be everywhere.
In medical facilities, personal items such as reading glasses and water bottles tested positive for traces of viral RNA — the main way that researchers identify viral contamination. So, too, did bed rails and air vents. In quarantined households, wash basins and showers harboured the RNA, and in restaurants, wooden chopsticks were found to be contaminated. And early studies suggested that contamination could linger for weeks. Seventeen days after the Diamond Princess cruise ship was vacated, scientists found3 viral RNA on surfaces in cabins of the 712 passengers and crew members who tested positive for COVID-19.
But contamination with viral RNA is not necessarily cause for alarm, says Goldman. “The viral RNA is the equivalent of the corpse of the virus,” he says. “It’s not infectious.” - Human exposure studies of other pathogens provide additional clues about fomite transmission of respiratory viruses. In 1987, researchers at the University of Wisconsin— Madison put healthy volunteers in a room to play cards with people infected with a common-cold rhinovirus. When the healthy volunteers had their arms restrained to stop them touching their faces and prevent them transferring the virus from contaminated surfaces, half became infected. A similar number of volunteers who were unrestrained also became infected. In a separate experiment, cards and poker chips that had been handled and coughed on by sick volunteers were taken to a separate room, where healthy volunteers were instructed to play poker while rubbing their eyes and noses. The only possible mode of transmission was through the contaminated cards and chips; none became infected. The combination of experiments provided strong evidence that rhinoviruses spread through the air. But such studies are considered unethical for SARS-CoV-2, because it can kill.
- The WHO updated its guidance on 20 October, saying that the virus can spread “after infected people sneeze, cough on, or touch surfaces, or objects, such as tables, doorknobs and handrails”. A WHO spokesperson told Nature that “there is limited evidence of transmission through fomites. Nonetheless, fomite transmission is considered a possible mode of transmission, given consistent finding of environmental con tamination, with positive identification of SARS-CoV-2 RNA in the vicinity of people infected with SARS-CoV-2.” The WHO adds that “disinfection practices are important to reduce the potential for COVID-19 virus contamination”.
“Superspreading drives the COVID pandemic — and could help to tame it” (2/23/2021)
[edit]Dyani Lewis, “Superspreading drives the COVID pandemic — and could help to tame it”, Nature, (23 February 2021), 590, pp.544-546

- With a year’s worth of data, researchers have amassed ample evidence of some chief ingredients of superspreading events: prolonged indoor gatherings with poor ventilation. Activities such as singing and aerobic exercise, which produce many of the tiny infectious droplets that can be inhaled by others, are also common components.
But key questions remain. “We have some ideas of what factors are involved, but we still don’t know what is the main driver of the superspreading,” says Endo. Foremost are uncertainties about how much individual differences in people’s behaviour and biology matter — or can be controlled — and how best to target high-risk settings while keeping the cogs of society turning. Understanding the underlying factors that drive superspreading is crucial, says Lucy Li, an infectious-diseases modeller at the Chan Zuckerberg Biohub in San Francisco, California. - A team led by Bronwyn MacInnis, a geneticist at the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, traced the impact of superspreading events using viral genome sequences. One superspreading event — a two-day international business conference held in Boston in late February 2020 — seeded more than 90 cases in attendees and their close contacts. But the true impact was much greater, says MacInnis. She estimates that roughly 20,000 infections in Boston and its surrounding areas could be traced back to the conference.
- In all of the cases Prentiss and her team looked at, the person most likely to have infected others was either mildly symptomatic or hadn’t yet developed symptoms. This is a key similarity between the events and is probably shared by other occurrences of superspreading. “It’s transmission in young, healthy, mobile populations that actually does the most damage,” says MacInnis. “Just because you feel well doesn’t mean that you’re not infected and potentially spreading,” she says.
- Pay attention to personal hygiene. Yes, we know you’ve heard all this a million times already. It bears repeating. There are a lot of things we don’t know about this virus, but we do know it spreads through respiratory droplets produced when an infected person coughs or sneezes. Other individuals may be infected when they touch a surface that has virus particles on it and then touch their own mouth, nose, or eyes. Hand hygiene is the very best weapon in any fight between human and contagious disease.
- Don’t touch your face. This is a lot harder than it sounds and requires conscious effort. The average person touches their face 23 times an hour, and about half of the time, they’re touching their mouth, eyes, or nose — the mucosal surfaces that COVID-19 infects.
- Practice “social distancing.” Social distancing is exactly what it sounds like: keeping your distance from other people. It’s often used to describe public health measures imposed by local governments — measures like quarantining the sick, closing schools, and canceling public gatherings. And, when it’s done early enough during a pandemic illness, it’s been shown to save lives
“FAQ: COVID-19 (coronavirus disease 2019)”, “MIT.edu”.
[edit]- COVID-19 is the same type of coronavirus as MERS and SARs, both of which originated in bats. Many of the first people to contract COVID-19 in Wuhan either worked or frequently shopped at a large seafood and live-animal market, suggesting animal-to-person spread.
- February 29, 2020
- According to the Centers for Disease Control and Prevention (CDC) the virus is thought to spread mainly between people who are in close contact with each other (within 6 feet). The virus spreads through respiratory droplets produced when an infected person coughs, sneezes, or talks. These droplets can land in the mouths or noses of people who are nearby or may be inhaled into the lungs.
It may also be possible to get COVID-19 by touching a surface or object that has the virus on it and then touching your own mouth, nose, or eyes. However, scientists do not believe this is the main way the virus spreads. To minimize the possibility of contracting the virus in this way, the CDC recommends frequent hand-washing with soap and water or using an alcohol-based hand rub. The CDC also recommends routine cleaning of frequently touched surfaces.- April 7, 2020
- While we are still learning more about the virus, according to the Centers for Disease Control and Prevention (CDC), there is no evidence to support transmission of COVID-19 associated with food.
This is not surprising based on what we know about the varying paths organisms take to make people sick. Respiratory viruses, like COVID-19, typically attach to cells in places like the lungs and cannot survive the acidic environment of the digestive system. In contrast, the microorganisms that cause digestive illnesses, like norovirus and salmonella, survive the acid in stomachs and make people ill by attaching to the cells inside people’s guts.
In addition, any viral particles landing on food would not be expected to remain viable for long. Unlike bacteria, viruses cannot grow inside food, so any amount of virus in food would diminish over time, rather than grow.- April 7, 2020
- The individual who is self-quarantining must stay as separate as possible from other people sharing the living space. They should stay in their own bedroom and, if possible, use a bathroom that is not shared with others. If the self-quarantining individual needs to come out of their room for any reason, they should wash their hands and wear a mask. If there’s only one bathroom, set up a bathroom rotation in which the self-quarantining individual uses the bathroom last and then disinfects it thoroughly (read more about proper disinfection techniques).
Clean and disinfect commonly touched surfaces frequently. This includes countertops, doorknobs, light switches, and bathroom surfaces. Wash your hands frequently.
Do not share any items with the self-quarantining individual. This includes dishes, drinking glasses, silverware, towels, phones, and remote controls. If possible, use a dishwasher to clean and dry dishes and silverware used by the self-quarantining individual. If this is not possible, wash them by hand using detergent and warm water. Dry them thoroughly, using a separate dishtowel.- April 7, 2020
- [E]vidence indicates that people who are infected with 2019-nCoV may be at their most contagious in the 48–72 hours before symptoms are noticeable. In addition, it is now estimated that up to 25 percent of infected individuals remain asymptomatic and may unwittingly infect others. For that reason, the Centers for Disease Control and Prevention (CDC) is now recommending that individuals wear non-medical-grade, cloth face coverings in public settings where it may be difficult to maintain social distancing, such as grocery stores. If everyone wears masks, this might help prevent those who are unknowingly infected from spreading the illness.
- June 8, 2020
- A study in the New England Journal of Medicine reported that, in laboratory tests, the virus was detectable for up to 72 hours on plastic and stainless steel surfaces, up to 24 hours on cardboard, and up to four hours on copper. But a “detectable” amount of virus may not be enough to cause infection. In fact, most viral particles die relatively quickly outside of the body. Even on stainless steel and plastic, the half-life of the virus — the length of time it takes for half of the microbes in a given sample to die — was 5.6 and 6.8 hours respectively. On cardboard it was less than four hours.
- June 8, 2020
- The Centers for Disease Control and Prevention (CDC) is recommends that individuals wear non-medical-grade, cloth face coverings in public settings where it may be difficult to maintain social distancing, such as grocery stores. This recommendation is based on evidence that individuals may be at their most contagious in the 48–72 hours before symptoms are noticeable. In addition, it is now estimated that up to 25 percent of infected individuals remain asymptomatic and may unwittingly infect others. If everyone wears masks, this might help prevent those who are unknowingly infected from spreading the illness.
However, the CDC emphasizes, they are not recommending that individuals purchase surgical masks or N-95 respirators that are desperately needed for frontline healthcare workers. Rather, the CDC recommends making your own. You can sew a mask or use a 3D printer; the links below are a good place to start, but lots of other patterns and how-to videos are just a web search away. This video, for example, shows you how to create a no-sew face covering using a T-shirt or face towel and a couple of rubber bands or elastic hair ties.- June 8, 2020
- According to the Centers for Disease Control and Prevention (CDC), symptoms of COVID-19 include fever greater than 100.4°F (38.0°C), chills, dry cough, fatigue, shortness of breath or difficulty breathing, sudden loss of sense of smell or taste, nasal congestion, runny nose, sore throat, nausea or diarrhea, muscle or body aches, and headache. These symptoms typically begin gradually.
Not all affected individuals will exhibit all symptoms, and there is now evidence that up to 40 percent of infected individuals will have no symptoms at all.- August 20, 2020
- Taking into account your individual risk of complications from contracting the virus, such as age or underlying medical conditions, it may make sense to suspend house-cleaning services during the pandemic. However, recognizing that house-cleaners are often immigrants and low-wage workers, you may want to consider continuing to pay them if you can afford to do so.
If you do continue to use house-cleaning services, it’s important to take precautions that protect both you and the cleaners. Even though they are there to make your house clean, they could still transmit the virus to you, or you to them, if either of you were infected. Make sure your cleaners don a fresh pair of disposable gloves when they enter your home and change them often while they are working. Stay at least six feet away from your cleaners while they are in your home. Ask them not to come if they feel sick, or if you become ill. You might also think about trying to limit the amount of time they spend in your home each time they visit; perhaps more time-consuming cleaning jobs, like washing windows, can be done during a separate visit.- September 10, 2020
“Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics” (1/9/2020)
[edit]Eskild Petersen, Marion Koopmans, Unyeong Go, Davidson H Hamer, Nicola Petrosillo, Francesco Castelli, Merete Storgaard, Sulien Al Khalili, Lone Simonsen; “Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics”, The Lancet, (September 01, 2020), Volume 20, ISSUE 9, e238-e244,
- The new coronavirus SARS-CoV-2 is less deadly but far more transmissible than MERS-CoV or SARS-CoV. The virus emerged in December, 2019, and as of June 29, 2020, 6 months into the first pandemic wave, the global count is rapidly approaching 10 million known cases and has passed 500 000 deaths. Because of its broad clinical spectrum and high transmissibility, eradicating SARS-CoV-2, as was done with SARS-CoV in 2003, does not seem a realistic goal in the short term.
- The R0 for the SARS outbreak in 2003 was estimated to be between 2•0 and 3•0 in the early months (until the end of April), before public health control measures were introduced. Various control measures soon reduced the transmissibility to 1•1, with a wide IQR of 0•4–2•4. For MERS-CoV, the R0 (unmitigated) was estimated to be 0•69 (95% CI 0•50–0•92), consistent with MERS-CoV never having caused sustained epidemics. For SARS-CoV-2, a recent China joint mission by WHO concluded that “transmission of SARS-CoV-2 is mostly driven by clusters in close contacts, particularly family clusters, and less so by community transmission”. Since the statement was released, this conclusion has been challenged, although superspreading events continue to occur in the pandemic. Studies have estimated the R0 at 2•2 (95% CI 1•4–3•9) and 2•7 (2•5–2•9); therefore, an average R0 of 2•5 seems a reasonable estimate. By comparison, the initial R0 estimate for the 2009 influenza A H1N1 pandemic was 1•7, later estimated between 0•17 and 1•3 after mitigation was initiated. R0 for the 1918 influenza pandemic was estimated at around 2•0 in the first wave in July, 1918.
- A notable difference between SARS-CoV, SARS-CoV-2, and MERS-CoV are the kinetics of virus shedding. Whereas SARS-CoV and MERS-CoV have tropism for lower airways, with less virus present in the upper respiratory tract, this tropism is different in SARS-CoV-2. For SARS-CoV-2, the average viral load in a family cluster was 6•8 × 105 copies per upper respiratory tract swab during the first 5 days, and live virus isolates were obtained from swabs during the first week of illness. In a study from Hong Kong, high viral loads were found in the first samples obtained after admission to hospital. This finding was confirmed in a study from China, which found a high viral load at the onset of symptoms that declined in the following 5–6 days. This quick decline in the viral load makes isolation and quarantine of patients with SARS-CoV-2 and their contacts much more challenging and less effective, as it has to be done as soon as possible after illness onset in order to reduce transmission. By contrast, for SARS-CoV viral loads peaked at 6–11 days after symptom onset, allowing a full extra week to identify and isolate cases before transmission occurred. This difference would in part explain why SARS could be eradicated in 2003 compared with the trajectory seen in the SARS-CoV-2 pandemic.
“The coronavirus is here to stay — here’s what that means” (16//2/2021)
[edit]Nicky Phillips, “The coronavirus is here to stay — here’s what that means”, Nature, (16 February 2021), 590, pp.382-384
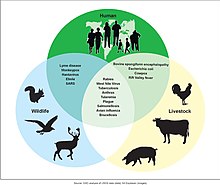
- In January, Nature asked more than 100 immunologists, infectious-disease researchers and virologists working on the coronavirus whether it could be eradicated. Almost 90% of respondents think that the coronavirus will become endemic — meaning that it will continue to circulate in pockets of the global population for years to come (see 'Endemic future').
- Five years from now, when childcare centres call parents to tell them that their child has a runny nose and a fever, the COVID-19 pandemic might seem a distant memory. But there’s a chance the virus that killed more than 1.5 million people in 2020 alone will be the culprit.
This is one scenario that scientists foresee for SARS-CoV-2. The virus sticks around, but once people develop some immunity to it — either through natural infection or vaccination — they won’t come down with severe symptoms. The virus would become a foe first encountered in early childhood, when it typically causes mild infection or none at all, says Jennie Lavine, an infectious-disease researcher at Emory University in Atlanta, Georgia.
Scientists consider this possible because that’s how the four endemic coronaviruses, called OC43, 229E, NL63 and HKU1, behave. At least three of these viruses have probably been circulating in human populations for hundreds of years; two of them are responsible for roughly 15% of respiratory infections. Using data from previous studies, Lavine and her colleagues developed a model that shows how most children first come down with these viruses before the age of 6 and develop immunity to them1. That defence wanes pretty quickly so it is not sufficient to block reinfection entirely, but it seems to protect adults from getting sick, says Lavine. Even in children, the first infection is relatively mild. - Because the virus has spread around the world, it might seem that it could already be classed as endemic. But because infections continue to increase worldwide, and with so many people still susceptible, scientists still technically class it as in a pandemic phase. In the endemic phase, the number of infections becomes relatively constant across years, allowing for occasional flare-ups, says Lavine.
To reach this steady state could take a few years or decades, depending on how quickly populations develop immunity, says Lavine. Allowing the virus to spread unchecked would be the fastest way to get to that point — but that would result in many millions of deaths. “That path has some huge costs,” she says. The most palatable path is through vaccination. - If vaccines do block transmission — and if they remain effective against newer variants of the virus — it might be possible to eliminate the virus in regions where enough people are vaccinated so that they can protect those who are not, contributing to herd immunity. A vaccine that is 90% effective at blocking transmission will need to reach at least 55% of the population to achieve temporary herd immunity as long as some social distancing measures — such as face masks and many people working from home — remain in place to keep transmission in check, according to a model3 developed by Alexandra Hogan at Imperial College London and her colleagues. (A vaccine would need to reach almost 67% of people to provide herd immunity if all social distancing measures were lifted.) But if the rate of transmission increases because of a new variant, or if a vaccine is less effective than 90% at blocking transmission, vaccine coverage will need to be greater to blunt circulation.
Vaccinating even 55% of the population will be challenging in many countries. “The virus will stick around if parts of the world don’t get vaccinated,” says Jeffrey Shaman, an infectious-disease researcher at Columbia University in New York City. - The 1918 influenza pandemic, which killed more than 50 million people, is the yardstick by which all other pandemics are measured. It was sparked by a type of virus known as influenza A, which originated in birds. Almost all cases of influenza A since then, and all subsequent flu pandemics, have been caused by descendants of the 1918 virus. These descendants circulate the globe, infecting millions of people each year. Flu pandemics occur when populations are naive to a virus; by the time a pandemic virus becomes seasonal, much of the population has some immunity to it. Seasonal flu still has a significant toll globally, claiming roughly 650,000 lives per year.
Jesse Bloom, an evolutionary biologist at the Fred Hutchinson Cancer Research Center in Seattle, thinks the coronavirus might follow a similar path. “I do think SARS-CoV-2 will become a less serious problem and something like flu,” he says. Shaman and others say the virus could also settle into a seasonal pattern of annual winter outbreaks similar to flu.
Flu seems to evolve much faster than SARS-CoV-2, allowing it to sneak past the immune system’s defences. This feature is why flu vaccines need to be reformulated each year; that might not be needed for SARS-CoV-2. - [T]he immune system has lots of tricks up its sleeve, and can respond to many features of the virus, not just spike, says Lavine. “The virus is probably going to have to go through lots of mutations to make a vaccine ineffective,” she says.
- More than 70% of the researchers surveyed by Nature think that immune escape will be another driver of the virus’s continuing circulation (see 'Driving factors'). This would not be a first for a human coronavirus. In a study yet to be peer reviewed, Bloom and his colleagues show that the endemic coronavirus 229E has evolved so that neutralizing antibodies in the blood of people infected with the viral variant circulating in the late 1980s and early 1990s are much less effective against more recent variants. People are reinfected with 229E over their lifetime, and Bloom suspects that it might be harder to stave off the variants that have evolved to escape previous immunity. But scientists don’t know whether these reinfections are associated with worse symptoms. “I would expect that over many years, accumulated mutations to SARS-CoV-2 will more completely erode neutralizing antibody immunity as we saw for CoV-229E, although I can’t say for sure how the rates will compare among the two coronaviruses,” says Bloom.
- Bloom thinks it’s probable that SARS-CoV-2 vaccines will need to be updated, possibly every year. But even then, immunity from either past vaccination or infection will probably blunt serious disease, he says. And Lavine notes that even if people are reinfected, this might not be a big deal. With the endemic coronaviruses, frequent reinfections seem to boost immunity against related variants and typically people experience only mild symptoms, she says. But it is possible that vaccines won’t stop some people developing severe symptoms, in which case the virus will continue to be a significant burden on society, says Shaman.
- The future of SARS-CoV-2 will also depend on whether it establishes itself in a wild animal population. Several diseases brought under control persist because animal reservoirs, such as insects, provide chances for pathogens to spill back into people. These include yellow fever, Ebola and chikungunya virus.
SARS-CoV-2 probably originated in bats, but it might have passed to people through an intermediate host. The virus can readily infect many animals, including cats, rabbits and hamsters. It is particularly infectious in mink, and mass outbreaks on mink farms in Denmark and the Netherlands have led to huge animal culls. The virus has also passed between minks and people. If it became established in a wild-animal population and could spill back into people, it would be very difficult to control, says Osterholm. “There is no disease in the history of humankind that has disappeared from the face of the Earth when zoonotic disease was such an important part of, or played a role in, the transmission,” he says.
“The sprint to solve coronavirus protein structures — and disarm them with drugs” (5/15/2020)
[edit]Megan Scudellari, “The sprint to solve coronavirus protein structures — and disarm them with drugs”, Nature 581, (15 May 2020; correction 19 May 2020), pp.252-255.


Meanwhile, on 10 February, just 12 days after harvesting the protein, McLellan and his group submitted its cryo-EM structure6 to the PDB. By studying the spike in detail, they found that it binds to its human cell receptor, a protein called ACE2, at least ten times more tightly than SARS-CoV does.
At the University of Minnesota in Saint Paul, Li’s team was on its way to working out why. On 11 February, Li and his colleagues began collecting X-ray data from the spike protein using the Advanced Photon Source (APS), the synchrotron facility at the US Department of Energy’s Argonne National Laboratory near Chicago, Illinois. By 13 February, the researchers had defined the small, important spot where the spike protein locks on to the ACE2 receptor7. They found that the new coronavirus spike protein has small molecular differences in its binding region compared with that of SARS-CoV, which might be why the new virus attaches to ACE2 more strongly. These changes could also explain why it seems to infect cells better and spreads faster than the SARS virus. That same week, the virus also got a name: SARS-CoV-2.
- Lying in bed on the night of 10 January, scrolling through news on his smartphone, Andrew Mesecar got an alert. He sat up. It was here. The complete genome of a coronavirus causing a cluster of pneumonia-like cases in Wuhan, China, had just been posted online.
Around the world, similar notifications appeared on the devices of scientists who first crossed swords with coronaviruses in the 2003 outbreak of SARS (severe acute respiratory syndrome) and then again with MERS (Middle East respiratory syndrome) in 2012. Instantly, the researchers mobilized against a new adversary. “We always knew that this was going to come back,” says Mesecar, head of biochemistry at Purdue University in West Lafayette, Indiana. “It’s what history has shown us.”
In Lübeck, Germany, Rolf Hilgenfeld stopped packing boxes for his retirement and started preparing buffers for crystallography. In Minnesota, Fang Li stayed up all night analysing the new genome and drafting a manuscript. In Shanghai, China, Haitao Yang rallied a dozen graduate students to clear their schedules. In Texas, Jason McLellan instructed laboratory members to start assembling gene sequences from the viral genome.
Within 24 hours, a network of structural biologists around the world had redirected their labs towards a single goal — solving the protein structures of a deadly, rapidly spreading new contagion. To do so, they would need to sift through the 29,811 RNA bases in the virus’s genome, seeking out the instructions for each of its estimated 25–29 proteins. With those instructions in hand, the scientists could recreate the proteins in the lab, visualize them and then, hopefully, identify drug compounds to block them or develop vaccines to incite the immune system against them. - To solve the 3D structure of a protein at high resolution, scientists first design a gene construct — a circle of DNA containing the instructions for the protein, together with regulatory sequences to control where and how it is expressed. They then insert the construct into living cells, often the bacterium Escherichia coli, using the cells’ own machinery to churn out the desired protein. Next, they purify the protein so that they can visualize its structure using either of two methods. One is X-ray crystallography, which involves growing tiny crystals of pure protein and revealing their internal structure by bombarding them with X-rays from a high-energy electron beam. The other is cryo-electron microscopy (cryo-EM), a process of scanning flash-frozen proteins using a high-powered electron microscope.
Either process can take months, even years, for an unfamiliar protein. Luckily, many of the new coronavirus proteins were familiar, with 70–80% sequence similarity to SARS-CoV, the virus that caused the 2003 SARS outbreak. By 7:30 a.m., Mesecar and his team had begun designing gene constructs for the new viral proteins, and even predicted which of their existing coronavirus inhibitors might block these proteins. - In McLellan’s molecular biosciences lab at the University of Texas at Austin, graduate student Daniel Wrapp spent the weekend designing a gene construct for another key protein — the outer, three-pronged spike that gives the coronavirus its crown-like appearance and name (see ‘The key coronavirus proteins’). Wrapp placed an order for the constructs with a commercial firm that Monday, 13 January.
McLellan had been involved in determining the structures of two other coronavirus spikes — from HKU1, a cause of common colds1, and from the MERS virus2. The work was done in collaboration with structural biologist Andrew Ward at the Scripps Research Institute in La Jolla, California, and virologist Barney Graham at the US National Institute of Allergy and Infectious Diseases’ Vaccine Research Center in Bethesda, Maryland. So, the group knew how to tweak the spike protein’s genetic sequence so that it would stabilize in a pre-fusion shape — the form it adopts before it docks onto a host cell. “Our ability to get this particular structure was based upon all our prior knowledge from working on HKU1 and MERS and SARS,” says McLellan.
Mpro in coronaviruses is made up of two identical subunits and looks like a moth-eaten heart, with an active enzyme site on each side of the structure. On 26 January, Rao and Yang submitted the Mpro structural data to the Protein Data Bank (PDB), an open-access digital resource for 3D structures of biological molecules. By 5 February, the data had been processed and the final structure was released online — not a moment too soon, says Yang. The laboratory had already received an overwhelming 300 requests for the structure. - In Hilgenfeld’s lab at the University of Lübeck, researcher Linlin Zhang had taken to phoning the company making the Mpro gene construct daily until it finally arrived. Thanks to the lab’s experience crystallizing other coronavirus proteases, Zhang grew Mpro crystals in 10 days, and on 1 February, she took the precious samples to the BESSY II synchrotron in Berlin, which opened up a beamline especially for the project.
In addition to focusing on the unbound Mpro structure, Hilgenfeld docked a small-molecule inhibitor called 13a, which he had designed to inhibit the MERS virus, into the protein’s active site. It wasn’t a perfect fit, so the team altered a residue on the compound and named it 13b. This one “fit nicely”, says Hilgenfeld, and in ten more days his team had solved the structure of Mpro bound to the inhibitor4. - Vaccines are often based on presenting parts of a virus to the human immune system to provoke a response, and the spike protein is an obvious candidate because it has a crucial role in infection.
The spike is formed of three identical molecules stuck together in the shape of a pyramid, with a hinge-like trapdoor. This opens to expose a portion that grabs onto a receptor on a human cell (see ‘The spike locks on’). Graham and McLellan’s past work on a similar protein5 suggested that presenting the spike protein in its pre-grab state would provoke the human immune system. From the complete structure, Graham could see that McLellan’s gene construct made a high-quality protein arranged in the right conformation. “It was really, really important to have that electron-microscopy information,” says Graham. - Graham tested the spike protein in mice, working to improve its expression levels and the strength of its effect on the immune system, and sent the sequence to Moderna, where the production line was ready and waiting. On 7 February, Moderna completed its first batch of the vaccine based on that protein.
Meanwhile, on 10 February, just 12 days after harvesting the protein, McLellan and his group submitted its cryo-EM structure6 to the PDB. By studying the spike in detail, they found that it binds to its human cell receptor, a protein called ACE2, at least ten times more tightly than SARS-CoV does.
At the University of Minnesota in Saint Paul, Li’s team was on its way to working out why. On 11 February, Li and his colleagues began collecting X-ray data from the spike protein using the Advanced Photon Source (APS), the synchrotron facility at the US Department of Energy’s Argonne National Laboratory near Chicago, Illinois. By 13 February, the researchers had defined the small, important spot where the spike protein locks on to the ACE2 receptor7. They found that the new coronavirus spike protein has small molecular differences in its binding region compared with that of SARS-CoV, which might be why the new virus attaches to ACE2 more strongly. These changes could also explain why it seems to infect cells better and spreads faster than the SARS virus. That same week, the virus also got a name: SARS-CoV-2. - So far, the CSGID consortium has solved 12 unique SARS-CoV-2 protein structures, which are kept in a new online database with their accompanying genomic information. “We’ve been part of projects like this on cancer, but it took five years to set that all up,” says Adam Godzik, a bioinformatician at the University of California, Riverside, and a CSGID investigator. “This happened spontaneously in the course of months.”
- With 3D structures in hand, structural-biology teams moved straight to next steps. “Structures aren’t everything,” says Mesecar. “You want to get to compounds — to antivirals and vaccines.”
On 16 March, just 65 days after the viral genome was released, clinicians gave the first dose of Moderna’s vaccine candidate to a patient in a clinical trial funded by the US National Institutes of Health.
“It was a lot faster than even the fastest one we’d previously done,” says Graham. Because of research on SARS and MERS, coronaviruses were probably the only viral family for which that was possible, he adds. “If it was a bunyavirus or an arenavirus, we would have been lost for two to three years.”
But even a vaccine developed at record-breaking speed is likely to be a slower solution than repurposing an approved drug, or at least finding one for which safety testing has begun. “That’s absolutely going to be the fastest way to help patients sick in the hospital today,” says Satchell. - On 10 April, Rao, Yang and their collaborators published8 the structure of the virus’s replication complex — a large protein called RNA-dependent RNA polymerase (RdRp, or nsp12) that forms a complex with two others, nsp7 and nsp8. They also modelled how it binds to the antiviral drug remdesivir, originally developed to treat Ebola and now in phase III trials for coronavirus. Another recently completed structure of the protein in complex with the drug9 could provide a template to help model and modify other existing antivirals.
- Structural biologists continue to plug away at the remaining unsolved proteins in the coronavirus genome. These include ORF8, a protein whose function remains mysterious. “We predict it should be crystallizable, but nobody has done it, so we’re trying,” says Godzik.
In the United Kingdom, the Diamond team is screening various compounds against a second coronavirus protease. In Texas, McLellan has shipped spike constructs to more than 100 labs worldwide. Many are looking for treatments, using the protein to fish antibodies out of the blood of people who have had COVID-19, and McLellan’s team is now characterizing the first of these potentially therapeutic antibodies.
Hilgenfeld, who was officially scheduled to retire on 1 April as a result of a mandatory retirement policy, has packed up his office but continues to work. “I’ve been working on coronaviruses for 20 years, and most of the time it was neglected and not taken seriously,” he says. “Now that it’s happened, how can I leave?” His team is investigating other SARS-CoV-2 structures, including nsp3, a large protein that the virus uses to shut down host-cell defences.
The race against the virus can’t afford to slow down anytime soon. As soon as countries start lifting restrictions on people’s movement, the virus will return and “flip around the world again”, says Satchell. “When that happens, it would be really great to have beautiful drugs that were designed specifically to target this coronavirus,” she says. “But we need to do it fast.”
Virus-infected patients
[edit]- Danny Altmann, professor of immunology at Imperial faculty in London, guesses that those that recuperate from Covid-19 can have maybe 90% safety for a “fair while”. But how lengthy is that? “I would bet my house on you being safe for possibly a year but not much longer,” he mentioned. “The problem is that whenever an immunologist says anything about Covid immunity to a journalist, it’s right for about two weeks and then it’s completely wrong.”
- Danny Altman as quoted in "Flurry of coronavirus reinfections leaves scientists puzzled", “Pehal News Team”, (Oct. 7, 2020)
- Fatality rate of the 2019-CoV infection is relatively low, at slightly more than three percent, suggesting the possibility that those who died could have other predispositions. Most (of the patients) would fully recover.
- Sazaly Abu Bakar (2020) cited in "'Most coronavirus patients will recover'" on New Straits Times, 28 January 2020.
- Monoclonal antibodies are lab-made drugs meant to mimic natural antibodies to SARS-CoV-2, the virus that causes Covid-19. They're recommended for people who are at high risk of getting very sick from the virus, including anyone over age 65 and people with underlying health conditions.
At least one study showed that the therapy can lower the amount of virus in a person's system. But no gold standard research proves that monoclonal antibodies do, indeed, provide this benefit. Most reports are anecdotal.- Erika Edwards, ”Monoclonal antibodies could ease record Covid hospitalizations. Why are they going unused?”, (Jan 15, 2021)
- Monoclonal antibodies must be given soon after a person has tested positive. "These medications work best when given early," Surgeon General Jerome Adams said during Thursday's briefing.
The two monoclonal antibody products that have been authorized for emergency use by the FDA, from the drugmakers Eli Lilly and Regeneron, must be given within the first week of illness.- Erika Edwards, ”Monoclonal antibodies could ease record Covid hospitalizations. Why are they going unused?”, (Jan 15, 2021)
- In all the history of respiratory-borne viruses of any type, asymptomatic transmission has never been the driver of outbreaks. … Even if there’s a rare asymptomatic person that might transmit, an epidemic is not driven by asymptomatic carriers.
- Anthony Fauci, “Update on the New Coronavirus Outbreak First Identified in Wuhan, China | January 28, 2020”, U.S. Department of Health and Human Services, (Jan. 28, 2020)
- According to the United Nations, about 1 billion persons live in so-called slums. Numerous studies have shown that this population is particularly vulnerable to infectious diseases. The current COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, emphatically underlines this problem. The often high-density living quarters coupled with a large number of persons per dwelling and the lack of adequate sanitation are reasons why measures to contain the pandemic only work to a limited extent in slums. Furthermore, assignment to risk groups for severe courses of COVID-19 caused by noncommunicable diseases (eg, cardiovascular diseases) is not possible due to inadequate data availability. Information on people living in slums and their health status is either unavailable or only exists for specific regions (eg, Nairobi). We argue that one of the greatest problems with regard to the COVID-19 pandemic in the context of slums in the Global South is the lack of data on the number of people, their living conditions, and their health status.
- John Friesen, Peter F Pelz, “COVID-19 and Slums: A Pandemic Highlights Gaps in Knowledge About Urban Poverty”, JMIR Public Health Surveill. 2020 Jul-Sep; 6(3)
- The baseline assumptions for the model were that peak infectiousness occurred at themedian of symptom onset and that 30% of individuals with infection never develop symptoms andare 75% as infectious as those who do develop symptoms. Combined, these baseline assumptionsimply that persons with infection who never develop symptoms may account for approximately 24%of all transmission. In this base case, 59% of all transmission came from asymptomatic transmission,comprising 35% from presymptomatic individuals and 24% from individuals who never developsymptoms. Under a broad range of values for each of these assumptions, at least 50% of new SARS-CoV-2 infections was estimated to have originated from exposure to individuals with infection butwithout symptoms.
- Michael A. Johansson, PhD1,2; Talia M. Quandelacy, PhD, MPH1; Sarah Kada, PhD1; et al Pragati Venkata Prasad, MPH1; Molly Steele, PhD, MPH1; John T. Brooks, MD1; Rachel B. Slayton, PhD, MPH1,2; Matthew Biggerstaff, ScD, MPH1,2; Jay C. Butler; “SARS-CoV-2 Transmission From People Without COVID-19 Symptoms”, JAMA Netw Open. (January 7, 2021);4(1):e2035057.
- SARS-CoV-2, the virus that causes coronavirus disease 2019 (COVID-19), is transmitted predominantly by respiratory droplets generated when infected persons cough, sneeze, spit, sing, talk, or breathe. CDC recommends community use of face masks to prevent transmission of SARS-CoV-2. As of October 22, 2020, statewide mask mandates were in effect in 33 states and the District of Columbia. This study examined whether implementation of statewide mask mandates was associated with COVID-19–associated hospitalization growth rates among different age groups in 10 sites participating in the COVID-19–Associated Hospitalization Surveillance Network (COVID-NET) in states that issued statewide mask mandates during March 1–October 17, 2020. Regression analysis demonstrated that weekly hospitalization growth rates declined by 2.9 percentage points (95% confidence interval [CI] = 0.3–5.5) among adults aged 40–64 years during the first 2 weeks after implementing statewide mask mandates. After mask mandates had been implemented for ≥3 weeks, hospitalization growth rates declined by start highlight5.6end highlight percentage points among persons aged 18–39 years (95% CI = start highlight0.9end highlight–10.4) and those aged 40–64 years (95% CI = start highlight1.0end highlight–10.2). Statewide mask mandates might be associated with reductions in SARS-CoV-2 transmission and might contribute to reductions in COVID-19 hospitalization growth rates, compared with growth rates during <4 weeks before implementation of the mandate and the implementation week. Mask-wearing is a component of a multipronged strategy to decrease exposure to and transmission of SARS-CoV-2 and reduce strain on the health care system, with likely direct effects on COVID-19 morbidity and associated mortality.
- Heesoo Joo; Gabrielle F. Miller; Gregory Sunshine; Maxim Gakh; Jamison Pike; Fiona P. Havers; Lindsay Kim; Regen Weber; Sebnem Dugmeoglu; Christina Watson; Fátima Coronado; Decline in COVID-19 Hospitalization Growth Rates Associated with Statewide Mask Mandates — 10 States, March–October 2020”, CDC, (Feb 12, 2021)
- Katonah rejected the idea that we can add those who have already been infected with COVID-19 to vaccinated people to reach the 70%-80% level of coverage needed for herd immunity.
"First, there's an overlap: some people who were infected later got vaccinated. The second issue is that once you're infected, your immunity goes away fairly fast. So you don't just count the people who are infected, but the people who were recently infected," he said. He estimated that natural immunity might not last longer than 3 months.- Peter Katonah as quoted in “What Experts Predict From COVID This Fall and Winter”, by Ken Terry, WebMD, (May 20, 2021)
- To our knowledge, this study is the first to report an association between detailed sleep habits (sleep hours at night, daytime napping hours, severe sleep problems) and COVID-19 in multiple countries. It has been speculated that insufficient sleep may play an important role in COVID-19. One prior study found that self-reported lack of sleep was associated with higher odds whereas 1-hour longer daily sleep time was associated with lower odds of ≥20 days of hospital stay due to COVID-19. Our results on sleep hours at night are in agreement with this previous study, but we contribute to the literature by providing more comprehensive information on sleep habits. Several prior studies have already shown that short sleep duration prior to virus exposure is prospectively associated with a greater risk of acute infectious diseases, such as pneumonia and common cold. Similarly, self-reported sleep disorder has been associated with greater odds of head or chest cold. The mechanism underlying these associations remains unclear, but it has been hypothesized that lack of sleep and sleep disorders may adversely influence the immune system by increasing proinflammatory cytokines and histamines. However, it is important to note that our study used self-reported sleep duration and self-reported sleep disorders, and the association between daytime napping and COVID-19 attenuated when we restricted COVID-19 cases to a positive PCR or antibody test. Future studies are needed to confirm whether these associations persist with objective measures of sleep.
- Hyunju Kim, Sheila Hegde, Christine LaFiura, Madhunika Raghavan, Eric Luong, Susan Cheng, Casey M Rebholz, Sara B Seidelmann. “COVID-19 illness in relation to sleep and burnout.” BMJ Nutrition, Prevention & Health, 2021; bmjnph-2021-000228 DOI: 10.1136/bmjnph-2021-000228
- Our findings raise the possibility that the nature of an individual’s antibody response to prior endemic CoV infection may affect the course of COVID-19. They also indicate that analysis of S2 reactivity is crucial for a complete assessment of the humoral response to SARS-CoV-2, consistent with the observation that S2-only assays provide an equally strong correlate of neutralization compared to RBD-only assays (J. Nikolich and D. Bhattacharya, personal communication). The HR2 and FP cross-reactivities characterized here represent a possible source of background signal for SARS-CoV-2 serological assays that include the S2 subunit of Spike, which would be absent in those targeting only the RBD, for which sequence conservation is lower across CoV species. However, our findings also indicate that the incorporation of related endemic CoV antigens may improve the sensitivity of SARS-CoV-2 serological analyses, and in particular, that a differential analysis of SARS-CoV-2 and endemic CoV Spike S2 reactivity may provide an important measure of the efficiency with which preexisting cross-reactive responses can be redirected.
The identification of broadly immunogenic epitopes in conserved functional domains of the SARS-CoV-2 Spike S2 subunit, including cross-reactivity with endemic HCoVs, also has implications for the design of therapeutic antibodies and vaccines. SARS-CoV-2 vaccines under development predominantly use two forms of the S antigen—whole protein or the RBD—and in each case are designed primarily to elicit neutralizing antibodies. Relative to RBD-focused vaccines, we hypothesize that vaccines that include the Spike HR2 and FP sites (1) will be able to induce a broader array of neutralizing reactivities, (2) may be more capable of rapidly recruiting preexisting memory B cells that are prevalent in the population, and (3) may be less prone to viral escape due to a lower tolerance for amino acid substitutions. In particular, the identification of HR2 and FP as conserved, functionally important and broadly immunogenic sites capable of eliciting cross-reacting antibodies, makes these regions candidates for the development of broadly neutralizing responses against CoVs. Future work should resolve the functional consequences of these cross-reactive antibody responses, and how an individual’s exposure history to endemic CoVs may affect their course of COVID-19.- Jason T. Ladner, Sierra N. Henson, Annalee S. Boyle, Anna L. Engelbrektson, Zane W. Fink, Fatima Rahee, Jonathan D’ambrozio, Kurt E. Schaecher, Mars Stone, Wenjuan Dong, Sanjeet Dadwal, Jianhua Yu, Michael A. Caligiuri, Piotr Cieplak, Magnar Bjørås, Mona H. Fenstad, Svein A. Nordbø, Denis E. Kainov, Norihito Muranaka, Mark S. Chee, Sergey A. Shiryaev, John A. Altin; “Epitope-resolved profiling of the SARS-CoV-2 antibody response identifies cross-reactivity with endemic human coronaviruses”. Cell Reports Medicine, 2021; 2 (1): 100189 DOI: 10.1016/j.xcrm.2020.100189
- We need to get a better idea of how many people are discharged from hospital and a better understanding of how many mild cases have been missed (from this COVID-19), while we focused on more severe disease (until this moment (3 February 2020)). When we find that out will depend on China giving us more details, because that's where most cases are, and so far, a decent number of cases outside of China have not seemed as severe.
- Ian Mackay (2020) cited in: "Can the Wuhan Coronavirus Be Stopped?" in TheStreet, 3 February 2020.
- The risk of severe illness or death from COVID-19 increases steadily with age. Eight out of 10 COVID-19 deaths reported in the United States have been among individuals aged 65 years and older. Certain underlying medical conditions also increase your risk for severe illness. These include type 2 diabetes, serious heart conditions, sickle cell disease, COPD (chronic obstructive pulmonary disease), chronic kidney disease, immune deficiency, and obesity, defined as a body mass index (BMI) of 30 or higher. Other medical conditions, such as asthma, smoking, and pregnancy, may also increase an individual’s risk of severe COVID-19 illness.
- MIT.edu, “FAQ: COVID-19 (coronavirus disease 2019)”, (September 8, 2020)
- But even with similar viral loads, it’s not a foregone conclusion that vaccinated people are necessarily as contagious as unvaccinated people.
“This is intriguing data, it’s important, but I’m not positive that you’re equally as infectious if you’re vaccinated,” said Dr. Monica Gandhi, an infectious disease specialist at University of California, San Francisco, who was not involved in the research.
Gandhi said there are multiple parts to the immune system – including antibodies and T cells – that raise important questions around using viral load, which is measured by PCR tests, as a proxy for how contagious someone is.- Michael Nedelman, ”CDC shares ‘pivotal discovery’ on Covid-19 breakthrough infections that led to new mask guidance”, “CNN”, (Updated 2:01 PM EDT, Fri July 30, 2021)
- "Imbalance in the microbiome contributes to the severity of COVID-19, and if it persists after viral clearance, could contribute to persistent symptoms and multi-system inflammation syndromes like long COVID syndrome," said lead researcher Dr. Siew Ng, a professor from the Institute of Digestive Dis-ease at the Chinese University of Hong Kong.
"Restoration of the missing beneficial bacteria might boost our immunity against SARS-CoV2 virus and hasten recovery from the disease," she said. "Managing COVID-19 should not only aim at clearing the virus, but also restoring the gut microbiota."- Siew Ng as quoted in U.S. News A World Report, ”People's 'Microbiomes' Might Influence COVID-19 Severity: Study”, (Jan. 13, 2021)
- Sixty-one eligible studies and reports were identified, of which 43 used polymerase chain reaction (PCR) testing of nasopharyngeal swabs to detect current SARS-CoV-2 infection and 18 used antibody testing to detect current or prior infection. In the 14 studies with longitudinal data that reported information on the evolution of symptomatic status, nearly three quarters of persons who tested positive but had no symptoms at the time of testing remained asymptomatic. The highest-quality evidence comes from nationwide, representative serosurveys of England (n = 365 104) and Spain (n = 61 075), which suggest that at least one third of SARS-CoV-2 infections are asymptomatic.
- Daniel P. Oran, Eric J. Topol; “The Proportion of SARS-CoV-2 Infections That Are Asymptomatic”, Annals of Internal Medicine, (22 January 2021)
- Perhaps because of this broad spectrum of presentation, the topic of asymptomatic SARS-CoV-2 infection has generated some controversy. Imprecise use of the term “asymptomatic” is partly to blame. “Asymptomatic” should be reserved for persons who never develop symptoms, whereas “presymptomatic” is a better description of those who have no symptoms when they receive a positive test result but who eventually develop symptoms. We know for certain who is asymptomatic only in retrospect. On the basis of our current knowledge of the natural history of coronavirus disease 2019 (COVID-19), after a person is infected with SARS-CoV-2, we must wait approximately 14 days to determine whether symptoms have developed. Infection without symptoms, whether presymptomatic or asymptomatic, is important because infected persons can transmit the virus to others even if they have no symptoms.
- Daniel P. Oran, Eric J. Topol; “The Proportion of SARS-CoV-2 Infections That Are Asymptomatic”, Annals of Internal Medicine, (22 January 2021)
- Current data suggest that infected persons without symptoms—including both presymptomatic and asymptomatic persons—account for more than 40% of all SARS-CoV-2 transmission. The proportion of new infections caused by asymptomatic persons alone is uncertain, but when researchers in Wanzhou, China, analyzed epidemiologic data for “183 confirmed COVID-19 cases and their close contacts from five generations of transmission,” they determined that the asymptomatic cases, which made up 32.8% of infected persons, caused 19.3% of infections.
The 61 studies and reports that we have collected provide compelling evidence that the asymptomatic fraction of SARS-CoV-2 infection is sizable.- Daniel P. Oran, Eric J. Topol; “The Proportion of SARS-CoV-2 Infections That Are Asymptomatic”, Annals of Internal Medicine, (22 January 2021)
- This (COVID-19) virus is different from SARS-CoV, which caused severe illness in most infected patients. It appears that many patients have relatively mild illness. These relatively mild cases may recover after one week or so.
- Hitoshi Oshitani (2020) cited in "China’s health officials say priority is to stop mild coronavirus cases from getting worse" on South China Morning Post, (4 February 2020).
- RESULTS In 405 hospitals in 30 countries 11,266 adults were randomized, with 2750 allocated Remdesivir, 954 Hydroxychloroquine, 1411 Lopinavir, 651 Interferon plus Lopinavir, 1412 only Interferon, and 4088 no study drug. Compliance was 94-96% midway through treatment, with 2-6% crossover. 1253 deaths were reported (at median day 8, IQR 4-14). Kaplan-Meier 28-day mortality was 12% (39% if already ventilated at randomization, 10% otherwise). Death rate ratios (with 95% CIs and numbers dead/randomized, each drug vs its control) were: Remdesivir RR=0.95 (0.81-1.11, p=0.50; 301/2743 active vs 303/2708 control), Hydroxychloroquine RR=1.19 (0.89-1.59, p=0.23; 104/947 vs 84/906), Lopinavir RR=1.00 (0.79-1.25, p=0.97; 148/1399 vs 146/1372) and Interferon RR=1.16 (0.96-1.39, p=0.11; 243/2050 vs 216/2050). No study drug definitely reduced mortality (in unventilated patients or any other subgroup of entry characteristics), initiation of ventilation or hospitalisation duration.
CONCLUSIONS These Remdesivir, Hydroxychloroquine, Lopinavir and Interferon regimens appeared to have little or no effect on hospitalized COVID-19, as indicated by overall mortality, initiation of ventilation and duration of hospital stay. The mortality findings contain most of the randomized evidence on Remdesivir and Interferon, and are consistent with meta-analyses of mortality in all major trials.- H. Pan et al. Repurposed antiviral drugs for COVID-19; interim WHO SOLIDARITY trial results. medRxiv.org. October 15, 2020. doi: 10.1101/2020.10.15.20209817
- The primary hypothesized mechanism of benefit from convalescent plasma is through direct antiviral action of neutralizing antibodies on SARS-CoV-2 RNA.1 In the PLACID Trial, a statistically significant 20% higher rate of conversion to a negative result for SARS-CoV-2 RNA occurred on day 7 among patients in the intervention arm.
In plain English, this means that convalescent plasma did exactly what the investigators hoped it would do, yet there was no net clinical benefit to patients. Why might this be the case?
The most common use of therapeutic plasma, which contains more than 1000 different proteins, is for the management of acute bleeding and complex coagulopathies. Despite the presence in plasma of anticoagulation factors such as antithrombin and protein C, the net effect of plasma is prothrombotic. Immunoglobulin therapy, which is derived from whole plasma, is subject to a US Food and Drug Administration warning about the risks of thrombosis, particularly in older patients, those with cardiovascular risk factors, and those with hypercoagulable conditions.
It is now widely recognized that covid-19 is a life threatening thrombotic disorder. An excellent recent pathophysiology synthesis concluded that “SARS-CoV-2 not only produces an inflammatory and hypercoagulable state, but also a hypofibrinolytic state not seen with most other types of coagulopathy.” Most recently, plasma from convalescent covid-19 patients has been shown to directly cause endothelial cell damage in vitro.- Elizabeth B Pathak, “Convalescent plasma is ineffective for covid-19”, BMJ, 2020;371:m4072
- To affirm a reinfection, scientists should study the genetic code of the virus from every spherical of sickness and show they’re distinct. That means gaining access to each units of swabs and the wherewithal to do entire genome sequencing. Even in hospitals the place the capability exists, such checks are not often accomplished. Reinfected sufferers merely go unnoticed or unreported. “There is probably a lot more than we are seeing,” mentioned Iwasaki.
The immune system’s battle towards coronavirus is unleashed in a number of waves. The first line of defence, the innate immune system, is imprecise however quick. Invading pathogens immediate cells to churn out signalling proteins known as cytokines which name in a military of white blood cells that engulf and disrupt the virus.
Next to gear up is the adaptive immune system, a extra specialised attacking drive. This unleashes T-cells, which destroy contaminated cells, and prompts B-cells to make antibodies that stick with viruses and cease them spreading additional. If and when an infection is crushed, the T- and B-cells stand down, however some needs to be saved within the physique for years, an immune reminiscence that may be recommissioned ought to the virus attempt once more.
Given the complexity of the immune response, it’s no shock that scientists are struggling to unravel why reinfections happen. Blood checks on sufferers reveal that virus-disabling antibodies can wane after a number of months, notably in these with gentle or no signs. But even with wholesome ranges of antibodies, reinfection cannot solely occur, however trigger extra severe illness.- “Pehal News Team”, "Flurry of coronavirus reinfections leaves scientists puzzled", (Oct. 7, 2020)
- Despite the lack of accurate data on how physical activity improves the immune response against the new coronavirus, there is evidence of lower rates of ARI incidence, duration and intensity of symptoms and risk of mortality from infectious respiratory diseases in individuals who exercise at high levels appropriate.
- Matheus Pelinski da Silveira, Kimberly Kamila da Silva Fagundes, Matheus Ribeiro Bizuti, Édina Starck,1 Renata Calciolari Rossi,2 and Débora Tavares de Resende e Silva , “Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature”, Clin Exp Med. 2020 Jul 29 : 1–14.
- There are still gaps in the knowledge regarding the pathogenic mechanisms involved in SARS-CoV-2 infection. However, there is consensus in the scientific literature about the important involvement of the immune system in the susceptibility, progression and outcome of COVID-19. The imbalance in innate and adaptive immune responses, characterized mainly by changes such as cytokine storm and lymphopenia, in addition to the disorders in coagulation- and host-related conditions, including obesity, metabolic syndrome and aging (immunosenescence), is among the factors notoriously associated with a worse prognosis of infection.
The benefits of exercise—regular and at appropriate intensity levels—for the immune system in respiratory infections such as COVID-19 include increased immunovigilance and improved immune competence, which help in the control of pathogens, a fact that becomes more important considering the immunosenescence and susceptibility of the elderly population to severe infection. Other favorable effects in relation to host factors, such as prevention or reduction of overweight, increased physical and cardiopulmonary conditioning, attenuation of the systemic pro-inflammatory and pro-thrombotic states, decrease in oxidative stress, improvements in glycemic, insulinic and lipidic metabolisms, besides the enhancement of the vaccination response, also indicate how adequately physical activity can help the organism’s immune response against COVID-19.- Matheus Pelinski da Silveira, Kimberly Kamila da Silva Fagundes, Matheus Ribeiro Bizuti, Édina Starck, Renata Calciolari Rossi, and Débora Tavares de Resende e Silva, “Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature”, Clin Exp Med. 2020 Jul 29 : 1–14.
- SARS-CoV-2 causes mild or asymptomatic disease in most cases; however, severe to critical illness occurs in a small proportion of infected individuals, with the highest rate seen in people older than 70 years. The measured case fatality rate varies between countries, probably because of differences in testing strategies. Population-based mortality estimates vary widely across Europe, ranging from zero to high. Numbers from the first affected region in Italy, Lombardy, show an all age mortality rate of 154 per 100 000 population. Differences are most likely due to varying demographic structures, among other factors. However, this new virus has a focal dissemination; therefore, some areas have a higher disease burden and are affected more than others for reasons that are still not understood. Nevertheless, early introduction of strict physical distancing and hygiene measures have proven effective in sharply reducing R0 and associated mortality and could in part explain the geographical differences.
- Eskild Petersen, Marion Koopmans, Unyeong Go, Davidson H Hamer, Nicola Petrosillo, Francesco Castelli, Merete Storgaard, Sulien Al Khalili, Lone Simonsen; “Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics”, The Lancet, Volume 20, ISSUE 9, e238-e244, (September 01, 2020)
- Clinical case fatality, for which the case definition was fever and respiratory symptoms (including pneumonia), was around 5% in Hubei province and only around 1% in the rest of China and South Korea. In the USA, case fatality rates among patients with COVID-19 were less than 1% for people aged 20–54 years, 1–5% in those aged 55–64 years, 3–11% in those aged 65–84 years, and 10–27% in people aged 85 years and older. Early in the outbreak there have been few deaths in children and young adults younger than 20 years. Although most patients (90%) with COVID-19 have mild clinical illness, there is considerable demand for intensive care because of the subset of patients who develop acute respiratory distress syndrome. This requirement for respiratory support is higher for SARS-CoV-2 cases than for the influenza pandemic in 2009. In a study of patients who were admitted to hospital in New York, NY, USA, 14% required intensive care (median age 68 years).
- Eskild Petersen, Marion Koopmans, Unyeong Go, Davidson H Hamer, Nicola Petrosillo, Francesco Castelli, Merete Storgaard, Sulien Al Khalili, Lone Simonsen; “Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics”, The Lancet, Volume 20, ISSUE 9, e238-e244, (September 01, 2020)
- The first WHO “disease X” scenario has become a reality. The SARS-CoV-2 pandemic has already caused severe morbidity and mortality in older adults, much higher than in the pandemic influenza. Although children are clearly less affected, their role in the transmission of the virus still needs to be studied.
- Eskild Petersen, Marion Koopmans, Unyeong Go, Davidson H Hamer, Nicola Petrosillo, Francesco Castelli, Merete Storgaard, Sulien Al Khalili, Lone Simonsen; “Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics”, The Lancet, Volume 20, ISSUE 9, e238-e244, (September 01, 2020)
- To affirm a reinfection, scientists should study the genetic code of the virus from every spherical of sickness and show they’re distinct. That means gaining access to each units of swabs and the wherewithal to do entire genome sequencing. Even in hospitals the place the capability exists, such checks are not often accomplished. Reinfected sufferers merely go unnoticed or unreported. “There is probably a lot more than we are seeing,” mentioned Iwasaki.
The immune system’s battle towards coronavirus is unleashed in a number of waves. The first line of defence, the innate immune system, is imprecise however quick. Invading pathogens immediate cells to churn out signalling proteins known as cytokines which name in a military of white blood cells that engulf and disrupt the virus.
Next to gear up is the adaptive immune system, a extra specialised attacking drive. This unleashes T-cells, which destroy contaminated cells, and prompts B-cells to make antibodies that stick with viruses and cease them spreading additional. If and when the an infection is crushed, the T- and B-cells stand down, however some needs to be saved within the physique for years, an immune reminiscence that may be recommissioned ought to the virus attempt once more.
Given the complexity of the immune response, it’s no shock that scientists are struggling to unravel why reinfections happen. Blood checks on sufferers reveal that virus-disabling antibodies can wane after a number of months, notably in these with gentle or no signs. But even with wholesome ranges of antibodies, reinfection cannot solely occur, however trigger extra severe illness.- “Pehal News Team”, "Flurry of coronavirus reinfections leaves scientists puzzled", (Oct. 7, 2020)
- Women who have COVID-19 during childbirth are more likely to face complications than moms-to-be without the coronavirus, researchers say.
Fortunately, the absolute risk for complications for any one woman is very low (less than 1%). But the relative risks for problems -- such as clotting and early labor -- are significant, the new study found.
Still, "the findings here, truly, are that among women who are hospitalized for childbirth and who were diagnosed with COVID, adverse events are incredibly low. That should provide a lot of reassurance to women who are hoping to become pregnant during this period, or who are pregnant," said study co-author Dr. Karola Jering, from the cardiovascular medicine division at Brigham and Women's Hospital in Boston.- Steven Reinberg, “COVID-19 Ups Complication Risks During Childbirth”, “USNews.com”, (Jan. 20, 2021)
- Take a look at the death toll now (as of 5 February 2020 due to the COVID-19 outbreak), there are almost no children. A nine-month-old baby is the youngest known patient, and the baby's still alive. The youngest patients who died are about 30 years old. Most of them have congenital diseases, such as brain disorders, heart diseases, lung diseases, diabetes or cancer. There are patients who are over 80 years old. At first, more than half of them were over 80 years old. Many cases are 89. If you ask me, some 89-year-old people happen to fall and die. So, don't panic about the number of fatalities. A majority of them have congenital diseases, pneumonia or influenza. Their depth of breathing is lower than normal, and there's a possibility that they want to eliminate excess phlegm. This can pose a life-threatening risk. Most fatalities are not young people. There's not much difference from the common influenza. If people who are 89 or 90 years old have influenza, that's not good.
- Yong Poovorawan (2020) cited in "Virologist says measures must be implemented for one year to address coronavirus" on Pattaya Mail, (5 February 2020).
- Making it (COVID-19) a notifiable disease would give them (Auckland Regional Public Health Service) more powers to isolate and quarantine people who might have been exposed (to the virus as they enter New Zealand), as well as monitor their health.
- William Rainger (2020) cited in: "China coronavirus checks: 'Looking for a needle in a haystack'" in RNZ, (27 January 2020).
- One thing about this (COVID-19) that's somewhat unprecedented is the speed at which new data is coming out and becoming available for mass consumption. In that article, there's not a lot of detail about when the initial patient returning to China became symptomatic. It's really hard to tell. People don't always accurately report. That's not on purpose or anything, but people aren't so self-aware that they're going to notice a single sneeze, or every little cough, or clearing their throat, or their nose is running and they think it's allergies. There are a lot of reasons why people might not necessarily recognize that they are symptomatic when they actually are.
- Angela Rasmussen (2020) cited in ""Talking to a Virologist About How Worried We Should Be About Coronavirus" on Intelligencer, (31 January 2020).
- The absence of a vaccine and effective treatment for COVID-19 has created public panic and burdened the health systems in most countries. Along with health workers’, sanitation personnel are also working at the frontlines in the war against the disease by keeping cities clean. Sanitation workers are engaged in Drudgery, Dangerous, Dirty and Dehumanising work that makes them vulnerable for developing the chronic respiratory diseases due to the exposure of various hazardous materials and toxic gases that are emitted from the solid waste. The sanitation workers working on a contractual basis are excluded from the labour policies and welfare programs who are playing a vital role in fighting the pandemic. Women sanitation workers are even more vulnerable because most of them are non-literate, poor in financial management and under-represented in the sanitation employee’s union. The local and state governments should protect and safeguard sanitation workers by providing them with adequate protective equipment, ensure payment of paying adequate salaries and provide them with health insurance.
- Pradeep S. Salve & Suresh Jungari ”Sanitation workers at the frontline: work and vulnerability in response to COVID-19”, Local Environment, Volume 25, 2020 - Issue 8, pp.627-630, (published online: 13 Jul 2020)
- The COVIDSurg Collaborative's study of surgical outcomes in patients with COVID-19 is commendable, as most existing publications around perioperative practice are commentaries or recommendations with extrapolated knowledge.
The study findings suggest a grievous prognosis for patients having surgery during the COVID-19 pandemic, in that nearly one in four (23•8% [268 of 1128]) patients die within 30 days, and about half (51•2% [577]) of them will have major pulmonary complications. Factors associated with these outcomes were non-modifiable, except for the decision of elective surgery. Even among elective surgeries, delaying cancer surgery might have its own consequences. Hence, it becomes crucial to look for modifiable risk factors, such as the anaesthetic type.
Although unproven in people with COVID-19, preference for regional anaesthetic over general anaesthesia has advantages such as minimal effect on the respiratory system, avoidance of intubation-related seeding of pathogens to the lower respiratory tract, decreasing thromboembolic complications, and a reduced surgical stress response.
Using regional anaesthetic techniques, aerosol-generating procedures can be avoided with decreased risk to health personnel; additionally, there is potential to conserve protective equipment and essential drugs during shortages.- Harsha Shanthanna, Vishal Uppal; “Surgery during the COVID-19 pandemic”, The Lancet, e74, (November 07, 2020)
- Today, some of those data were published in CDC’s Morbidity and Mortality Weekly Report (MMWR), demonstrating that Delta infection resulted in similarly high SARS-CoV-2 viral loads in vaccinated and unvaccinated people. High viral loads suggest an increased risk of transmission and raised concern that, unlike with other variants, vaccinated people infected with Delta can transmit the virus. This finding is concerning and was a pivotal discovery leading to CDC’s updated mask recommendation. The masking recommendation was updated to ensure the vaccinated public would not unknowingly transmit virus to others, including their unvaccinated or immunocompromised loved ones.
- “Statement from CDC Director Rochelle P. Walensky, MD, MPH on Today’s MMWR”, CDC, (July 30, 2021)
- Catching COVID-19 may raise the risk of developing autoimmune disease by 43% in the months following the infection, according to the largest study of its kind.
"The impact of this study is huge — it's the strongest evidence so far answering this question of COVID-19 and autoimmune disease risk," said Anuradhaa Subramanian, a research fellow in health informatics at the University of Birmingham, who was not involved in the study.- Carissa Wong quoting Anuradhaa Subramanian, “COVID-19 linked to 40% increase in autoimmune disease risk in huge study”, Live Science, (2/24/2023)
- "These findings just cannot be ignored," Subramanian said. "We need to pursue research into how COVID-19 is potentially triggering autoimmunity because many people are continuing to suffer from the effects of COVID-19." There are several hypotheses as to how COVID-19 might trigger autoimmunity, and it's possible that different mechanisms affect different organ systems, the researchers noted.
- Carissa Wong quoting Anuradhaa Subramanian, “COVID-19 linked to 40% increase in autoimmune disease risk in huge study”, Live Science, (2/24/2023)
- "Understanding how COVID-19 impacts autoimmune disease risk will help in executing the prevention measures and early treatments to prevent associated morbidity and mortality," said Jagadeesh Bayry, a professor of biological sciences and engineering at the Indian Institute of Technology Palakkad who was not involved in the study.
- Carissa Wong quoting Jagadeesh Bayry, “COVID-19 linked to 40% increase in autoimmune disease risk in huge study”, Live Science, (2/24/2023)
- Although the large sample size makes this a strong study, it is worth noting that it "only shows an association between COVID-19 and autoimmune disease but doesn't prove causality," said Dr. Atsushi Sakuraba, an associate professor of gastroenterology at the University of Chicago who was not involved in the research.
- Carissa Wong quoting Atsushi Sakuraba “COVID-19 linked to 40% increase in autoimmune disease risk in huge study”, Live Science, (2/24/2023)
- The implications of COVID-19 infection during pregnancy remain unclear at this moment. Pregnancy is considered high risk as this population remains vulnerable to coronavirus infection. Till date, data regarding SARS-CoV-2 infection amongst pregnant women, their manifestations and outcomes remain limited. Most pregnancies had good outcomes, and transmission of SARS-CoV-2 to infant was uncommon. However, the relationship between SARS-CoV-2 infection and risk of miscarriage remains unclear.
- Tze Cheng Wong, Zhi Yuan Lee, Tonnii L. L. Sia, Andrew K. W. Chang, and Hock Hin Chua; “Miscarriage Risk in COVID-19 Infection“, SN Compr Clin Med. (2020 Aug 15): 1–4.
- Our (Government of Hong Kong) primary duty is to care for (COVID-19) patients. Everyone can hold a different political view and different thoughts, as well as different views on the (Hong Kong) government's way of combating the pandemic. But I sincerely hope, amid choppy waters and at a critical moment, we can all put aside our conflicts ... and do our share for patients who need help.
- Anthony Wu (2020) cited in "Hong Kong hospital strike kicks off as top doctor backs mainland China border closure calls amid coronavirus fears" on South China Morning Post, 3 February 2020.
- From observations, the (COVID-19) virus is capable of transmission even during incubation period. Some patients have normal temperatures and there are many milder cases. There are hidden carriers. There are signs showing the virus is becoming more transmissible. These walking "contagious agents" (hidden carriers) make controlling the outbreak a lot more difficult.
- Ma Xiaowei (2020) cited in "5 million left Wuhan before lockdown, 1,000 new coronavirus cases expected in city" on South China Morning Post, 26 January 2020.
- We (France) are going to have patients suspected of having the (COVID-19) virus, there are going to be (more) cases.
- Yazdan Yazdanpanah (2020) cited in: "French carmaker to evacuate expats from virus-hit Chinese city" in Borneo Post Online, 26 January 2020.
- In general however, those hit by the new (COVID-19) virus are in a less serious condition than with SARS.
- Yazdan Yazdanpanah (2020) cited in: "Here's The Science on How Serious The Wuhan Coronavirus Outbreak Actually Is" in Science Alert, 29 January 2020.
- SARS-CoV-2 infects less than 1% of cells in the human body, yet it can cause severe damage in a variety of organs. Thus, deciphering the non-cell-autonomous effects of SARS-CoV-2 infection is imperative for understanding the cellular and molecular disruption it elicits. Neurological and cognitive defects are among the least understood symptoms of COVID-19 patients, with olfactory dysfunction being their most common sensory deficit. Here, we show that both in humans and hamsters, SARS-CoV-2 infection causes widespread downregulation of olfactory receptors (ORs) and of their signaling components. This non-cell-autonomous effect is preceded by a dramatic reorganization of the neuronal nuclear architecture, which results in dissipation of genomic compartments harboring OR genes. Our data provide a potential mechanism by which SARS-CoV-2 infection alters the cellular morphology and the transcriptome of cells it cannot infect, offering insight to its systemic effects in olfaction and beyond.
- Marianna Zazhytska, Albana Kodra, Daisy A. Hoagland, Benjamin R. tenOever, Jonathan B. Overdevest, Stavros Lomvardas; “Non-cell-autonomous disruption of nuclear architecture as a potential cause of COVID-19-induced anosmia”, Cell, Volume 185, ISSUE 6, P1052-1064.e12, (March 17, 2022)
- We have developed an effective treatment plan (to patients contracting COVID-19) based on our experience of dealing with SARS, by employing various life support methods to (achieve) a higher rate of recovery.
- Zhong Nanshan (2020) cited in "China starts clinical trials for new antiviral drug to treat coronavirus" on South China Morning Post, 3 February 2020.
“Could COVID delirium bring on dementia?” (2/12/2020)
[edit]Carrie Arnold, “Could COVID delirium bring on dementia?”, Nature 588, (02 December 2020), pp.22-24


- Physicians treating people hospitalized with COVID-19 report that a large number experience delirium, and that the condition disproportionately affects older adults. An April 2020 study in Strasbourg, France, found that 65% of people who were severely ill with coronavirus had acute confusion — a symptom of delirium1. Data presented last month at the annual meeting of the American College of Chest Physicians by scientists at the Vanderbilt University Medical Center in Nashville, Tennessee, showed that 55% of the 2,000 people they tracked who were treated for COVID-19 in intensive-care units (ICUs) around the world had developed delirium. These numbers are much higher than doctors are used to: usually, about one-third of people who are critically ill develop delirium, according to a 2015 meta-analysis2 (see ‘How common is delirium?’).
Delirium is so common in COVID-19 that some researchers have proposed making the condition one of the disease’s diagnostic criteria. The pandemic has sparked physicians’ interest in the condition, says Sharon Inouye, a geriatrician at the Marcus Institute for Aging and Harvard Medical School in Boston, who has studied delirium for more than 30 years. - As clinicians face the immediate realities of confusion and agitation on their wards, Inouye and other researchers are concerned about the future. In the past decade, long-term studies have revealed that a single episode of delirium can increase the risk of developing dementia years later3, and accelerate rates of cognitive decline in those who already have the condition4. The reverse is also true: having dementia makes someone more likely to develop delirium3. A set of simple steps, such as ensuring a family member is present to help people orient themselves, can reduce the incidence of delirium by 40%, but doctors struggle to follow that advice on COVID-19 wards.
- If the pandemic can be said to have a silver lining, says Inouye, it has been to spur interest in how delirium can lead to dementia — and vice versa. What’s more, says Catherine Price, a neuropsychologist at the University of Florida in Gainesville, the spread of COVID-19 “has highlighted the blurring of the lines between delirium and dementia, especially with more older adults in our populace”.
- As Crosby endured coronavirus-induced delirium in her Boston bedroom, Poloni was treating delirious people with COVID-19 in Lombardy — Italy’s ground zero for the coronavirus. Many of Poloni’s patients already had dementia and, like many physicians, he was watching for common symptoms of respiratory infections such as fever, cough and difficulty breathing. But some of his patients didn’t show those signs at all. Instead, they mostly became “dull and sleepy”, Poloni said. Others became restless and agitated — all signs of delirium. It was so prominent that Poloni argued that delirium should be added to the virus’s diagnostic criteria. Inouye has made that argument, too, and it is supported by a study she published last month showing that 28% of older adults with COVID-19 have delirium when they present to the emergency department11.
The high numbers of people who developed delirium immediately made Inouye, Price and other researchers worry that the pandemic could lead to a surge in dementia cases in the coming decades, on top of the increase in cases as a result of ageing populations (see ‘The cost of delirium’). “Is there going to be an increase in dementia from people who had COVID-19 during adulthood or midlife?” asks Natalie Tronson, a neuropsychologist at the University of Michigan in Ann Arbor. “What happens over the next decades, as the population ages more?” - To begin to find answers, institutes around the world have funded a variety of studies into the long-term cognitive effects of COVID-19, some of which will look at delirium. Already under way in the United States is a study tracking people who have been treated in hospital for COVID-19, many of whom developed delirium during their stay. This study will measure cognitive and psychiatric function in people participating in a trial to assess the safety and efficacy of hydroxychloroquine to treat coronavirus. An international study is planned to measure the prevalence of delirium in people with COVID-19 in ICUs, as well as identifying factors that predict long-term outcomes. A separate study in Germany and the United Kingdom is also tracking neurocognitive outcomes in people with COVID-19 to determine how delirium affects brain function months later. Another research project led by a team at Vanderbilt University is looking for an alternative to commonly-used sedatives such as benzodiazepines, which are known to increase delirium. The researchers are testing a sedative called dexmedetomidine to see whether it is a safer option for people hospitalized with COVID-19.
“Millions still without sense of smell or taste after Covid-19” (July 27, 2022)
[edit]Evan Bush, “Millions still without sense of smell or taste after Covid-19”, NBC, (July 27, 2022)
- Losing smell has been linked to higher death rates in older adults and has been shown to have major impacts on people’s emotional and psychological well-being, said Dr. Zara Patel, a rhinologist at Stanford University who was not involved in The BMJ research.
“Having these now millions more people worldwide with decreased ability to smell — that may simply be a new public health crisis,” Patel said.
Loss of smell was one of the most distinct markers of Covid-19 in the pandemic’s beginning days.
“You could track the pandemic across the globe” by analyzing Google searches about smell loss, Patel said. - Patients who suffered smell loss after Covid-19 make up a unique subset, said Dr. Aria Jafari, a rhinologist at the UW Medicine Sinus Center in Seattle, who was not involved in the new analysis. “They tend to get better and kind of quickly, which makes sense based on the cells that are affected.”
Jafari said about half of his patients deprived from the sense of smell likely had Covid-19 at some point. Many experienced dramatic impacts on their well-being because of the loss. - “Many previous studies have shown that objective smell testing can identify far more people with smell loss than if we asked them to self-report,” wrote Professor Song Tar Toh, an author of the study and head of the department of Otolaryngology-Head & Neck Surgery at Singapore General Hospital, in an email. “The true number of people affected is likely to be far higher than our estimate.”
Patel suspects the true rate of smell dysfunction among those who have experienced Covid-19 could be above 20%. - Patel said she hopes research funding and public interest in smell and taste dysfunction continue to grow so researchers can dive deeper and unlock new treatments.
Before the pandemic, “it was the orphan, Cinderella sense,” Patel said. “It’s only after so many millions of people have been affected or had loved ones affected that people are coming to understand the huge impacts smell and taste have on your quality of life.”
“Risk of autoimmune diseases in patients with COVID-19: a retrospective cohort study” (February 2023)
[edit]Renin Chang, Thomas Yen-Ting Chen, Shiow-Ing Wang Yao-Min Hung, Hui-Yuan Chen, Cheng-Chung James Wei; “Risk of autoimmune diseases in patients with COVID-19: a retrospective cohort study”, The Lancet, Volume 56, (February 2023)
- COVID-19 has been reported to present immunological features that resemble those of autoimmune diseases, such as over-activation of mature natural killer cells, CD8+ T cells, 7 and dysregulation of B cells and T cells. Also, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may lead to dysregulation of immune response and increased inflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-1 and IL-6. Cases of autoimmune diseases following SARS-CoV-2 infection have been reported. The incidence of Kawasaki-like disease (now recognized as multisystem inflammatory syndrome in children, MIS-C) has been observed to increase during the COVID-19 epidemic. Some case reports showed the development of Guillain-Barré syndrome after a SARS-CoV-2 infection. Cases of systemic lupus erythematosus and psoriasis triggered by COVID-19 had also been reported. However, no large-scale study had assessed whether COVID-19 survivors have an increased risk of new-onset autoimmune diseases compared with those without COVID-19.
- p.2
- The current large propensity scores-matched study of a multi-institutional U.S. Collaborative Research Network showed that patients with a positive PCR test result for COVID-19 had significantly higher risks of autoimmune diseases including rheumatoid arthritis, ankylosing spondylitis, systemic lupus erythematosus, dermatomyositis, systemic sclerosis, Sjögren’s yndrome, mixed connective tissue disease, Behçet’s disease, polymyalgia rheumatica, vasculitis, psoriasis, inflammatory bowel disease, celiac disease, type 1 diabetes, and also mortality, when compared to “PCR test-negative” non-COVID-19 controls. The results were cross validated in another dataset from TriNetX. The results of subgroup analysis by sex and age were generally consistent. The results of subgroup analysis by race indicated some racial disparity. When compared to their non-COVID-19 counterparts, COVID-19 patients were associated with a significant higher risk of all autoimmune diseases and mortality in Whites, a higher risk of psoriasis and ankylosing spondylitis in Blacks, and a higher risk of systemic lupus erythematosus in Asians. Also, some discrepancy in risks of autoimmune diseases was found between inpatient and outpatient COVID-19 patients. COVID-19 was associated with increased risks of all autoimmune diseases and also mortality among outpatients, while COVID-19 inpatients were found with increased risks of psoriasis and mortality, but significantly lower risks of systemic sclerosis and inflammatory bowel disease.
- pp.8-9
- Viruses play a significant role in the environmental factors that affect human immune system. Cytomegalovirus 28 and Epstein–Barr virus 6 are examples of viruses that have been linked to numerous autoimmune diseases, and now SARS-CoV-2 has the potential to be added to the list. The definite mechanisms underlying such phenomena are unknown. According to recent research, viruses can trigger autoimmunity through a number of different mechanisms, including molecular mimicry, epitope spreading, and bystander activation. We hypothesized that the prolonged inflammation in COVID-19 might trigger the immune system to create antibodies against virus antigens that share structural similarities with self-antigens and further lead to a cross-reactive response against both self-antigens and non-self-antigens. Also, the hyper-stimulation and dysregulation of inflammation and immune response following SARS-CoV-2 infection may contribute to other environmental disturbances that lead to the observed disease in susceptible individuals. Cañas proposed the theory that COVID-19 triggers autoimmune conditions by two factors: temporary impairment of innate and acquired immunity resulting in a loss of self-tolerance to self-antigens, and an inappropriate immune reconstitution in people with predisposing conditions of auto-immunity. Besides, the above-mentioned autoimmune phenomenon may also contribute to the development of post-COVID-19 syndrome (PCS). Given the current evidence on latent autoimmunity in PCS, we could further anticipate a higher incidence of autoimmune diseases in COVID-19 cases with enough follow-up time. In addition, there are other potential mechanisms that could contribute to the association between COVID-19 and autoimmunity diseases. For example, previous studies have reported excessive neutrophil extracellular traps being involved in rheumatoid arthritis and myositis and neutrophil extracellular traps has also been associated with COVID-19 pathogenesis. Contrarily, there is also mounting evidence that viruses could play a protective role against autoimmunity, whereby viral infections trigger regulatory immune responses, which in turn prevent the onset of autoimmune reactions. It is reasonable that the dual impact of viral infections on autoimmunity is coordinated by different host, viral and environmental factors.
- pp.9-10
”Rogue antibodies could be driving severe COVID-19” (1/2021)
[edit]Roxannee Khamsi, “Rogue antibodies could be driving severe COVID-19”, Nature, (January 2021), 590, pp.29-31

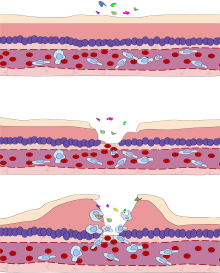
Lee, the researcher who studied annexin A2, says the evidence that infections can give rise to autoimmunity is not receiving enough attention. “It should make us rethink dozens of diseases, if not hundreds,” he says. “I’m like, ‘How is anybody not seeing this?’”
- More than a year after COVID-19 emerged, many mysteries persist about the disease: why do some people get so much sicker than others? Why does lung damage sometimes continue to worsen well after the body seems to have cleared the SARS-CoV-2 virus? And what is behind the extended, multi-organ illness that lasts for months in people with ‘long COVID’? A growing number of studies suggest that some of these questions might be explained by the immune system mistakenly turning against the body — a phenomenon known as autoimmunity.
“This is a rapidly evolving area, but all the evidence is converging,” says Aaron Ring, an immunologist at the Yale School of Medicine in New Haven, Connecticut.
Early in the pandemic, researchers suggested that some people have an overactive immune response to COVID infection. Immune-system signalling proteins called cytokines can ramp up to dangerous levels, leading to ‘cytokine storms’ and damage to the body’s own cells. Clinical trials have now shown that some drugs that broadly dampen immune activity seem to reduce death rates in critically ill people, if administered at the right time.
But scientists studying COVID are increasingly also highlighting the role of autoantibodies: rogue antibodies that attack either elements of the body’s immune defences or specific proteins in organs such as the heart. In contrast to cytokine storms, which tend to cause systemic, short-duration problems, autoantibodies are thought to result in targeted, longer-term damage, says immunologist Akiko Iwasaki, a colleague of Ring’s at Yale. - Yehuda Shoenfeld, head of the Zabludowicz Center for Autoimmune Diseases in Tel-Hashomer, Israel, suspects that COVID-19 might cause autoimmune disease. Last June, he published an article about COVID-19 and autoimmunity, and cited an April 2020 case report of a 65-year-old woman with COVID-19 whose platelet count dropped precipitously and who required a platelet transfusion7. Although there is not enough evidence to prove that this was ITP, there have been a few dozen other cases of ITP linked to COVID-19 in the literature.
Some people might have a genetic predisposition to developing an autoimmune reaction in response to infection. For example, certain individuals have DNA that encodes the immune-system protein HLA-DRB1, which Shoenfeld says is “notorious” for its link to autoimmunity. A related protein, HLA-DQB1, is strongly suspected to have put individuals receiving a now-discontinued vaccine against the H1N1 ‘swine flu’ at risk of developing a form of narcolepsy that is thought to result from an autoimmune attack on neurons in the brain. - Another way pathogens might trigger immunity is if a part of them coincidentally resembles human cell components. For example, S. pyogenes has an ‘M’ protein that mimics certain proteins found in the human heart. This is known as molecular mimicry. In their June 2020 article, Shoenfeld and his collaborators found similarities between numerous short sequences of the SARS-CoV-2 spike protein, which the virus uses to enter the cell, and human proteins. Others caution, however, that this might not have meaningful effects. “This is not to say that mimicry by pathogens is not a real thing,” says Brian Wasik, a virologist at Cornell University in Ithaca, New York. “But most instances of such mimicry have been defined by testing how the pathogens’ proteins actually react to antibodies in the lab.”
Another theory is that inflammation caused by an infection might prime the immune system to mistakenly see the spewed contents of destroyed cells as ‘foreign’ and create autoantibodies against these cellular pieces, says Leona Gilbert, a molecular biologist who is a consultant at a diagnostic company named Te?ted Oy in Finland, which has developed and sells a test for SARS-CoV-2 antibodies. The tissue damage that accompanies inflammation is a recipe for the body to begin attacking itself, Gilbert says: “That just precipitates the whole event in developing autoimmune conditions,” she says.
Lee, the researcher who studied annexin A2, says the evidence that infections can give rise to autoimmunity is not receiving enough attention. “It should make us rethink dozens of diseases, if not hundreds,” he says. “I’m like, ‘How is anybody not seeing this?’” - Even before autoantibodies came into focus, the idea that a cytokine storm might be a culprit meant that studies were under way to see whether immunosuppressive steroids such as dexamethasone, or the arthritis drugs tocilizumab and sarilumab, could be used to calm immune systems set awry by COVID. The World Health Organization now “strongly recommends” the use of dexamethasone in severe cases, and the United Kingdom is using the arthritis drugs for people with severe COVID after a clinical trial on 7 January suggested that they cut death rates in patients in intensive care.
- Physicians emphasize that, whether they are used to quell a cytokine storm or to try to address autoimmunity, administration of the drugs needs to be carefully timed so that they don’t interfere with the body’s battle against SARS-CoV-2. Suri notes that broad-spectrum immunosuppressants make the body more prone to infection. His company is one of a handful conducting preclinical work to develop engineered molecules that go after specific immunity pathways, rather than suppress immunity across the board.
Lee, meanwhile, says that if autoantibodies against annexin A2 and other proteins prove to be a consequence of COVID-19, then it might make sense to study what happens when patients’ plasma is run through a process that clears these antibodies out before returning the plasma.
Scientists are very interested in understanding whether autoimmunity is linked to long COVID, too. “First of all, we don’t know if these autoantibodies contribute to long COVID, but if they do, what is the longevity? How long will they last? How long is the body going to keep producing those antibodies?” Ring says. But answering these questions is a complicated endeavour, because people naturally produce many different kinds of antibody, including autoantibodies.
“U.K. variant puts spotlight on immunocompromised patients’ role in the COVID-19 pandemic” (12/23/2020)
[edit]Kai Kupferschmidt, “U.K. variant puts spotlight on immunocompromised patients’ role in the COVID-19 pandemic” Science, (Dec. 23, 2020)
- Now, his analysis, reported in a preprint on medRxiv earlier this month, has become a crucial puzzle piece for researchers trying to understand the importance of B.1.1.7, the new SARS-CoV-2 variant first found in the United Kingdom. That strain, which appears to spread faster than others, contains one of the mutations that Gupta found, and researchers believe B.1.1.7, too, may have originated in an immune compromised patient who had a long-running infection. “It’s a perfectly logical and rational hypothesis,” says infectious disease scientist Jeremy Farrar, director of the Wellcome Trust.
Scientists are still trying to figure out the effects of the mutations in B.1.1.7, whose emergence led the U.K. government to tighten coronavirus control measures and other countries in Europe to impose U.K. travel bans. But the new variant, along with research by Gupta and others, has also drawn attention to the potential role in COVID-19 of people with weakened immune systems. If they provide the virus with an opportunity to evolve lineages that spread faster, are more pathogenic, or elude vaccines, these chronic infections are not just dangerous for the patients, but might have the potential to alter the course of the pandemic. - So far, SARS-CoV-2 typically acquires only one to two mutations per month. And B.1.1.7 is back to this pace now, suggesting it doesn’t mutate faster normally than other lineages. That’s why scientists believe it may have gone through a lengthy bout of evolution in a chronically infected patient who then transmitted the virus late in their infection. “We know this is rare but it can happen,” says World Health Organization epidemiologist Maria Van Kerkhove. Stephen Goldstein, a virologist at the University of Utah, agrees. “It’s simply too many mutations to have accumulated under normal evolutionary circumstances. It suggests an extended period of within-host evolution,” he says.
People with a weakened immune system may give the virus this opportunity, as Gupta’s data show. More evidence comes from a paper published in The New England Journal of Medicine on 3 December that described an immunocompromised patient in Boston infected with SARS-CoV-2 for 154 days before he died. Again, the researchers found several mutations, including N501Y. “It suggests that you can get relatively large numbers of mutations happening over a relatively short period of time within an individual patient,” says William Hanage of the Harvard T.H. Chan School of Public Health, one of the authors. (In patients who are infected for a few days and then clear the virus, there simply is not enough time for this, he says.) When such patients are given antibody treatments for COVID-19 late in their disease course, there may already be so many variants present that one of them is resistant, Goldstein says. - U.K. scientists and others were initially cautious about concluding that B.1.1.7’s mutations made the virus better at spreading from person to person. But the new variant is rapidly replacing others, says Müge Çevik, an infectious disease specialist at the University of St. Andrews. “We can’t really rule out the possibility that seasonality and human behavior explain some of the increase,” she says. “But it certainly seems like there is something to do with this variant.” Drosten says he was initially skeptical, but has become more convinced as well.
But exactly what impact each mutation has is much more difficult to assess than spotting them or showing they’re on the rise, says Seema Lakdawala, a biologist at the University of Pittsburgh. Animal experiments can help show an effect, but they have limitations. Hamsters already transmit SARS-CoV-2 virus rapidly, for instance, which could obscure any effect of the new variant. Ferrets transmit it less efficiently, so a difference may be more easily detectable, Lakdawala says. “But does that really translate to humans? I doubt it.” A definitive answer may be months off, she predicts.
One hypothesis that scientists are discussing is that the virus has increased how strongly it binds to the ACE2 receptor on human cells, and that this allows it to better infect children than before, expanding its playing field. But the evidence for that is very thin so far, Çevik says. Even if children turn out to make up a higher proportion of people infected with the new variant, that could be because the variant spread at a time when there was a lockdown but schools were open. Another hypothesis is that P681H helps the virus better infect cells higher up in the respiratory tract, from where it can spread more easily than from deep in the lungs, Drosten says.
“Why do COVID death rates seem to be falling?” (11/11/2020)
[edit]Heidi Ledford, “Why do COVID death rates seem to be falling?”, Nature 587, (11 November 2020), pp.190-192.
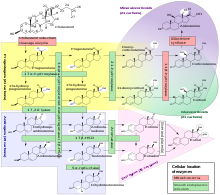


- Researchers have struggled to work out whether the COVID-19 death rates are truly dropping. The calculations can be complex. Case-fatality rates depend on testing: a country that tests only people with severe symptoms, for example, will have an outsized case-fatality rate compared with one in which asymptomatic testing is widespread. And fatality rates in intensive-care units can mislead if the demographics of the people admitted change over time. For example, many hospitals reported high numbers of younger patients as the pandemic wore on.
The detailed data that are needed to parse these differences have been hard to come by in many countries, and that frustrates Andrew Levin, an economist at Dartmouth College in Hanover, New Hampshire. “We still don’t have the data that scientists and public-health officials should have,” he says.
As a result, it has taken researchers some time to determine whether the number of deaths per SARS-CoV-2 infection is really falling, particularly for older people, says epidemiologist Ali Mokdad at the University of Washington in Seattle. Mokdad and his colleagues have been monitoring global data, with a focus on the United States and Europe. A provisional analysis, he says, which includes data from the American Hospital Association, now suggests that the number of fatalities per infection might have fallen by 20%. - In contrast to more-targeted drugs, blanket suppression of the immune system using steroids has been shown to cut death rates when used to treat severe COVID-19. On 16 June, the UK RECOVERY trial found that a common steroid called dexamethasone could reduce COVID-19 fatalities by as much as one-third when administered to patients who require supplemental oxygen or are on ventilators. (However, Summers cautions that dexamethasone treatment has not been shown to carry a benefit for people with mild COVID-19 who do not need oxygen support, possibly because it weakens defences against the virus itself.)
- Thus far, steroids are the only medicine that has been shown to have a dramatic effect on COVID-19 mortality. “Anyone who’s very sick should get steroids,” says Angus. “And everything else is a crapshoot.”
The antiviral drug remdesivir, developed by the biopharmaceutical company Gilead Sciences in Foster City, California, has been shown by a US National Institutes of Health study to shorten hospital stays7. A subsequent trial coordinated by the World Health Organization found that the drug had little, if any, effect on mortality, but the US Food and Drug Administration nevertheless approved it for treating COVID-19 on 22 October. - Hundreds of other therapies are being tested against COVID-19, but many of the ongoing trials are too small to yield convincing results soon. Among the furthest along are studies of antibodies against SARS-CoV-2 — either purified antibodies administered individually or in cocktails, or antibody-rich blood plasma taken from people recovering from the disease.
Convalescent plasma studies have been hampered in the United States by the widespread availability of the treatment outside clinical trials, but the UK RECOVERY trial hopes to have data on this approach from a large, randomized, controlled trial this year. Meanwhile, a 464-person, open-label study in India found that convalescent plasma did not prevent moderate COVID-19 from progressing to severe disease or reduce deaths8.
Tests of purified antibodies are also under way — such as those assessing the mixture of two antibodies produced by the biotechnology firm Regeneron Pharmaceuticals in Tarrytown, New York, that was administered to US President Donald Trump. These mainly target people who have mild COVID-19 symptoms. Despite Trump’s claims that the treatment was a “cure”, large trials of the cocktail have not yet been completed, and there is no evidence that it has an impact on death rates from COVID-19.
Some studies in people with mild disease have shown that treatment with these antibodies can reduce hospitalizations. However, in October, the US National Institutes of Health halted a trial of an antibody produced by the pharmaceutical company Eli Lilly in Indianapolis, Indiana, in people hospitalized with COVID-19 after finding no benefit from the treatment. Regeneron has also stopped enrolment in a trial of its antibody cocktail for people with severe symptoms. - Some intensive-care researchers are sceptical of the chances that a highly effective medicine will be found, citing decades of failed attempts to find a ‘magic bullet’ for acute respiratory distress. “Apart from a vaccine, I think the differences in outcome will be driven by things like other ways to supply oxygen or help patients in their gas exchange,” says Schultz.
In the early days of the pandemic, physicians were alarmed by the rapid deterioration of some people with COVID-19, says Eddy Fan, an intensive-care physician at University Health Network in Toronto, Canada. “There were a lot of unknowns about the best way to manage this,” he says. “Because the patient could deteriorate very quickly, the thought was to put them on a ventilator and breathing tube quickly to prevent deterioration.”
But, in retrospect, clinicians might have been overzealous at times. Schultz recalls asking patients to get off of their mobile phones so he could put them on a ventilator, but a candidate for a ventilator normally wouldn’t be well enough to hold a telephone conversation. As physicians became more comfortable treating people with COVID-19, many realized that early ventilation was not necessary, says Fan.
Unfortunately, the public began to become concerned that ventilators themselves were causing harm, says Summers. Now, she says, families are upset when physicians recommend that their loved ones be put on a ventilator — even when there are no other suitable ways of providing oxygen. “The narrative you’ve heard is that ventilators kill people,” she says. “That’s been particularly unhelpful.” The NHS health-care centres with the lowest mortality rates during the pandemic used ventilators, but not too early. They followed standard protocols for when to use the devices, says Summers. - This might mean that keeping death rates low could hinge on measures to reduce transmission. In Singapore, where COVID-19 death rates are among the lowest in the world, intensive-care physician Jason Phua at Alexandra Hospital says the key to the country’s success has been suppressing transmission, so that hospitals were never overwhelmed. Early reports of mortality from Wuhan approached 97% for people with COVID-19 who were on ventilators, he says. In Singapore, mortality rates in intensive-care units have been less than 15%. “I don’t think it’s because we are using the correct drugs,” he says. “I think what’s happening is that the others are overwhelmed.”
“The search for animals harbouring coronavirus — and why it matters” (3/2/2020)
[edit]Smriti Mallapati, “The search for animals harbouring coronavirus — and why it matters”, Nature 591, (02 March 2021), pp. 26-28

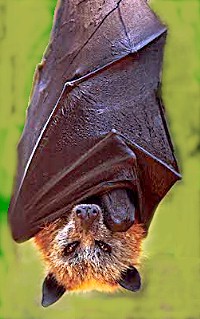



- In theory, the virus could evolve as it circulates among animals — possibly in ways that threaten the efficacy of vaccines or make the pathogen more deadly and infectious to people, says Arinjay Banerjee, a coronavirus researcher at McMaster University in Hamilton, Canada. “Not to sound any alarms, but everything we don’t want to see with this virus seems to happen,” he says.
- In one year, scientists have collected as much data about the susceptibility of different species to SARS-CoV-2 as was accumulated over the past 50 years for influenza, says Martin Beer, a virologist at the Federal Research Institute for Animal Health in Greifswald, Germany.
- Animal infections are rare, and some researchers are reassured by the data collected so far. But others are more cautious. SARS-CoV-2 is known to infect a wide range of animal species (see ‘Animal outbreaks’). This fact, says Gryseels, combined with the large number of infected people, means that, in principle, the virus has had millions of opportunities to jump from people to animals.
Many of those jumps could be passing under the radar. Wildlife studies are difficult to do, and animal infections have not been a priority for much of the research community. The wild mink that tested positive in Utah “could just be the tip of the iceberg”, says Sarah Hamer, an epidemiologist and veterinarian at Texas A&M University in College Station. “The more we look, the more we might find.” - Early in the pandemic, pigs were top of the watchlist. They are known to incubate other viruses, such as influenza, and they live in huge numbers in close proximity to humans — some 300 million pigs are farmed in China, where the pandemic began. “We are always afraid if pigs are involved,” says Beer.
Pigs can also host coronaviruses. In 2018, researchers described a new bat coronavirus that had killed some 25,000 pigs in southern China. And in February 2020, scientists working on SARS-CoV-2 showed that it could enter pig cells through the ACE2 protein — the same receptor that it uses to infect people.
But when researchers began artificially infecting pigs and piglets with SARS-CoV-2, they found that it did not replicate well. These studies suggest that pigs are largely resistant to infection with the virus. “Thank goodness, because with the volume of pig production globally, that would have been a huge problem,” says Peter Daszak, president of the non-profit research organization Ecohealth Alliance in New York City. - Because bats and humans aren’t often in close contact, it’s highly unlikely that people will spread the virus to colonies that haven’t been exposed, says Kaitlin Sawatzki, a virologist at Tufts University in Boston, Massachusetts.
She and her colleagues have tested 321 bats captured from across the northeastern United States and have detected no SARS-CoV-2 viral RNA so far. Scientists say that risk could increase when the pandemic eases and travel and tourism ramp up, along with research and conservation work. - Yet even when animals are in very close contact with humans, the barrier to natural infection can be high. In one striking example, Sawatzki tested 29 pet ferrets whose owners had contracted COVID-19. As the owners convalesced at home, tired and feverish, they cuddled, groomed and lounged on their beds with their ferrets, and yet none of their pets tested positive for viral RNA or for antibodies against the infection. “I could not have been more surprised,” says Sawatzki.
- In laboratory settings, cats are easily infected and are contagious to other cats. They also don’t get very sick, which means that detecting infection is tricky.
But they get over infection quickly, which means that they probably aren’t infectious for long, says Angela Bosco-Lauth, an infectious-disease researcher at Colorado State University in Fort Collins, who has studied the effects of SARS-CoV-2 infection in cats. “I don’t think cats pose any risk to human health, even in the long term,” she says. - Several surveys reveal low rates of infection in cats, and no cats have been reported to have passed the infection on to people in a natural setting. Of 920 blood samples taken from a random collection of cats in Germany between April and September, during the first pandemic wave, Beer and his colleagues found only 6 with antibodies against SARS-CoV-2 — some 0.7% — corresponding to the low rates of infection detected in people. A study in a region of northern Italy that was hit hard by the pandemic found that around 6% of 191 house cats had SARS-CoV-2 antibodies.
“There is no reason to be sensational and to be afraid of cats, but you cannot exclude them as a potential, sporadic source of infection in people,” says Jan Felix Drexler, a virologist at the Charité hospital in Berlin. - No amount of lab work or fieldwork, however, could have prepared scientists for what has happened on mink farms, says Linfa Wang, a virologist at Duke–National University of Singapore Medical School. “The virus taught us a lesson with mink. It said, ‘You guys can never catch me.’”
An unusual spike in mink deaths at two farms in the Netherlands — and a strong surveillance system — alerted researchers to the first -outbreaks, in April. By the end of 2020, SARS-CoV-2 had reached 70 Dutch farms, as well as farms in about a dozen other countries, including Denmark, Greece, Canada and the United States.
Sawatzki describes the situation in the farms as the “perfect storm”. Animals susceptible to infection are packed together and are in regular, direct contact with infected farmers. In one Danish farm, for example, some 97% of the tested mink had antibodies against SARS-CoV-2, a jump from 6% only 8 days earlier, says Anette Boklund, an epidemiologist at the University of Copenhagen. - Some researchers worry that, over time, minor genomic tweaks in hundreds or thousands, if not millions, of mink, could eventually add up to changes that make the virus more contagious or more deadly in people, or able to evade treatments and vaccines. In November, researchers in Denmark isolated from mink several variants, one of which, in preliminary cell experiments, evaded antibodies from some people who had recovered from COVID-19. But this variant had been detected in only 12 people and not since mid-September, suggesting that none of those people had passed it on.
- Marion Koopmans, who studies virology at the Erasmus University Medical Centre in Rotterdam, the Netherlands, says she was not surprised that a wild mink had contracted the virus, given the high levels of contamination observed in bedding and dust around affected Dutch farms, and that mink sometimes escape from farms and establish themselves in the wild. More than a dozen mink — caught in the wild but probably escapees from farms with active outbreaks — have tested positive for SARS-CoV-2 viral RNA or antibodies in the United States and the Netherlands.
So far, the mink captured in Utah is the only wild animal to have tested positive, but several national and regional research consortia are continuing to survey wild animals near mink farms for evidence of infection.
Some countries have taken sweeping measures to prevent the virus spreading in mink. Denmark — the world’s largest producer of mink skins — and the Netherlands have culled their entire mink populations, totalling nearly 20 million animals. Other countries are considering vaccinating their mink. The pandemic is “speeding up the end of mink farming”, says Drexler. - The story of mink and COVID-19 has confirmed researchers’ early fears that the virus can find refuge in animals in ways that are difficult to predict and control, and that it can then jump back to people. But it remains unknown whether SARS-CoV-2 can spread efficiently among wild populations, says Koopmans, who is monitoring wild mink in the Netherlands. “Mink are rather solitary animals when left alone, so that may work to our advantage,” she says.
Scientists also wonder what is happening in China regarding mink and other animals farmed for fur, such as the raccoon dog — a fox-like animal that some researchers think could have been an intermediate host of SARS. Very little research on SARS-CoV-2 and animals has been published from China, although a World Health Organization (WHO) team investigating the origins of SARS-CoV-2 said at a press briefing on 9 February that results from testing wild and farmed animals across China had found no evidence of the virus circulating in these animals. - Fast-spreading variants that were first identified in the United Kingdom, South Africa and Brazil have not yet been tested for their ability to infect animals. But all the new variants contain a mutation that can make the virus infectious to laboratory mice (Mus musculus), which are resistant to versions without the mutation. The new variants’ global spread increases the possibility that house mice, and perhaps also rats, will acquire the infection from people and contaminated environments such as sewers, says Gryseels.
“How COVID-19 can damage the brain” (15/9/2020)
[edit]Michael Marshal, 15 “How COVID-19 can damage the brain”, Nature, 585, 342-343, (15 September 2020)


- In the early months of the COVID-19 pandemic, doctors struggled to keep patients breathing, and focused mainly on treating damage to the lungs and circulatory system. But even then, evidence for neurological effects was accumulating. Some people hospitalized with COVID-19 were experiencing delirium: they were confused, disorientated and agitated. In April, a group in Japan published the first report of someone with COVID-19 who had swelling and inflammation in brain tissues. Another report described a patient with deterioration of myelin, a fatty coating that protects neurons and is irreversibly damaged in neurodegenerative diseases such as multiple sclerosis.
- [A] major problem in quantifying cases is that clinical studies have typically focused on people with COVID-19 who were hospitalized, often those who required intensive care. The prevalence of neurological symptoms in this group could be “more than 50%”, says neurobiologist Fernanda De Felice at the Federal University of Rio de Janeiro in Brazil. But there is much less information about those who had mild illness or no respiratory symptoms.
That scarcity of data means it is difficult to work out why some people have neurological symptoms and others do not. It is also unclear whether the effects will linger: COVID-19 can have other health impacts that last for months, and different coronaviruses have left some people with symptoms for years. - The most pressing question for many neuroscientists, however, is why the brain is affected at all. Although the pattern of disorders is fairly consistent, the underlying mechanisms are not yet clear, says De Felice.
Finding an answer will help clinicians to choose the right treatments. “If this is direct viral infection of the central nervous system, these are the patients we should be targeting for remdesivir or another antiviral,” says Michael. “Whereas if the virus is not in the central nervous system, maybe the virus is clear of the body, then we need to treat with anti-inflammatory therapies.”
Getting it wrong would be harmful. “It’s pointless giving the antivirals to someone if the virus is gone, and it’s risky giving anti-inflammatories to someone who’s got a virus in their brain,” says Michael.
There is clear evidence that SARS-CoV-2 can infect neurons. Muotri’s team specializes in building ‘organoids’ — miniaturized clumps of brain tissue, made by coaxing human pluripotent stem cells to differentiate into neurons.
In a May preprint, the team showed that SARS-CoV-2 could infect neurons in these organoids, killing some and reducing the formation of synapses between them. Work by immunologist Akiko Iwasaki and her colleagues at Yale University School of Medicine in New Haven, Connecticut, seems to confirm this using human organoids, mouse brains and some post-mortem examinations, according to a preprint published on 8 September. But questions remain over how the virus might reach people’s brains. - A team led by Mary Fowkes, a pathologist at the Icahn School of Medicine at Mount Sinai in New York City, posted a preprint in late May9 describing post mortems in 67 people who had died of COVID-19. “We have seen the virus in the brain itself,” says Fowkes: electron microscopes revealed its presence. But virus levels were low and were not consistently detectable. Furthermore, if the virus was invading through the olfactory nerve, the associated brain region should be the first to be affected. “We’re simply not seeing the virus involved in the olfactory bulb,” says Fowkes. Rather, she says, infections in the brain are small and tend to cluster around blood vessels.
“The lasting misery of coronavirus long-haulers” (14/9/2020)
[edit]Michael Marshall, “The lasting misery of coronavirus long-haulers”, Nature 585, (14 September 2020), pp. 339-341.
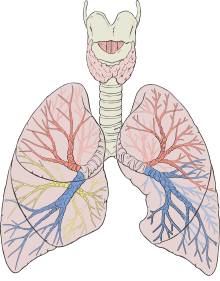

- [L]ung scans were the first sign of trouble. In the early weeks of the coronavirus pandemic, clinical radiologist Ali Gholamrezanezhad began to notice that some people who had cleared their COVID-19 infection still had distinct signs of damage. “Unfortunately, sometimes the scar never goes away,” he says.
Gholamrezanezhad, at the University of Southern California in Los Angeles, and his team started tracking patients in January using computed tomography (CT) scanning to study their lungs. They followed up on 33 of them more than a month later, and their as-yet-unpublished data suggest that more than one-third had tissue death that has led to visible scars. The team plans to follow the group for several years.
These patients are likely to represent the worst-case scenario. Because most infected people do not end up in hospital, Gholamrezanezhad says the overall rate of such intermediate-term lung damage is likely to be much lower — his best guess is that it is less than 10%. Nevertheless, given that 28.2 million people are known to have been infected so far, and that the lungs are just one of the places that clinicians have detected damage, even that low percentage implies that hundreds of thousands of people are experiencing lasting health consequences. - The obvious place to check for long-term harm is in the lungs, because COVID-19 begins as a respiratory infection. Few peer-reviewed studies exploring lasting lung damage have been published. Gholamrezanezhad’s team analysed lung CT images of 919 patients from published studies, and found that the lower lobes of the lungs are the most frequently damaged. The scans were riddled with opaque patches that indicate inflammation, that might make it difficult to breathe during sustained exercise. Visible damage normally reduced after two weeks. An Austrian study also found that lung damage lessened with time: 88% of participants had visible damage 6 weeks after being discharged from hospital, but by 12 weeks, this number had fallen to 56% (see go.nature.com/3hiiopi).
- Symptoms might take a long time to fade; a study posted on the preprint server medRxiv in August followed up on people who had been hospitalized, and found that even a month after being discharged, more than 70% were reporting shortness of breath and 13.5% were still using oxygen at home.
Evidence from people infected with other coronaviruses suggests that the damage will linger for some. A study published in February recorded long-term lung harm from SARS, which is caused by SARS-CoV-1. Between 2003 and 2018, Peixun Zhang at Peking University People’s Hospital in Beijing and his colleagues tracked the health of 71 people who had been hospitalized with SARS. Even after 15 years, 4.6% still had visible lesions on their lungs, and 38% had reduced diffusion capacity, meaning that their lungs were poor at transferring oxygen into the blood and removing carbon dioxide from it. - Some people who have recovered from COVID-19 could be left with a weakened immune system. Many other viruses are thought to do this. “For a long time, it’s been suggested that people who have been infected with measles are immunosuppressed in an extended period and are vulnerable to other infections,” says Daniel Chertow, who studies emerging pathogens at the National Institutes of Health Clinical Center in Bethesda, Maryland. “I’m not saying that would be the case for COVID, I’m just saying there’s a lot we don’t know.” SARS, for instance, is known to decrease immune-system activity by reducing the production of signalling molecules called interferons.
- An over-reactive immune system can lead to inflammation, and one particularly susceptible organ is the heart. During the acute phase of COVID-19, about one-third of patients show cardiovascular symptoms, says Mao Chen, a cardiologist at Sichuan University in Chengdu, China. “It’s absolutely one of the short-term consequences.”
- One of the most insidious long-term effects of COVID-19 is its least understood: severe fatigue. Over the past nine months, an increasing number of people have reported crippling exhaustion and malaise after having the virus. Support groups on sites such as Facebook host thousands of members, who sometimes call themselves “long-haulers”. They struggle to get out of bed, or to work for more than a few minutes or hours at a time. One study of 143 people with COVID-19 discharged from a hospital in Rome found that 53% had reported fatigue and 43% had shortness of breath an average of 2 months after their symptoms started. A study of patients in China showed that 25% had abnormal lung function after 3 months, and that 16% were still fatigued.
The only way to find out whether SARS-CoV-2 is behind these symptoms is to compare people known to have had the virus with those who have not, says Chertow, to see how often fatigue manifests and in what form. Otherwise there is a risk of lumping together people whose fatigue has manifested for different reasons, and who might need distinct treatments.
Chertow says he is not aware of such a study for COVID-19, but they have been done for other diseases. Following the Ebola epidemic in West Africa in 2014–16, US researchers collaborated with the Ministry of Health in Liberia to perform a long-term follow-up study called Prevail III. The study identified six long-term impacts from Ebola, ranging from joint pain to memory loss. Bhadelia, who treated hundreds of people with Ebola during the outbreak, says that these post-viral symptoms had not previously been recognized. Usually, she says, “we don’t stick around past the acute stage. We don’t look at the long tail of recovery. It’s important to do that, because it tells you more about the virus and its pathophysiology.” - Once again, there is evidence from SARS that coronavirus infection can cause long-term fatigue. In 2011, Harvey Moldofsky and John Patcai at the University of Toronto in Canada described 22 people with SARS, all of whom remained unable to work 13–36 months after infection. Compared with matched controls, they had persistent fatigue, muscle pain, depression and disrupted sleep. Another study, published in 2009, tracked people with SARS for 4 years and found that 40% had chronic fatigue. Many were unemployed and had experienced social stigmatization.
It is not clear how viruses might do this damage, but a 2017 review of the literature on chronic fatigue syndrome found that many patients have persistent low-level inflammation, possibly triggered by infection.
“Even mild Covid is linked to brain damage, scans show” (March 7, 2022)
[edit]Benjamin Ryan, “Even mild Covid is linked to brain damage, scans show”, NBC News, (March 7, 2022)
- During at least the first few months following a coronavirus infection, even mild cases of Covid-19 are associated with subtle tissue damage and accelerated losses in brain regions tied to the sense of smell, as well as a small loss in the brain’s overall volume, a new British study finds. Having mild Covid is also associated with a cognitive function deficit.
These are the striking findings of the new study led by University of Oxford investigators, one that leading Covid researchers consider particularly important because it is the first study of the disease’s potential impact on the brain that is based on brain scans taken both before and after participants contracted the coronavirus.
“This study design overcomes some of the major limitations of most brain-related studies of Covid-19 to date, which rely on analysis and interpretation at a single time point in people who had Covid-19,” said Dr. Serena S. Spudich, a neurologist at the Yale University School of Medicine, who was not involved in the research. - Gwenaëlle Douaud, an associate professor at the Nuffield Department of Clinical Neurosciences at Oxford and the paper’s lead author, said that the excess loss of brain volume she and her colleagues observed in brain scans of hundreds of British individuals is equivalent to at least one extra year of normal aging.
“It is brain damage, but it is possible that it is reversible,” she said. “But it is still relatively scary because it was in mildly infected people.” - Dr. Avindra Nath, clinical director of the National Institute of Neurological Disorders and Stroke at the National Institutes of Health, said that these findings “have long-term implications, since we would be concerned about the possibility of similar cognitive dysfunction in a large population worldwide."
"It needs to be determined if these patients could further deteriorate over a period of time," he said. - “This study provides the most definitive clinical data available to date that SARS-CoV-2 directly or indirectly damages nerves and that this, in turn, can have systemic effects, including changes in the brain,” said Dr. Steven Deeks, a veteran HIV researcher at the University of California, San Francisco. “It contributes to an emerging theme that nerve damage was common during the first few waves of the pandemic.”
“Pregnancy and COVID: what the data say” (9/3/2021)
[edit]Nidhi Subbarman, “Pregnancy and COVID: what the data say”, Nature 591, (09 March 2021), pp. 193-195



- Yalda Afshar was about two months pregnant when reports of COVID-19 began to emerge in the United States in February last year. As an obstetrician managing high-risk pregnancies at the University of California, Los Angeles, Afshar knew that respiratory viruses are especially dangerous to pregnant women. There was very little data on the effects of the SARS-CoV-2 virus and, as cases racked up, she felt like she was flying blind, both while advising her patients and in navigating her own worries about contracting the virus and passing it on to her baby and family. But her situation also brought her closer to the women she was treating. “I had this sense of solidarity that I’ve not felt before,” she says. “It was an inspiration to just work harder and try to get answers faster.”
- [A] data void gapes around vaccination safety. Following established norms, none of the major vaccine makers enrolled pregnant women in its first trials, although some current and planned trials now include them. As health systems around the world began to churn out shots, regulators have offered conflicting or vague recommendations about whether pregnant women should be offered the jab. In January, the World Health Organization (WHO) recommended that the messenger RNA vaccines made by Moderna and Pfizer/BioNTech be offered only to pregnant women at highest risk — those working in frontline positions or with existing health conditions — and only after consultation with their physician. It later added clarifying language that said the vaccines posed no known specific risks in pregnancy. A WHO spokesperson told Nature that, because of the lack of data, the agency “could not provide a broad recommendation for vaccination of pregnant women”.
Overwhelmingly, physicians contacted by Nature say they would recommend that pregnant women be offered the vaccine after medical consultation. “Given what we know about the increased risk of hospitalization, mortality, preterm birth — for me, it’s a no-brainer,” says Kristina Adams Waldorf, an obstetrician and a researcher at the University of Washington in Seattle. - It’s no surprise that respiratory viruses pose a threat to pregnant women, whose lungs are already working harder than usual. As the uterus grows it pushes up against the diaphragm, reducing lung capacity and taxing an oxygen supply divided between mother and fetus. On top of that, pregnancy dials down the immune system so as not to harm the baby. That makes women more susceptible to complications from infection. Take influenza: pregnant women who catch it are at higher risk of hospitalization compared with women who are not pregnant. Pregnant women who caught the H1N1 flu during the 2009–10 pandemic were at higher risk of preterm delivery and stillbirth.
- The earliest data from China indicated that pregnant women didn’t fare much worse than non-pregnant women of the same age. But doctors were sceptical. “That didn’t really resonate that well with most maternal–fetal medicine physicians,” says Andrea Edlow, an obstetrician at the Vincent Center for Reproductive Biology at Massachusetts General Hospital in Boston. Besides, she says, everybody saw the signs in their patients: “Pregnant women were getting sicker than other women.”
A volley of reports from around the globe began filling in the picture. An analysis of 77 cohort studies published last September made clear that pregnant women are a high-risk group. The review included data from more than 11,400 women with confirmed or suspected COVID-19 and who were hospitalized during their pregnancy for any reason. The odds of pregnant women with a COVID-19 diagnosis being admitted to the intensive-care unit (ICU) were 62% higher than for non-pregnant women of reproductive age, and the odds of needing invasive ventilation were 88% higher. A study by the US Centers for Disease Control and Prevention (CDC) echoed these findings. The study included more than 400,000 women with a positive test and symptoms of COVID-19, of whom 23,434 were pregnant, and found similar increases in the odds of ICU admission and invasive ventilation in pregnant women (see ‘COVID risks in pregnancy’). - Health-care workers should be made aware that pregnant women are less likely than non-pregnant women to show symptoms of COVID-19, says Shakila Thangaratinam, a maternal and perinatal health researcher at the University of Birmingham, UK, who led the analysis of the 77 studies. But she acknowledged that the sample was restricted by including only women who were hospitalized for some reason, and that this could hide the scale of the problem. “I think we need to systematically start getting information on what’s happening in the community,” she says.
Pregnant women with COVID-19 had higher rates of preterm delivery than did those without the disease, according to data from two registries that tracked more than 4,000 women with confirmed or suspected COVID-19 in the United States and the United Kingdom6. Twelve per cent of participants in the UK registry delivered before 37 weeks, compared with the rate for 2020 of 7.5% across England and Wales; in the United States, 15.7% of women with COVID-19 experienced preterm birth (the expected national rate is 10%). According to Thangaratinam’s analysis4, pregnant women with COVID-19 had three times the odds of delivering preterm compared with those without the disease. - Reassuringly, COVID-19 has so far not been linked to a clear increase in rates of stillbirth or stalled fetal growth. “We can be relatively reassuring, because if we’re worried about stillbirth or growth restriction, that is not any more likely,” says Christoph Lees, an obstetrician at Imperial College London, who was part of the team that compared registry data for 4,000 women in the United States and the United Kingdom.
- One big unknown early in the pandemic was whether SARS-CoV-2 could transmit from mother to baby. Edlow, keen to find out, pivoted her team from studies of maternal obesity in mice to building a registry of pregnant patients and a repository for biological samples. As non-essential laboratories around them closed, other medical researchers donated equipment and reagents, and Edlow’s team began collecting and studying maternal plasma, cord plasma and placentae.
Studies published from her group last December joined a chorus of data that showed that this ‘vertical transmission’ was rare. In 62 pregnant women who tested positive for SARS-CoV-2 by way of a nose or throat swab, Edlow’s team found no evidence of virus in the blood or cord blood, and none of the 48 babies that were swabbed tested positive for the virus at birth. “It’s a lucky asset of SARS-CoV-2 that we don’t get neonates getting really sick and dying,” Edlow says.
Afshar’s team also found that babies born to infected mothers generally fared well. In a study8 that compared 179 babies born to women who had tested positive for SARS-CoV-2 with 84 born to mothers who tested negative, most babies were healthy at birth and for 6–8 weeks after.
The question of whether a mother’s immunity transfers to her baby is a little more complicated. Edlow’s team and others have found antibodies to SARS-CoV-2 in the umbilical-cord blood of women who had been infected, but it is not yet clear how much protection those levels confer on the fetus, Edlow says. - Severe viral infections in mothers have been linked to an increased chance of depression and autism spectrum disorder in their children11, and researchers wondered whether SARS-CoV-2 could also have this effect. There is no evidence yet that SARS-CoV-2 infection in mothers can affect their babies in this way, and any such links could take years to establish, but some researchers are watching their cohorts for any delays to neurological development; Afshar’s team will be tracking babies in their first year following birth.
In rare cases, the placenta can be a key player in disease, says David Baud, an obstetrician at the University of Lausanne in Switzerland who is studying a group of 1,700 pregnant women from across the world, using the architecture of a registry his team had developed to study the Zika virus in 2009. - All of this convinces most physicians that pregnant women must be prioritized for COVID-19 vaccines. But because the early vaccine trials excluded pregnant women, there are unanswered questions about the safety of vaccines in this group. “I think that it was a huge mistake to not include them, because now essentially everyone is a guinea pig,” says Adams Waldorf.
- Researchers and advocacy groups want to use the COVID-19 example to change the standards of future clinical trials, and include pregnant women from the start. The leaders of the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Maryland, part of the US National Institutes of Health, argued12 in February that “pregnant and lactating persons should not be protected from participating in research, but rather should be protected through research”.
The concern that this group will be forgotten is what motivated Afshar to kick-start her collaboration in the first place. “Pregnant people are seriously marginalized from studies. And if we’re not doing the research to answer these questions, no one else is.”
Demography
[edit]“A guide to R — the pandemic’s misunderstood metric” (03/7/2020)
[edit]David Adam, “A guide to R — the pandemic’s misunderstood metric”, Nature, (03 July 2020), 583, pp.346-348


- Mathematicians and public-health experts watched through their fingers in May as British Prime Minister Boris Johnson unveiled a series of charts to explain how the government would guide Britain out of coronavirus lockdown. Perhaps most prominent was a colourful dial with a needle hovering near a single digit: 1.
The dial indicated R, a now-totemic figure in the COVID-19 pandemic. The nation, said Johnson, would set a COVID-19 alert level, to be "primarily determined" by the number of coronavirus cases, and by R, the reproduction number.
To infectious-disease experts, Johnson’s focus on the reproduction number as a guiding light for policy was worryingly myopic. They worry about placing too much weight on R, the average number of people each person with a disease goes on to infect. - R is an imprecise estimate that rests on assumptions, says Jeremy Rossman, a virologist at the University of Kent, UK. It doesn’t capture the current status of an epidemic and can spike up and down when case numbers are low. It is also an average for a population and therefore can hide local variation. Too much attention to it could obscure the importance of other measures, such as trends in numbers of new infections, deaths and hospital admissions, and cohort surveys to see how many people in a population currently have the disease, or have already had it.
“Epidemiologists are quite keen on downplaying R, but the politicians seem to have embraced it with enthusiasm,” says Mark Woolhouse, an infectious-diseases expert at the University of Edinburgh in the United Kingdom, who is a member of a modelling group that advises the British government on the pandemic. “We’re concerned that we’ve created a monster. R does not tell us what we need to know to manage this.” - First used almost a century ago in demography, R originally measured the reproduction of people — whether a population was growing or not. In epidemiology, the same principle applies, but it measures the spread of infection in a population. If R is two, two infected people will, on average, infect four others, who will infect eight others, and so on. The measure allows modellers to work out the extent of the spread, but not the speed at which the infection grows.
Unless they regularly test an entire country’s population, epidemiologists can’t measure R directly. So it is usually estimated retrospectively: disease modellers look at current and previous numbers of cases and deaths, make some assumptions to find infection numbers that could have explained the trend and then derive R from these.
One variant of R, R0, assumes that everybody in a population is susceptible to infection. That usually isn’t true, but might be when a new virus, such as SARS-CoV-2, emerges. At the start of the epidemic, assessing R0 (and other metrics) was crucial for epidemiologists building models of how the disease might spread. But when politicians and scientists talk about R, they usually mean another variant called Rt (sometimes called Re, or ‘effective R’), which is calculated over time as an outbreak progresses and considers how some people might have gained immunity, perhaps because they have survived infection or been vaccinated.
Rt and R0 both vary with the social dynamics of a population: even an easily transmitted virus will have trouble spreading in a region where people rarely meet. In January, the COVID-19 R0 in Wuhan, China, was calculated to be between two and three; after lockdown, estimates put the Rt there at just over one. - Working out Rt involves trade-offs and compromise. Confirmed cases and mortality figures can be used to infer the total number of infections, but both come with a significant lag — which scientists estimate could be anything from a week to three weeks or more. “If you have your Rt estimate lagging by at least ten days, possibly two weeks, then it’s not going to be that useful as a real-time decision-making tool,” says Gabriel Leung, a public-health scientist at the University of Hong Kong.
With a mathematical trick called nowcasting, researchers can use the observed statistical distribution of reporting delays to predict how much higher the number of fresh infections will be in, for example, two weeks. Some estimates of Rt already rely on nowcasting infection data in this way: it is "the method with the least guesses", says Lars Schaade, vice-president of the Robert Koch Institute in Berlin, Germany’s main public-health agency, which reports a daily and seven-day Rt value based on infections reported by state health authorities. - Even non-experts can use plug-and-play formulas to create their own variants of R — which can sometimes lead to problems. In May, local newspapers across England ran stories claiming to reveal regional Rt values for specific towns and cities. The Swindon Advertiser claimed the town’s Rt was 0.35, perhaps “one of the lowest in UK”. But officials at Brighton and Hove City Council (labelled with the fourth-highest Rt, at 1.7) issued a statement calling the figures misleading and potentially dangerous. “It is not possible to calculate meaningful R values at a very local level,” said Alistair Hill, a public-health official on the council.
The figures were not, it turned out, Rt values at all: they came from an index created by the founders of a London-based analytics start-up called deckzero.com. That index, termed RZ, was intended to show how fast local epidemics were growing on the basis of case data from local authorities; it is not an established variable in epidemiology, says Jenna Wang, a co-founder and director of the firm. On 7 June, the founders withdrew their page from public access and said it had been “interpreted out of the context and scope of its original intention”. - An important aspect of Rt is that it represents only an average across a region. This average can miss regional clusters of infection. Conversely, high incidences of infection among a spatially distinct smaller subsection of a population can sway a larger region’s Rt value. For instance, Germany’s national Rt value jumped from just over 1 to 2.88 in late June (later revised down to 2.17) largely because of an outbreak in a meat-processing plant at Gütersloh in North Rhine-Westphalia (see 'Germany's Regional Outbreaks'). The Robert Koch Institute noted that national infections overall were still low, which is why the local outbreak had such an effect on the country’s Rt, which had dropped below 1 again by the end of June. This makes it unlikely that Rt would be used to steer local lockdown policy in Germany, Schaade says. “If the rolling mean of R was at 1.2 for a few weeks, then that would show there was a problem that needed attention, even if case numbers were low.” But in practice, researchers find out about local outbreaks before that because of a reported spike in cases, not because of changes to Rt. Germany has ongoing surveillance and public reporting of transmission levels in 400 counties.
- [M]ost experts say that the Rt for the United Kingdom is kept artificially high by the very large numbers of infections and deaths in care homes for older people, and does not reliably represent the risk to the general population.
Regional Rt numbers have been touted as a way to guide the further easing of restrictions, because they could allow a place that showed a resurgence in cases to be sealed off. But regional Rt numbers become less accurate as they are applied to smaller populations, especially when absolute infections are low.
The Harvard site produces numbers for US counties — which can range from thousands to millions of inhabitants — but one of its creators, Xihong Lin, says that hyperlocal data come with big uncertainties. The researchers don’t calculate an Rt for a county unless there are ten cases, Lin says. And she stresses that policymakers should not use them in isolation, but only alongside other measures such as the total number of cases and whether it is increasing. “When making recommendations. it’s definitely important to look at the whole picture and not just rely on Rt,” she says. Used properly, the data could help public-health officials to identify hot spots of infection to prioritize resources such as testing, she says. - Another subtlety not captured by Rt is that many people never infect others, but a few 'superspreaders' pass on the disease many more times than average, perhaps because they mingle in crowded, indoor events where the virus spreads more easily — church services, choir practices, nightclubs and birthday parties, for instance. As few as 10–20% of infected people seem to cause 80% of new COVID-19 cases, Leung says. (Epidemiologists describe this using a ‘dispersion’ parameter, k’, which depicts the variation in viral transmission among infected hosts). That means bans on certain crowded indoor activities could have more benefit than blanket restrictions introduced whenever the Rt value hits one.
“A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes” (August 01, 2020)
[edit]Rabail Chaudhry, George Dranitsaris, Talha Mubashir, Justyna Bartoszko, Sheila Riazi; “A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes”, The Lancet, Volume 25, (August 01, 2020)
- Increasing COVID-19 caseloads were associated with countries with higher obesity (adjusted rate ratio [RR]=1.06; 95%CI: 1.01–1.11), median population age (RR=1.10; 95%CI: 1.05–1.15) and longer time to border closures from the first reported case (RR=1.04; 95%CI: 1.01–1.08). Increased mortality per million was significantly associated with higher obesity prevalence (RR=1.12; 95%CI: 1.06–1.19) and per capita gross domestic product (GDP) (RR=1.03; 95%CI: 1.00–1.06). Reduced income dispersion reduced mortality (RR=0.88; 95%CI: 0.83–0.93) and the number of critical cases (RR=0.92; 95% CI: 0.87–0.97). Rapid border closures, full lockdowns, and wide-spread testing were not associated with COVID-19 mortality per million people. However, full lockdowns (RR=2.47: 95%CI: 1.08–5.64) and reduced country vulnerability to biological threats (i.e. high scores on the global health security scale for risk environment) (RR=1.55; 95%CI: 1.13–2.12) were significantly associated with increased patient recovery rates.
- In a matter of weeks after the World Health Organization (WHO) declaring a global pandemic for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), over 100 countries implemented varied levels of containment in order to reduce disease transmission. Some evidence suggested that strict social distancing measures and other interventions may limit spread of this novel pathogen, originating from individual countries or from jurisdictions within countries. To our knowledge, no published articles have used a country-level analysis, pooling data across multiple countries, to report the impact of population health interventions, country-specific socioeconomic factors, and healthcare capacity on overall COVID-19 cases (recovered or critical), and associated mortality.
- At present, public health policies across countries have varied considerably with respect to the restrictiveness of interventions, the acceptance of widespread implementation, and presumed effectiveness in reducing disease transmission. Measures such as the detection and isolation of infected individuals, contact-tracing, quarantine measures, physical distancing, and closure of non-essential businesses have become major components of public health guidance, aiming to reduce the spread of further infection, and prevent health system strain. Although containment measures implemented in countries like China, South Korea, and Taiwan have reduced new cases by more than 90%, this has not been the case in many other countries such as Italy, Spain, and the United States. Despite appropriate public health guidance, less than optimal population compliance in western democracies may be an important contributing factor to variation in outcomes among the various countries. In addition, the timing of implementation of public health measures, pre-existing socioeconomic characteristics of the country, baseline healthcare capacity, and other health-related population features (i.e. smoking prevalence, obesity rate, and global health indices) may be contributing factors to disparities in outcomes between countries.
- Among the 50 countries included in the analysis, 38 (76%) had a complete border closures, while 10 (20%) had only partial border closures by April 01, 2020. The median time to any border closure from the first reported case in China was 78 days (77, 80), or 23 days (18, 44) from the first case in each country. Of the 50 countries, 40 (80%) had implemented a complete lockdown by the reference date (May 01, 2020), while a partial lockdown or a curfew was applied by 5 (10%) countries. The median time to any lockdown from first reported case in China or from first case in the reference country was 77.5 days (76, 81) and 23 days (19, 32), respectively (Table 2).
- The findings of the multivariable regression analyses to identify factors associated with COVID-19 total case rates and recovered cases (per million) are presented in Table 3. Predictors significantly associated with the total number of reported cases per million were days to any lockdown (i.e. full or partial), median age of population, prevalence of obesity, days to any border closure and number of tests performed per million population (Table 3). There was a negative association between the number of days to any lockdown (RR=0.94; 95%CI:0.91–0.98) and the total number of reported cases per million, where a longer time prior to implementation of any lockdown was associated with a lower number of detected cases per million. In contrast, those countries with a higher median population age (RR=1.10; 95%CI:1.05–1.15), prevalence of obesity (RR=1.06; 95%CI:1.01–1.11) and a longer number of days to any border closure (RR=1.04; 95%CI 1.01–1.08) had significantly higher caseloads. When the analysis was continued on the outcome variable ‘recovered cases per million’; a full lockdown (versus partial/curfew only; RR=2.47; 95%CI:1.08–5.64); and a higher GHS risk environment (RR=1.55; 95%CI:1.13–2.12) were positively associated with an increased number of recovered cases (Table 3).
- The next series of analyses focused on the number of critical cases and deaths per million. Socioeconomic variables positively associated with an increased number of critical cases per million for any given country were: a higher percent unemployment rate (RR=1.18; 95%CI:1.07–1.30) and per capita GDP (RR=1.02; 95%CI 1.01–1.4). In contrast, lower income dispersion scores (RR=0.92; 95%CI:0.87–0.97) and a higher prevalence of smoking within a population (RR=0.96; 95%CI:0.93–0.99) were associated with a reduction in the number of critical cases (Table 4).
- When COVID-19 mortality was assessed, variables significantly associated with an increased death rate per million were population prevalence of obesity and per capita GDP (Table 4). In contrast, variables that was negatively associated with increased COVID-19 mortality were reduced income dispersion within the nation, smoking prevalence, and the number of nurses per million population (Table 4). Indeed, more nurses within a given health care system was associated with reduced mortality (Fig. 1). Mortality rates were also higher in those counties with an older population upon univariate analysis, but age as a factor was not retained in multivariable analysis (Fig. 2). Lastly, government actions such as border closures, full lockdowns, and a high rate of COVID-19 testing were not associated with statistically significant reductions in the number of critical cases or overall mortality.
- An exploratory country level analysis using publicly available sources of data was conducted to examine factors associated with COVID-19 related health outcomes. Predictors evaluated consisted of government policies/actions for COVID-19 containment, scale of testing, country specific socioeconomic parameters, health care capacity, degree of preparedness, and population comorbidities. Consistent with reported COVID-19 outcome data from Europe, the United States, and China, higher caseloads and overall mortality were associated with comorbidities such as obesity, and advanced population age. In contrast, a lower income dispersion within the nation reduced overall mortality and critical cases. Of all the GHS subscales evaluated, the index for risk environment had the most profound association with recovered cases per million. Countries that were the least vulnerable to biological threats (as indicated by higher scores) had the highest number of recovered cases. Indeed, for every ten-unit increase in the GHS score for risk environment, the relative rate of recovered cases increased by 55%.
There were a series of predictors with significant associations with the outcome variables that require careful interpretation. An increased scale of national testing was not associated with the number of critical cases, or deaths per million. The government policy of full lockdowns (vs. partial or curfews only) was strongly associated with recovery rates (RR=2.47; 95%CI: 1.08–5.64). Similarly, the number of days to any border closure was associated with the number of cases per million (RR=1.04; 95%CI: 1.01–1.08). This suggests that full lockdowns and early border closures may lessen the peak of transmission, and thus prevent health system overcapacity, which would facilitate increased recovery rates.
The final two variables significantly associated to poorer outcomes were per capita GDP and smoking prevalence. Countries with a higher per capita GDP had an increased number of reported critical cases and deaths per million population. This may reflect more widespread testing in those countries, greater transparency with reporting and better national surveillance systems. Other potential putative reasons for the association might include increase accessibility to air travel and international holidays in wealthier countries, as travel was identified as an important factor contributing to international viral spread. The final unexpected finding was the lower frequency of critical cases and deaths in countries with a higher smoking prevalence. This finding requires further investigation, as the literature is inconsistent. However, there was an interesting observation from a recently published paper describing 393 critical patients with COVID-19 admitted to two hospitals in New York City. The analysis revealed that only 5.1% of the patient sample were current smokers, compared to the 15.6% smoking incidence in United States reported by the CDC. The finding of relatively lower smoking rates amongst critical ill COVID-19 patients is due in part due to their increased age distribution, since countries with a lower median age have higher smoking rates. Hence, the potentially lower median age amongst countries with higher smoking prevalence in our model may be driving the observed association of low COVID-19 critical cases and deaths with high smoking prevalence. A potential protective effect of smoking was identified in a recent evaluation of 17 million adult patients within the National Health Service of the United Kingdom, with 5683 COVID related deaths. In their analysis, current smokers were associated with a reduced risk of COVID-19 related mortality (adjusted HR = 0.88; 95%CI: 0.79–0.99). Notwithstanding these findings, more study is needed. - There are important limitations with our data, including the fact that at or prior to May 1, 2020, many countries included in our dataset were not yet in the “plateau” or downslope phase of their individual epidemiologic curves, with border restrictions having been introduced only very recently. In the context of COVID-19, it is thought that public health interventions typically require from 2 to 3 weeks to affect outcomes, hence the impact of widespread border restrictions may not have yet been detected in our dataset. Additionally, the relative difference in the number of cases in neighboring countries is likely to have a significant impact on whether border closures are effective. Two countries with similar epidemiologic curves and effective social distancing policies may not see a major impact from border closures, whereas two countries with very disparate epidemiologic curves may be more likely to see a significant impact from travel restrictions. In the case of full lockdowns, such a government policy may only be effective in those countries where it can be easily implemented and enforced. For example, the United States has had challenges enforcing lockdowns, with citizens in several states publicly protesting public health measures to limit viral transmission, and encouraging open revolt.
- The findings of this country level analysis on COVID-19 related health outcomes suggest that low levels of national preparedness, scale of testing, as well as population characteristics such as obesity, advanced age and higher per capita GDP are associated with increased national case load and mortality.
“How many people has the coronavirus killed?” (1/9/2020)
[edit]Guiliana Viglione, “How many people has the coronavirus killed?”, Nature, (01 September 2020), 585, pp.22-24
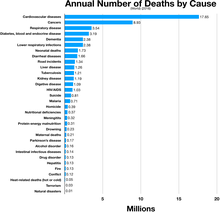


- At the beginning of March, Andrew Noymer felt a familiar twinge of doubt. He was watching countries across Europe and North America begin to record their first deaths from COVID-19, and he knew there could be problems with the data. Even in a normal winter, some deaths caused by influenza get misclassified as pneumonia. If that can happen with a well-known disease, there were bound to be deaths from COVID-19 going unreported, thought Noymer, a demographer at the University of California, Irvine. “I just remember thinking, ‘this is going to be really difficult to explain to people’,” he recalls.
And in March and April, when national statistics offices began to release tallies of the number of deaths, it confirmed his suspicions: the pandemic was killing a lot more people than the COVID-19 figures alone would suggest. - In times of upheaval — wars, natural disasters, outbreaks of disease — researchers need to tally deaths rapidly, and usually turn to a blunt but reliable metric: excess mortality. It’s a comparison of expected deaths with ones that actually happened, and, to many scientists, it’s the most robust way to gauge the impact of the pandemic. It can help epidemiologists to draw comparisons between countries, and, because it can be calculated quickly, it can identify COVID-19 hotspots that would otherwise have gone undetected. According to data from more than 30 countries for which estimates of excess deaths are available (see ‘Terrible toll’), there were nearly 600,000 more deaths than would normally be predicted in these nations for the period between the onset of the pandemic and the end of July (413,041 of those were officially attributed to COVID-19).
But this high-level metric has several flaws. It cannot distinguish between those who are dying of the disease and those who succumb to other factors related to the pandemic, such as disruptions to regular health care, which can delay treatments or mean that people do not seek medical care. It relies on accurate, timely reporting of deaths, which can be limited owing to underdeveloped death-registration systems, or might even be intentionally suppressed. And as with so many other aspects of the pandemic, the statistic has become politicized — a way for countries to claim superiority over one another. - Experts worry that simple reports of excess deaths have led to premature or faulty comparisons of countries’ pandemic responses, and have largely ignored the situation in low- and middle-income countries owing to a lack of data.
There are more sophisticated ways to categorize mortality to find out how many people were killed as a direct result of infection with SARS-CoV-2, and how many deaths happened because of other factors associated with the pandemic. Eventually, demographers and public-health researchers will have enough granular information from death certificates to do this. They will then be able to assess which interventions worked best, to inform future pandemic responses.
Several media outlets are already crunching the data and drawing such conclusions. Some statisticians argue that, as the first wave of the pandemic recedes in many places, comparisons can — and should — be made between government policies to see how they might have affected mortality. But many experts say that it’s still too early in the pandemic to do this with rigour. The process can be skewed by the random way that some early outbreaks spread and others fizzle out, making analysis complicated until the pandemic has run its course, says Jennifer Dowd, a demographer and epidemiologist at the University of Oxford, UK. “It’s going to be a very long road.” - When deaths began creeping up in Europe, Lasse Vestergaard was one of the first to notice. Vestergaard, an epidemiologist at the Statens Serum Institut in Copenhagen, leads the European Mortality Monitoring Project (EuroMOMO), which aggregates weekly all-cause death data from 24 European countries or regions. Between March and April, EuroMOMO’s tracker showed tens of thousands more deaths than expected — about 25% higher than the official COVID-19 deaths figure. Infections were slipping under the radar because of a lack of testing, and because different countries counted deaths in different ways — excluding deaths occurring in care homes, for instance. It was nearly impossible to get a true sense of how countries were faring.
- The Nature analysis shows that there are huge variations in excess deaths between countries (see ‘More than expected’). In the United States and Spain — two of the hardest-hit countries so far — about 25% and 35%, respectively, of the excess death toll is not reflected in official COVID-19 death statistics. But in other places, the mismatch is much greater, such as in Peru, where 74% of the excess deaths are not explained by reported COVID-19 deaths. And some countries, such as Bulgaria, have even experienced negative excess deaths during the pandemic so far — meaning that, despite the virus, fewer people have died this year than expected.
- Direct deaths feature on pandemic trackers showing numbers of cases and deaths, which are generally updated daily by local and national health authorities. But even this count isn’t as clear-cut as it might seem, warns Maimuna Majumder, a computational epidemiologist at Harvard Medical School in Boston, Massachusetts.
It can be challenging to differentiate between people who died of COVID-19 and those who were infected but died from unrelated causes. “That’s going to be a very critical piece of all this,” she says. “If you have two concurrent conditions, what does it get classified as?” Parsing those deaths, Majumder says, will require a death-classification system that accounts for the underlying conditions that make COVID-19 more likely to kill. Such a system would mean waiting for cause-of-death data, which take around a year to compile in full. - Then there are the direct-but-uncounted deaths — those that were missed because the individual presented with symptoms not recognized as COVID-19. “We’re still figuring out exactly how the disease manifests,” says Natalie Dean, a biostatistician at the University of Florida in Gainesville. Strokes and pulmonary embolisms are two potentially deadly complications of the virus that might have been overlooked initially, she says.
- Visits to emergency departments in the United States declined by more than 40% in the early days of the pandemic, according to a report from the Centers for Disease Control and Prevention (CDC), suggesting that many people were reluctant to attend (K. P. Hartnett et al. Morb. Mortal. Wkly Rep. 69, 699–704; 2020). And even if they did seek care, hospitals were severely overstretched, Majumder says. “You died from something else, but the reason you died from something else is because the systems that were initially in place to take care of you are no longer strong enough.” Preliminary, incomplete data from the CDC offer a glimpse of these indirect deaths: in April, US recorded deaths from diabetes were 20–45% higher than the 5-year average; deaths from ischaemic heart disease were anywhere from 6% to 29% higher than the norm.
- Demographers will probably never know the pandemic’s final toll with certainty, Noymer says. “You don’t get to scratch off the lottery ticket and find out the actual values underneath the grey plastic coating.” Once the pandemic subsides, disentangling the three types of death — and determining how many would have occurred in the absence of the virus — will be a process that will take months or even years. “We haven’t even settled on how many people died in the 1918 flu,” he says. “And we’ve had 100 years to sort out the numbers.”
Right now, statistics on excess deaths are helping to chart the path of the outbreak in different places. In the future, with full cause-of-death data, researchers will be able to analyse the impacts of lockdowns and other interventions by looking at the levels of direct and indirect deaths from country to country. But it’s risky to do that now, says Noymer, while the pandemic rages on and the final toll is unknown. “We just don’t have much perspective yet, because we’re still in the rising tide,” he says. “It’s like trying to predict rainfall totals in the middle of a hurricane.”
Even after the storm, these analyses will be possible only in high-income countries with robust systems that register births and deaths — known as civil registration and vital statistics (CRVS). In low- and middle-income countries, counting deaths is much less straightforward, says Irina Dincu, a programme specialist in CRVS at the International Development Research Centre in Ottawa. “Across the world, about 50% of the deaths occurring in a given year are registered,” she says. “The other 50% do not exist at all. They are invisible.” - For some demographers, it doesn’t necessarily matter whether someone died of the disease itself or because the health-care system was stretched beyond its capacity — all of the deaths can be attributed, in some way, to the pandemic. “At some point you have to say, ‘well that’s COVID-related, somehow, because COVID disrupted the health-care system’,” says Noymer. “To me, the thought experiment is, ‘what does 2020 look like if this thing had never, ever happened?’”
Other researchers are keen to separate deaths caused by the virus from those resulting from circumstance, so that they can build an accurate picture of how lethal the virus itself actually is.
But there’s little time for such analyses right now. The pandemic has drastically increased the strain on death-registration systems as well as the scrutiny they face. Politicians, the media and the public are demanding daily or weekly statistics that would usually take months to compile. That makes some demographers uneasy. “We understand mortality best in retrospect,” Noymer says, because of the time and labour required to compile and analyse death certificates. “Everyone all of a sudden wants to know about it in real time.”
Hygiene
[edit]Masks
[edit]- CDC recommends a combination of evidence-based strategies to reduce transmission of SARS-CoV-2, the virus that causes COVID-19 (1). Because the virus is transmitted predominantly by inhaling respiratory droplets from infected persons, universal mask use can help reduce transmission (1). Starting in April, 39 states and the District of Columbia (DC) issued mask mandates in 2020. Reducing person-to-person interactions by avoiding nonessential shared spaces, such as restaurants, where interactions are typically unmasked and physical distancing (≥6 ft) is difficult to maintain, can also decrease transmission (2). In March and April 2020, 49 states and DC prohibited any on-premises dining at restaurants, but by mid-June, all states and DC had lifted these restrictions. To examine the association of state-issued mask mandates and allowing on-premises restaurant dining with COVID-19 cases and deaths during March 1–December 31, 2020, county-level data on mask mandates and restaurant reopenings were compared with county-level changes in COVID-19 case and death growth rates relative to the mandate implementation and reopening dates. Mask mandates were associated with decreases in daily COVID-19 case and death growth rates 1–20, 21–40, 41–60, 61–80, and 81–100 days after implementation. Allowing any on-premises dining at restaurants was associated with increases in daily COVID-19 case growth rates 41–60, 61–80, and 81–100 days after reopening, and increases in daily COVID-19 death growth rates 61–80 and 81–100 days after reopening. Implementing mask mandates was associated with reduced SARS-CoV-2 transmission, whereas reopening restaurants for on-premises dining was associated with increased transmission. Policies that require universal mask use and restrict any on-premises restaurant dining are important components of a comprehensive strategy to reduce exposure to and transmission of SARS-CoV-2 (1). Such efforts are increasingly important given the emergence of highly transmissible SARS-CoV-2 variants in the United States (3,4).
- Gery P. Guy Jr., PhD; Florence C. Lee, MPH1; Gregory Sunshine, JD; Russell McCord, JD; Mara Howard-Williams, JD; Lyudmyla Kompaniyets, PhD; Christopher Dunphy, PhD; Maxim Gakh, JD; Regen Weber; Erin Sauber-Schatz, PhD; John D. Omura, MD; Greta M. Massetti, PhD; CDC COVID-19 Response Team, Mitigation Policy Analysis Unit; CDC Public Health Law Program; “Association of State-Issued Mask Mandates and Allowing On-Premises Restaurant Dining with County-Level COVID-19 Case and Death Growth Rates — United States, March 1–December 31, 2020”, (March 5, 2021)

- Here is how the fibers of a cotton mask compare with aerosol particles of different sizes. The coronavirus is about the size of the smallest particles, but it usually travels inside the larger ones.
The fibers present a dense forest that the particles must navigate as they move with the air stream. The laws of physics influence how the particles interact with the fibers and how well the mask can capture them.
Larger particles are easier to trap. They slam straight into the fibers and get stuck when the air stream brings them within touching distance, or when their momentum causes them to veer off course.
The smallest particles are bounced around by air molecules in a random zig-zag pattern, increasing the time they spend in the fiber forest and their chances of getting captured.
Medium-size particles are the hardest to filter. They evade capture because they follow the air flow, twisting and turning around the fibers.- Or Fleisher, Gabriel Gianordoli, Yuliya Parshina-Kottas, Karthik Patanjali, Miles Peyton and Bedel Saget; “Masks Work. Really. We’ll Show You How”, “New York Times”, (Oct. 30, 2020)

- Loose-fitting masks or those pressed against facial hair allow aerosols to leak.
A good mask will have a large surface area, a tight fit around the edges, and a shape that leaves space around your nostrils and mouth.
This creates a larger breathing zone to catch the particles and increases the chance they will encounter a fiber.
Some masks have valves that make it easier to exhale, but without filters, these valves do not trap the aerosols you breathe out, so they do little to protect others.- Or Fleisher, Gabriel Gianordoli, Yuliya Parshina-Kottas, Karthik Patanjali, Miles Peyton and Bedel Saget; “Masks Work. Really. We’ll Show You How”, “New York Times”, (Oct. 30, 2020)

- “It’s become clear that cloth masks, even though they’re not as effective as the N95s, are still effective at reducing transmission,” said Linsey Marr, an aerosol expert at Virginia Tech. “Even if you’re not achieving that 95 percent reduction, something is better than nothing.”
- Linsey Marr as quoted in “Masks Work. Really. We’ll Show You How”, Or Fleisher, Gabriel Gianordoli, Yuliya Parshina-Kottas, Karthik Patanjali, Miles Peyton and Bedel Saget; “New York Times”, (Oct. 30, 2020)
“Face masks: what the data say” (6/10/2020)
[edit]Lynne Peeples, “Face masks: what the data say”, Nature, (06 October 2020), 586, pp.186-189

“I said, ‘Yeah, that might be good, but there’s limited data on whether face masks are actually effective.’

- When her Danish colleagues first suggested distributing protective cloth face masks to people in Guinea-Bissau to stem the spread of the coronavirus, Christine Benn wasn’t so sure.
“I said, ‘Yeah, that might be good, but there’s limited data on whether face masks are actually effective,’” says Benn, a global-health researcher at the University of Southern Denmark in Copenhagen, who for decades has co-led public-health campaigns in the West African country, one of the world’s poorest.
That was in March. But by July, Benn and her team had worked out how to possibly provide some needed data on masks, and hopefully help people in Guinea-Bissau. They distributed thousands of locally produced cloth face coverings to people as part of a randomized controlled trial that might be the world’s largest test of masks’ effectiveness against the spread of COVID-19. - At the beginning of the pandemic, medical experts lacked good evidence on how SARS-CoV-2 spreads, and they didn’t know enough to make strong public-health recommendations about masks.
The standard mask for use in health-care settings is the N95 respirator, which is designed to protect the wearer by filtering out 95% of airborne particles that measure 0.3 micrometres (µm) and larger. As the pandemic ramped up, these respirators quickly fell into short supply. That raised the now contentious question: should members of the public bother wearing basic surgical masks or cloth masks? If so, under what conditions? “Those are the things we normally [sort out] in clinical trials,” says Kate Grabowski, an infectious-disease epidemiologist at Johns Hopkins School of Medicine in Baltimore, Maryland. “But we just didn’t have time for that.” - Confidence in masks grew in June with news about two hair stylists in Missouri who tested positive for COVID-191. Both wore a double-layered cotton face covering or surgical mask while working. And although they passed on the infection to members of their households, their clients seem to have been spared (more than half reportedly declined free tests). Other hints of effectiveness emerged from mass gatherings. At Black Lives Matter protests in US cities, most attendees wore masks. The events did not seem to trigger spikes in infections2, yet the virus ran rampant in late June at a Georgia summer camp, where children who attended were not required to wear face coverings3. Caveats abound: the protests were outdoors, which poses a lower risk of COVID-19 spread, whereas the campers shared cabins at night, for example. And because many non-protesters stayed in their homes during the gatherings, that might have reduced virus transmission in the community. Nevertheless, the anecdotal evidence “builds up the picture”, says Theo Vos, a health-policy researcher at the University of Washington in Seattle.
- More-rigorous analyses added direct evidence. A preprint study posted in early August (and not yet peer reviewed), found that weekly increases in per-capita mortality were four times lower in places where masks were the norm or recommended by the government, compared with other regions. Researchers looked at 200 countries, including Mongolia, which adopted mask use in January and, as of May, had recorded no deaths related to COVID-19. Another study looked at the effects of US state-government mandates for mask use in April and May. Researchers estimated that those reduced the growth of COVID-19 cases by up to 2 percentage points per day. They cautiously suggest that mandates might have averted as many as 450,000 cases, after controlling for other mitigation measures, such as physical distancing.
“You don’t have to do much math to say this is obviously a good idea,” says Jeremy Howard, a research scientist at the University of San Francisco in California, who is part of a team that reviewed the evidence for wearing face masks in a preprint article that has been widely circulated. - Although scientists can’t control many confounding variables in human populations, they can in animal studies. Researchers led by microbiologist Kwok-Yung Yuen at the University of Hong Kong housed infected and healthy hamsters in adjoining cages, with surgical-mask partitions separating some of the animals. Without a barrier, about two-thirds of the uninfected animals caught SARS-CoV-2, according to the paper published in May. But only about 25% of the animals protected by mask material got infected, and those that did were less sick than their mask-free neighbours (as measured by clinical scores and tissue changes).
The findings provide justification for the emerging consensus that mask use protects the wearer as well as other people. The work also points to another potentially game-changing idea: “Masking may not only protect you from infection but also from severe illness,” says Monica Gandhi, an infectious-disease physician at the University of California, San Francisco. - The virus itself is only about 0.1 µm in diameter. But because viruses don’t leave the body on their own, a mask doesn’t need to block particles that small to be effective. More relevant are the pathogen-transporting droplets and aerosols, which range from about 0.2 µm to hundreds of micrometres across. (An average human hair has a diameter of about 80 µm.) The majority are 1–10 µm in diameter and can linger in the air a long time, says Jose-Luis Jimenez, an environmental chemist at the University of Colorado Boulder. “That is where the action is.”
Scientists are still unsure which size of particle is most important in COVID-19 transmission. Some can’t even agree on the cut-off that should define aerosols. For the same reasons, scientists still don’t know the major form of transmission for influenza, which has been studied for much longer. - In a review of observational studies, an international research team estimates that surgical and comparable cloth masks are 67% effective in protecting the wearer.
In unpublished work, Linsey Marr, an environmental engineer at Virginia Tech in Blacksburg, and her colleagues found that even a cotton T-shirt can block half of inhaled aerosols and almost 80% of exhaled aerosols measuring 2 µm across. Once you get to aerosols of 4–5 µm, almost any fabric can block more than 80% in both directions, she says.
Multiple layers of fabric, she adds, are more effective, and the tighter the weave, the better. Another study found that masks with layers of different materials — such as cotton and silk — could catch aerosols more efficiently than those made from a single material. - Eric Westman, a clinical researcher at Duke University School of Medicine in Durham, North Carolina, co-authored an August study11 that demonstrated a method for testing mask effectiveness. His team used lasers and smartphone cameras to compare how well 14 different cloth and surgical face coverings stopped droplets while a person spoke. “I was reassured that a lot of the masks we use did work,” he says, referring to the performance of cloth and surgical masks. But thin polyester-and-spandex neck gaiters — stretchable scarves that can be pulled up over the mouth and nose — seemed to actually reduce the size of droplets being released. “That could be worse than wearing nothing at all,” Westman says.
- Across the United States, mask use has held steady around 50% since late July. This is a substantial increase from the 20% usage seen in March and April, according to data from the Institute for Health Metrics and Evaluation at the University of Washington in Seattle. The institute’s models also predicted that, as of 23 September, increasing US mask use to 95% — a level observed in Singapore and some other countries — could save nearly 100,000 lives in the period up to 1 January 2021.
- Benn’s team, working independently of Benfield’s group, is in the process of enrolling around 40,000 people in Guinea-Bissau, randomly selecting half of the households to receive bilayer cloth masks — two for each family member aged ten or over. The team will then follow everyone over several months to compare rates of mask use with rates of COVID-like illness. She notes that each household will receive advice on how to protect themselves from COVID-19 — except that those in the control group will not get information on the use of masks. The team expects to complete enrolment in November.
Several scientists say that they are excited to see the results. But others worry that such experiments are wasteful and potentially exploit a vulnerable population. “If this was a gentler pathogen, it would be great,” says Eric Topol, director of the Scripps Research Translational Institute in La Jolla, California. “You can’t do randomized trials for everything — and you shouldn’t.” As clinical researchers are sometimes fond of saying, parachutes have never been tested in a randomized controlled trial, either.
Immunity
[edit]
- What’s happening in Brazil offers a cautionary tale. Research published in Science suggests that the slowdown of COVID-19 in the city of Manaus between May and October might have been attributable to herd-immunity effects (L. F. Buss et al. Science 371, 288–292; 2021). The area had been severely hit by the disease, and immunologist Ester Sabino at the University of São Paulo, Brazil, and her colleagues calculated that more than 60% of the population had been infected by June 2020. According to some estimates, that should have been enough to get the population to the herd-immunity threshold, but in January Manaus saw a huge resurgence in cases. This spike happened after the emergence of a new variant known as P.1, which suggests that previous infections did not confer broad protection to the virus. “In January, 100% of the cases in Manaus were caused by P.1,” Sabino says. Scarpino suspects that the 60% figure might have been an overestimate. Even so, he says, “You still have resurgence in the face of a high level of immunity.”
There’s another problem to contend with as immunity grows in a population, Ferrari says. Higher rates of immunity can create selective pressure, which would favour variants that are able to infect people who have been immunized. Vaccinating quickly and thoroughly can prevent a new variant from gaining a foothold. But again, the unevenness of vaccine roll-outs creates a challenge, Ferrari says. “You’ve got a fair bit of immunity, but you still have a fair bit of disease, and you’re stuck in the middle.” Vaccines will almost inevitably create new evolutionary pressures that produce variants, which is a good reason to build infrastructure and processes to monitor for them, he adds.- Christie Aschwanden, “Five reasons why COVID herd immunity is probably impossible”, Nature, (18 March 2021), 591, pp.520-522
- The COVID Human Genetic Effort is an international consortium aiming to discover the human genetic and immunological bases of the various clinical forms of SARS-CoV-2 infection. In particular, we search for: ...
- (iii) Single-gene variants, rare or common, which make certain individuals resistant to the infection by the SARS-CoV2 itself, despite repeated exposure, or resistant to the development of clinical manifestations despite infection.
“The false promise of herd immunity for COVID-19” (10/21/2020)
[edit]Christie Aschwanden, “The false promise of herd immunity for COVID-19”, Nature, (21 October 2020), 587, pp.26-28


- In May, the Brazilian city of Manaus was devastated by a large outbreak of COVID-19. Hospitals were overwhelmed and the city was digging new grave sites in the surrounding forest. But by August, something had shifted. Despite relaxing social-distancing requirements in early June, the city of 2 million people had reduced its number of excess deaths from around 120 per day to nearly zero.
In September, two groups of researchers posted preprints suggesting that Manaus’s late-summer slowdown in COVID-19 cases had happened, at least in part, because a large proportion of the community’s population had already been exposed to the virus and was now immune. Immunologist Ester Sabino at the University of São Paulo, Brazil, and her colleagues tested more than 6,000 samples from blood banks in Manaus for antibodies to SARS-CoV-2.
“We show that the number of people who got infected was really high — reaching 66% by the end of the first wave,” Sabino says. Her group concluded that this large infection rate meant that the number of people who were still vulnerable to the virus was too small to sustain new outbreaks — a phenomenon called herd immunity. Another group in Brazil reached similar conclusions.
Such reports from Manaus, together with comparable arguments about parts of Italy that were hit hard early in the pandemic, helped to embolden proposals to chase herd immunity. The plans suggested letting most of society return to normal, while taking some steps to protect those who are most at risk of severe disease. That would essentially allow the coronavirus to run its course, proponents said. - Despite widespread critique, the idea keeps popping up among politicians and policymakers in numerous countries, including Sweden, the United Kingdom and the United States. US President Donald Trump spoke positively about it in September, using the malapropism “herd mentality”. And even a few scientists have pushed the agenda. In early October, a libertarian think tank and a small group of scientists released a document called the Great Barrington Declaration. In it, they call for a return to normal life for people at lower risk of severe COVID-19, to allow SARS-CoV-2 to spread to a sufficient level to give herd immunity. People at high risk, such as elderly people, it says, could be protected through measures that are largely unspecified. The writers of the declaration received an audience in the White House, and sparked a counter memorandum from another group of scientists in The Lancet, which called the herd-immunity approach a “dangerous fallacy unsupported by scientific evidence”.
- Epidemiologists can estimate the proportion of a population that needs to be immune before herd immunity kicks in. This threshold depends on the basic reproduction number, R0 — the number of cases, on average, spawned by one infected individual in an otherwise fully susceptible, well-mixed population, says Kin On Kwok, an infectious-disease epidemiologist and mathematical modeller at the Chinese University of Hong Kong. The formula for calculating the herd-immunity threshold is 1–1/R0 — meaning that the more people who become infected by each individual who has the virus, the higher the proportion of the population that needs to be immune to reach herd immunity. For instance, measles is extremely infectious, with an R0 typically between 12 and 18, which works out to a herd-immunity threshold of 92–94% of the population. For a virus that is less infectious (with a lower reproduction number), the threshold would be lower. The R0 assumes that everyone is susceptible to the virus, but that changes as the epidemic proceeds, because some people become infected and gain immunity. For that reason, a variation of R0 called the R effective (abbreviated Rt or Re) is sometimes used in these calculations, because it takes into consideration changes in susceptibility in the population.
Although plugging numbers into the formula spits out a theoretical number for herd immunity, in reality, it isn’t achieved at an exact point. Instead, it’s better to think of it as a gradient, says Gypsyamber D’Souza, an epidemiologist at Johns Hopkins University in Baltimore, Maryland. And because variables can change, including R0 and the number of people susceptible to a virus, herd immunity is not a steady state.
Even once herd immunity is attained across a population, it’s still possible to have large outbreaks, such as in areas where vaccination rates are low. “We’ve seen that play out in certain countries where misinformation about vaccine safety has spread,” Salathé says. “In local pockets, you start to see a drop in vaccinations, and then you can have local outbreaks which can be very large, even though you’ve technically reached herd immunity as per the math.” The ultimate goal is to prevent people from becoming unwell, rather than to attain a number in a model. - Reaching herd immunity depends in part on what’s happening in the population. Calculations of the threshold are very sensitive to the values of R, Kwok says. In June, he and his colleagues published a letter to the editor in the Journal of Infection that demonstrates this4. Kwok and his team estimated the Rt in more than 30 countries, using data on the daily number of new COVID-19 cases from March. They then used these values to calculate a threshold for herd immunity in each country’s population. The numbers ranged from as high as 85% in Bahrain, with its then-Rt of 6.64, to as low as 5.66% in Kuwait, where the Rt was 1.06. Kuwait’s low numbers reflected the fact that it was putting in place lots of measures to control the virus, such as establishing local curfews and banning commercial flights from many countries. If the country stopped those measures, Kwok says, the herd-immunity threshold would go up.
- Herd-immunity calculations such as the ones in Kwok’s example are built on assumptions that might not reflect real life, says Samuel Scarpino, a network scientist who studies infectious disease at Northeastern University in Boston, Massachusetts. “Most of the herd-immunity calculations don’t have anything to say about behaviour at all. They assume there’s no interventions, no behavioural changes or anything like that,” he says. This means that if a transient change in people’s behaviour (such as physical distancing) drives the Rt down, then “as soon as that behaviour goes back to normal, the herd-immunity threshold will change.”
Estimates of the threshold for SARS-CoV-2 range from 10% to 70% or even more. But models that calculate numbers at the lower end of that range rely on assumptions about how people interact in social networks that might not hold true, Scarpino says. Low-end estimates imagine that people with many contacts will get infected first, and that because they have a large number of contacts, they will spread the virus to more people. As these ‘superspreaders’ gain immunity to the virus, the transmission chains among those who are still susceptible are greatly reduced. And “as a result of that, you very quickly get to the herd-immunity threshold”, Scarpino says. But if it turns out that anybody could become a superspreader, then “those assumptions that people are relying on to get the estimates down to around 20% or 30% are just not accurate”, Scarpino explains. The result is that the herd-immunity threshold will be closer to 60–70%, which is what most models show (see, for example, ref. 6). - Earlier in the pandemic, media reports claimed that Sweden was pursuing a herd immunity strategy by essentially letting people live their lives as normal, but that idea is a “misunderstanding”, according to the country’s minister for health and social affairs, Lena Hallengren. Herd immunity “is a potential consequence of how the spread of the virus develops, in Sweden or in any other country”, she told Nature in a written statement, but it is “not a part of our strategy”. Sweden’s approach, she said, uses similar tools to most other countries: “Promoting social distancing, protecting vulnerable people, carrying out testing and contact tracing, and reinforcing our health system to cope with the pandemic.” Despite this, Sweden is hardly a model of success — statistics from Johns Hopkins University show the country has seen more than ten times the number of COVID-19 deaths per 100,000 people seen in neighbouring Norway (58.12 per 100,000, compared with 5.23 per 100,000 in Norway). Sweden’s case fatality rate, which is based on the number of known infections, is also at least three times those of Norway and nearby Denmark.
“So you haven't caught COVID yet. Does that mean you're a superdodger?” (September 12, 2022)
[edit]Michaeleen Doucleff, “So you haven't caught COVID yet. Does that mean you're a superdodger?”, Goats and Soda, NPR, (September 12, 2022)
- Just as with HIV, some people have been exposed multiple times but never had symptoms and never tested positive.
"We've heard countless anecdotes about nurses and health-care workers being exposed without any protection and remaining negative over and over again," says pediatrician Jean-Laurent Casanova, who studies the genetics of viral resistance at Rockefeller University. "Or people share a household with someone who's been coughing for a couple of weeks, and one person stays negative."
So why haven't these people caught COVID?
After two years of hunting, a team at the University of California, San Francisco has come pretty close to answering the question.
"These findings are like hot off the presses," says immunogeneticist Jill Hollenbach, who led this research. "We haven't published them yet. It's all stuff that's been happening this summer."
Hollenbach and her team have found a genetic mutation that doesn't prevent the virus from infecting cells – that's what Landau was searching for in his HIV research – but still does something remarkable: It prevents a person from having COVID symptoms.
Turns out, stopping an infection altogether is an extremely tough nut for our bodies to crack. - "So when SARS-CoV-2 came along, of course, many labs looked to see if the same might be true for this virus," Landau says. And inspired by the story of CCR5, they went looking for mutations in the genes required for SARS-CoV-2 to enter and infect cells.
For COVID superdodgers, the situation appears to be more complex than for people resistant to HIV, Landau says, because the way SARS-CoV-2 infects cells is different from that of HIV.
Instead of using CCR5 to "open the cell's door," SARS-CoV-2 uses the ACE2 receptor. People can't live without ACE2. "The receptor regulates your blood pressure," Landau explains. So, unlike CCR5, you can't simply knock out the ACE2 receptor, he says. "You're not going to have many people walking around that don't have ACE2.
"Of course, there may be more subtle mutations in ACE2 which could play a role in resistance to SARS-CoV-2," he adds. "But there doesn't seem to be an obvious and dramatic mutation as is the case for HIV."
But perhaps what's more likely, he says, is that people have mutations in genes other than ACE2, and these mutations probably don't protect them from getting infected per se but do protect them from getting sick. - There are other ways to resist an infection besides denying the virus entrance into the cell, Landau explains. And they likely involve your body's immune system.
That's exactly what the team at UCSF has found.
Since the pandemic begin, Jill Hollenbach and her colleagues at UCSF have been studying people who test positive COVID but show no symptoms. "Not even a sniffle or a scratchy throat," she says. "So they are entirely asymptomatic."
After analyzing DNA from more than 1,400 people, they identified a mutation that helps a person clear out a SARS-CoV-2 so fast that their body doesn't have a chance to develop symptoms.
The mutation occurs in a gene called HLA, which is critical during the earliest stages of infection. Hollenbach and her colleagues found that having a particular mutation in that gene increases a person's chance of being asymptomatic by almost 10 times. They reported those preliminary findings online last September. - When a virus first enters cells, HLA signals to the immune system that cells are invaded and need help. That signal triggers a cascade of events that ultimately leads your body to make potent weapons specifically designed to fight SARS-CoV-2. These weapons include antibodies and T cells that uniquely recognize pieces of this virus. Once these targeted weapons are available, your immune system has a much easier time clearing up the infection. But these weapons take time to manufacture. And that delay allows the infection to spread and symptoms to develop.
- This summer, Hollenbach and her colleagues demonstrated that, with a specific mutation in HLA, some people have T cells that are already pre-programmed to recognize and fight off SARS-CoV-2. So there's no delay in generating COVID-specfic weaponry. It's already there.
"Your immune response and these T cells fire up much more quickly [than in a person without the HLA mutation]," Hollenbach says. "So for lack of a better term, you basically nuke the infection before you even start to have symptoms."
But here's the kicker. For the HLA mutation to work (and for you to have these pre-armed T cells), you first had to have been infected with another coronavirus.
"Most of us have been exposed to some common cold coronavirus at some point in life," she explains. And we all generate T cells to fight off these colds. But if you also have this mutation in your HLA, Hollenbach says, then just by mere luck, these T cells you make can also fight off SARS-CoV-2.
"It's definitely luck," she says. "But, you know, this mutation is quite common. We estimate that maybe 1 in 10 people have it. And in people who are asymptomatic, that rises to 1 in 5."
"What the immune response to the coronavirus says about the prospects for a vaccine” (17/8/2020)
[edit]Heidi Ledford, “What the immune response to the coronavirus says about the prospects for a vaccine”, Nature, (17 August 2020; updated 01 September 2020), 585, pp.20-21


- Researchers have been rummaging through results from the Common Cold Study and others like it, while scrambling to understand the human immune response to SARS-CoV-2 using animals and cell cultures, along with the latest molecular techniques. They have catalogued antibody and immune-cell responses with uncommon speed, determined which are likely to be the most effective, and designed vaccines and therapies that, in animal studies and small human studies, provoke at least short-term immune responses. But there is no quick and simple experiment that can firmly determine whether immunity will be effective or lasting. It is just too soon to know.
“Only the future can tell us,” says Reinhold Förster, an immunologist at the Hanover Medical School in Germany. - Sporadic accounts of reinfection — people recovering from COVID-19, only to test positive for the disease again — have stoked fears that immunity might be short-lived. On 24 August, news broke of a man in Hong Kong who had been infected twice, with genetically distinct variants of SARS-CoV-2, although he showed no symptoms the second time. It is the best documented case of reinfection so far.
Media outlets have latched on to such reports, and have offered gloomy predictions about the prospects for a vaccine. But scientists are more circumspect. “We now know that reinfection can occur,” says John Wherry, an immunologist at the University of Pennsylvania in Philadelphia. “It remains unclear how frequent of an event reinfection is, or what features of the immune response are associated with reinfection.”
For the immunologists digging deeply into SARS-CoV-2, the data are so far unsurprising — and that bodes well. “We’re seeing great immune responses and fantastic-looking antibodies. We just don’t know the longevity of that response yet,” says Mehul Suthar, a viral immunologist at Emory University in Atlanta, Georgia. “Unfortunately, that will take time.” - Long-term immunity can vary by type and also by degree of response. Vaccine developers often hope to elicit what’s known as sterilizing immunity, a response, typically mediated by antibodies, that can rapidly prevent a returning virus from gaining ground in the body. But not all vaccines or infections elicit the neutralizing antibodies required for sterilizing immunity. HIV, for example, rarely induces neutralizing antibodies, a fact that has complicated efforts to develop vaccines against it.
The signs so far for SARS-CoV-2 are encouraging. Several teams of researchers were quick to isolate neutralizing antibodies from people infected with the virus; most could mount such an antibody response within days of testing positive. And several vaccine candidates against SARS-CoV-2 provoke a strong antibody response, a positive sign that the vaccines might generate immunity. - Antibody responses tended to be highest in people with the most severe infection. Those with mild infections — which is to say most people who have had COVID-19 — sometimes produced small amounts of neutralizing antibody. This pattern is often seen with viruses: the longer, more severe infections are more likely to produce strong, durable responses. This is one reason that common-cold coronaviruses sometimes don’t yield long-lasting immunity, says Shane Crotty, a virologist at the La Jolla Institute for Immunology in California.
- When researchers tracked COVID-19 patients over time, they found that the amount of antibody peaked in the days following the onset of symptoms, then began to decline. In some study participants, the antibodies were practically undetectable within about three months. Several major media outlets reported this as a loss of immunity, saying that it would complicate vaccine efforts.
Many immunologists found that declaration a bit premature, however. The data showed a perfectly normal response to a viral infection, says Luis Barreiro at the University of Chicago in Illinois, who studies the evolution of immune responses to pathogens. When a virus attacks, it spurs the proliferation of B cells that produce antibodies capable of recognizing pieces of the virus. But once the infection is gone, antibody levels typically wane. “There is a lot of fear out there,” says Miles Carroll, an infectious-disease specialist with Public Health England in Porton Down, UK. “But I think, on the whole, that it’s a fairly robust immune response.”
To determine how significant that waning could be, researchers still need to know how much antibody it takes to successfully fend off SARS-CoV-2. “Even small amounts of antibodies can potentially still be protective,” says Mala Maini, a viral immunologist at University College London.
They also need to track antibody levels for longer, to find out whether they eventually hold at a low concentration — as is common in viral infections — or continue to rapidly decline. Given these unknowns, virologist Katie Doores of King’s College London, lead author of one of the antibody studies, says that the negative press coverage of her work caught her off guard. “Everyone seems to have gone ‘Argh!’,” she says. “But we don’t know what level of antibodies are needed for protection.” - Even if antibody levels dip to vanishingly low levels, the immune system often has a backup plan. Memory B cells linger in the bone marrow until a virus returns, when they take on a new identity as antibody-producing plasma cells. The data on memory B cells’ role in fending off COVID-19 are incomplete — the cells are more difficult to locate and count than antibodies — but thus far, the evidence suggests that they proliferate, says Marcus Buggert, an immunologist at the Karolinska Institute in Stockholm
- Like memory B cells, T cells are more complicated to probe than antibodies, but studies so far suggest that they are called into action during SARS-CoV-2 infection. One recent study surveyed immune responses in 36 people recovering from COVID-19, and found T cells that recognize the coronavirus in all of them. “It looks like a virus that’s very stimulatory to T cells,” says immunologist Danny Altmann at Imperial College London. “Most people have very good T-cell responses to it.”
- T-cell studies are also converging on the possibility of cross-reactivity, in which T cells that recognize other coronaviruses also recognize SARS-CoV-2. Several studies have found T cells that react to SARS-CoV-2 in blood samples from people who had not been exposed to the virus. And one team recently reported that some of these T cells react not only to SARS-CoV-2, but also to some common-cold coronaviruses. The results suggest that there may be some lasting cross-immunity between these cold coronaviruses and SARS-CoV-2, leading to speculation that this could be responsible, in part, for the wild differences in severity of COVID-19 symptoms between individuals.
Modeling
[edit]- The most challenging aspects of modelling COVID-19 are the sociological components, Meyers says. “What we know about human behaviour up until now is really thrown out of the window because we are living in unprecedented times and behaving in unprecedented ways.” Meyers and others are trying to adjust their models on the fly to account for shifts in behaviours such as mask wearing and social distancing.
Non-pharmaceutical interventions will continue to play a crucial part in keeping cases down, Del Valle says. The whole point is to break the transmission path, she says, and limiting social contact and continuing protective behaviours such as masking can help to reduce the spread of new variants while vaccines are rolling out.- Christie Aschwanden, “Five reasons why COVID herd immunity is probably impossible”, Nature, (18 March 2021), 591, pp.520-522
- What is troubling to me is our fascination with modeling. I think modeling, particularly when it's erroneous, can be very detrimental. I've watched so many different estimates of case numbers from these models taken literally by policymakers and the public and particularly the media.
The reality is you can't model beyond 30 days out. Just look at what is happening right now. We can't even predict why these surges occur or when they occur. Who, 30 days ago, could have developed a model that would accurately predict what we're seeing right now with Omicron? Who could have predicted that?- Michael Osterholm as quoted by Peter Bergen in “The infectious disease expert who warned us 800,000 Americans would die of Covid-19”, CNN, (Dec 11, 2021)
“Special report: The simulations driving the world’s response to COVID-19” (2/4/2020)
[edit]David Adam (additional reporting by Richard Van Noorden); “Special report: The simulations driving the world’s response to COVID-19”, Nature, (02 April 2020, correction 03 April 2020), 580, pp.316-318



- The true performance of simulations in this pandemic might become clear only months or years from now. But to understand the value of COVID-19 models, it’s crucial to know how they are made and the assumptions on which they are built. “We’re building simplified representations of reality. Models are not crystal balls,” Ferguson says.
- Many of the models simulating how diseases spread are unique to individual academic groups that have been developing them for years. But the mathematical principles are similar. They are based around trying to understand how people move between three main states, and how quickly: individuals are either susceptible (S) to the virus; have become infected (I); and then either recover (R) or die. The R group is presumed to be immune to the virus, so can no longer pass on the infection. People with natural immunity would also belong to this group.
The simplest SIR models make basic assumptions, such as that everyone has the same chance of catching the virus from an infected person because the population is perfectly and evenly mixed, and that people with the disease are all equally infectious until they die or recover. More-advanced models, which make the quantitative predictions policymakers need during an emerging pandemic, subdivide people into smaller groups — by age, sex, health status, employment, number of contacts, and so on — to set who meets whom, when and in which places (see ‘Measuring social mixing’).
Using detailed information on population size and density, how old people are, transport links, the size of social networks and health-care provision, modellers build a virtual copy of a city, region or an entire country using differential equations to govern the movements and interactions of population groups in space and time. Then they seed this world with an infection and watch how things unfold.
But that, in turn, requires information that can be only loosely estimated at the start of an epidemic, such as the proportion of infected people who die, and the basic reproduction number (R0) — the number of people, on average, to whom one infected person will pass the virus. - Modellers also simulate people’s activities in different ways. In ‘equation-based’ models, individuals are sorted into population groups. But as the groups are broken into smaller, more-representative social subsets to better reflect reality, the models get increasingly complicated. An alternative approach is to use an ‘agent-based’ method in which each individual moves around and acts according to their own specific rules — rather like the simulated characters in the video-game series The Sims.
“You have a couple of lines of code, and those drive how your agents act, how they go about their day,” says Elizabeth Hunter, who works on models of disease transmission at Technological University Dublin.
Agent-based models build the same kinds of virtual world as the equation-based ones, but each person can behave differently on a given day or in an identical situation. “These very specific models are extremely data hungry,” says Kathleen O’Reilly, an epidemiologist at the London School of Hygiene and Tropical Medicine (LSHTM). “You need to collect information on households, how individuals travel to work and what they do at the weekend.” For example, researchers at the LSHTM, University College London and the University of Cambridge, UK, collected social-contact data from more than 36,000 volunteers in a citizen-science project run through the BBC, the UK national broadcaster. Some modellers aiding the UK government used this data set, which was reported in a February preprint. - On 26 March, Ferguson and his team released global projections of the impact of COVID-19 that uses the simpler equation-based approach. It divides people into four groups: S, E, I and R, where ‘E’ refers to those who have been exposed, but who are not yet infectious. “They give broadly similar overall numbers,” says epidemiologist Azra Ghani, who is also in the Imperial group. For instance, the global projections suggest that, had the United States taken no action against the virus, it would have seen 2.18 million deaths. By comparison, the earlier agent-based simulation, run using the same assumptions about mortality rate and reproduction number, estimated 2.2 million US deaths.
The different kinds of model have their own strengths and weaknesses, says Vittoria Colizza, a modeller at the Pierre Louis Institute of Epidemiology and Public Health in Paris, who is advising the French government during the current emergency. “It depends on the question you want to ask,” she says.
One difference comes down to the number of people that modellers expect to act in the same way. Being able to bunch one group into a compartment inside an equation-based model makes things simpler — and quicker — because the model doesn’t need to run at the high-resolution level of treating everyone as an individual. When Colizza and her team wanted to test the effects on infection rates of compelling large parts of the French population to work from home, for example, she used an equation-based model. “We didn’t need to track each individual separately and see if they were spending some time at work or some time at school,” she says. - “Forecasts made during an outbreak are rarely investigated during or after the event for their accuracy, and only recently have forecasters begun to make results, code, models and data available for retrospective analysis,” Edmunds and his team noted last year in a paper that assessed the performance of forecasts made in a 2014–15 Ebola outbreak in Sierra Leone. They found that it was possible to reliably predict the epidemic’s course one or two weeks ahead of time, but no longer, because of the inherent uncertainty and lack of knowledge about the outbreak.
To minimize the impact of incomplete data and incorrect assumptions, modellers typically carry out hundreds of separate runs, with the input parameters tweaked slightly each time. This ‘sensitivity analysis’ tries to prevent model outputs swinging wildly when a single input changes. And to avoid too much reliance on one model, Ferguson says, the UK government took advice from a number of modelling groups, including teams at Imperial and the LSHTM (see, for example, ref.). “We all reached similar conclusions,” he says. - A reliable test to see who has been infected without showing symptoms — and so could be moved to the recovered group — would be a game changer for modellers, and might significantly alter the predicted path of the pandemic, says Edmunds.
To stress the need for such a test, a team at the University of Oxford, UK, led by theoretical epidemiologist Sunetra Gupta, has suggested that the pattern of recorded deaths in the United Kingdom might fit a range of SIR models, including one that assumes millions of people have already been infected but haven’t shown any symptoms. Only tests that reveal such past infections can show what’s going on in reality.
“Two decades of pandemic war games failed to account for Donald Trump" (4/8/2020)
[edit]Amy Maxmen & Jeff Tollefson, “Two decades of pandemic war games failed to account for Donald Trump”, Nature, (04 August 2020), 584, pp. 26-29


- By late January, Inglesby was anxious. The coronavirus outbreak was escalating at a frightening pace in China and spreading to other countries, including the United States. These were the kinds of foreboding signs that he had plugged into his simulations. But the Trump administration seemed to view the outbreak as China’s problem, says Inglesby. During the third week of January, Trump posted one reassuring tweet about the coronavirus and around 40 regarding his impeachment hearings, his rallies and defeating the Democrats. The only public action that the government took was to screen travellers coming from China for symptoms at a handful of international airports.
Inglesby knew that travel bans and checkpoints don’t sufficiently prevent the spread of contagious pathogens. So, on 26 January, he listed a series of actions needed to prepare the United States for the coronavirus — dubbed nCoV — in a 25-part Twitter thread. “Global and national leaders should be looking ahead to what must be done to prepare for the possibility nCoV can’t be contained,” he wrote. The list included vaccine development, expansion of personal protective equipment for health-care workers, and “very high numbers of reliable diagnostic tests”. - Fearing undetected transmission in the United States, scientists in the states of Washington, New York and California started vetting tests that detect the genetic sequence of the virus in late January — including a protocol developed by German researchers and disseminated by the WHO. But their efforts to roll tests out for public use hit a wall at the FDA, which wasn’t ready to authorize them. Meanwhile, officials at the CDC insisted that labs exclusively use tests that it had developed.
The CDC started shipping test kits to public-health departments on 6 February. On a Sunday morning, three days later, Kelly Wroblewski, the infectious-disease director at the Association of Public Health Laboratories in Silver Spring, Maryland, woke up to a flood of e-mails saying that the tests didn’t work. “We always knew laboratory testing was complicated, but it’s something that was often overlooked in these simulations,” says Wroblewski; she had participated in Crimson Contagion just months earlier.
While the CDC scrambled to fix the faulty tests, labs lobbied for FDA authorization to use tests that they had been developing. Some finally obtained the green light on 29 February, but without coordination at the federal level, testing remained disorganized and limited. And despite calls from the WHO to implement contact tracing, many city health departments ditched the effort, and the US government did not offer a national plan. Beth Cameron, a biosecurity expert at the Nuclear Threat Initiative in Washington DC, which focuses on national-security issues, says that coordination could have been aided by a White House office responsible for pandemic preparedness. Cameron had led such a group during Barack Obama’s presidency, but Trump dismantled it in 2018. - Confusion emerged in most pandemic simulations, but none explored the consequences of a White House sidelining its own public-health agency. Perhaps they should have, suggests a scientist who has worked in the US public-health system for decades and asked to remain anonymous because they did not have permission to speak to the press. “You need gas in the engine and the brakes to work, but if the driver doesn’t want to use the car, you’re not going anywhere,” the scientist says.
By contrast, New Zealand, Taiwan and South Korea showed that it was possible to contain the virus, says Scott Dowell, an infectious-disease specialist at the Gates Foundation who spent 21 years at the CDC and has participated in several simulations. The places that have done well with COVID-19 had “early, decisive action by their government leaders” he says. Cameron agrees: “It’s not that the US doesn’t have the right tools — it’s that we aren’t choosing to use them.” - After more than 70 people in Taiwan died as a result of SARS in 2003, the government mapped out its emergency-response network. “Every year since then, for the past 17 years, they’ve held annual outbreak exercises and practised, practised, practised,” Morrison says. When the first coronavirus cases were reported in mainland China, Taiwan’s well-oiled systems quickly kicked into gear. Despite its proximity to the outbreak, Taiwan has had only seven deaths from COVID-19 so far.
“How the pandemic might play out in 2021 and beyond” (8/5/2020)
[edit]Megan Scudellari, “How the pandemic might play out in 2021 and beyond”, Nature, (05 August 2020), 584, pp.22-25

- Around the world, epidemiologists are constructing short- and long-term projections as a way to prepare for, and potentially mitigate, the spread and impact of SARS-CoV-2, the virus that causes COVID-19. Although their forecasts and timelines vary, modellers agree on two things: COVID-19 is here to stay, and the future depends on a lot of unknowns, including whether people develop lasting immunity to the virus, whether seasonality affects its spread, and — perhaps most importantly — the choices made by governments and individuals. “A lot of places are unlocking, and a lot of places aren’t. We don’t really yet know what’s going to happen,” says Rosalind Eggo, an infectious-disease modeller at the London School of Hygiene & Tropical Medicine (LSHTM).
“The future will very much depend on how much social mixing resumes, and what kind of prevention we do,” says Joseph Wu, a disease modeller at the University of Hong Kong. Recent models and evidence from successful lockdowns suggest that behavioural changes can reduce the spread of COVID-19 if most, but not necessarily all, people comply.
Last week, the number of confirmed COVID-19 infections passed 15 million globally, with around 650,000 deaths. Lockdowns are easing in many countries, leading some people to assume that the pandemic is ending, says Yonatan Grad, an epidemiologist at the Harvard T. H. Chan School of Public Health in Boston, Massachusetts. “But that’s not the case. We’re in for a long haul.”
If immunity to the virus lasts less than a year, for example, similar to other human coronaviruses in circulation, there could be annual surges in COVID-19 infections through to 2025 and beyond. - In South Africa, which now ranks fifth in the world for total COVID-19 cases, a consortium of modellers estimates that the country can expect a peak in August or September, with around one million active cases, and cumulatively as many as 13 million symptomatic cases by early November. In terms of hospital resources, “we’re already breaching capacity in some areas, so I think our best-case scenario is not a good one”, says Juliet Pulliam, director of the South African Centre for Epidemiological Modelling and Analysis at Stellenbosch University.
- But there is hopeful news as lockdowns ease. Early evidence suggests that personal behavioural changes, such as hand-washing and wearing masks, are persisting beyond strict lockdown, helping to stem the tide of infections. In a June report, a team at the MRC Centre for Global Infectious Disease Analysis at Imperial College London found that among 53 countries beginning to open up, there hasn’t been as large a surge in infections as predicted on the basis of earlier data. “It’s undervalued how much people’s behaviour has changed in terms of masks, hand washing and social distancing. It’s nothing like it used to be,” says Samir Bhatt, an infectious-disease epidemiologist at Imperial College London and a co-author of the study.
- At Anhembi Morumbi University in São Paulo, Brazil, computational biologist Osmar Pinto Neto and colleagues ran more than 250,000 mathematical models of social-distancing strategies described as constant, intermittent or ‘stepping-down’ — with restrictions reduced in stages — alongside behavioural interventions such as mask-wearing and hand washing.
The team concluded that if 50–65% of people are cautious in public, then stepping down social-distancing measures every 80 days could help to prevent further infection peaks over the next two years. “We’re going to need to change the culture of how we interact with other people,” says Neto. Overall, it’s good news that even without testing or a vaccine, behaviours can make a significant difference in disease transmission, he adds. - Infectious-disease modeller Jorge Velasco-Hernández at the National Autonomous University of Mexico in Juriquilla and colleagues also examined the trade-off between lockdowns and personal protection. They found that if 70% of Mexico’s population committed to personal measures such as hand washing and mask-wearing following voluntary lockdowns that began in late March, then the country’s outbreak would decline after peaking in late May or early June. However, the government lifted lockdown measures on 1 June and, rather than falling, the high number of weekly COVID-19 deaths plateaued. Velasco-Hernández’s team thinks that two public holidays acted as superspreading events, causing high infection rates right before the government lifted restrictions.
- But exactly how much contact tracing and isolation is required to contain an outbreak effectively? An analysis by the Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group at the LSHTM simulated fresh outbreaks of varying contagiousness, starting from 5, 20 or 40 introduced cases. The team concluded that contact tracing must be rapid and extensive — tracing 80% of contacts within a few days — to control an outbreak. The group is now assessing the effectiveness of digital contact tracing and how long it’s feasible to keep exposed individuals in quarantine, says co-author Eggo. “Finding the balance between what actually is a strategy that people will tolerate, and what strategy will contain an outbreak, is really important.”
Tracing 80% of contacts could be near-impossible to achieve in regions still grappling with thousands of new infections a week — and worse, even the highest case counts are likely to be an underestimate. A June preprint from a Massachusetts Institute of Technology (MIT) team in Cambridge analysing COVID-19 testing data from 84 countries suggests that global infections were 12 times higher and deaths 50% higher than officially reported (see ‘Predicting cases and deaths’). “There are many more cases out there than the data indicate. As a consequence, there’s higher risk of infection than people may believe there to be,” says John Sterman, co-author of the study and director of the MIT System Dynamics Group. - Many human respiratory viruses — influenza, other human coronaviruses and respiratory syncytial virus (RSV) — follow seasonal oscillations that lead to winter outbreaks, so it is likely that SARS-CoV-2 will follow suit. “I expect SARS-CoV-2 infection rate, and also potentially disease outcome, to be worse in the winter,” says Akiko Iwasaki, an immunobiologist at the Yale School of Medicine in New Haven, Connecticut. Evidence suggests that dry winter air improves the stability and transmission of respiratory viruses, and respiratory-tract immune defence might be impaired by inhaling dry air, she adds.
In addition, in colder weather people are more likely to stay indoors, where virus transmission through droplets is a bigger risk, says Richard Neher, a computational biologist at the University of Basel in Switzerland. Simulations by Neher’s group show that seasonal variation is likely to affect the virus’s spread and might make containment in the Northern Hemisphere this winter more difficult.
In future, SARS-CoV-2 outbreaks could arrive in waves every winter. The risk to adults who have already had COVID-19 could be reduced, as with flu, but it would depend on how rapidly immunity to this coronavirus wears off, says Neher. What’s more, the combination of COVID-19, flu and RSV in autumn and winter could be challenging, says Velasco-Hernández, who is setting up a model of how such viruses might interact. - To end the pandemic, the virus must either be eliminated worldwide — which most scientists agree is near-impossible because of how widespread it has become — or people must build up sufficient immunity through infections or a vaccine. It is estimated that 55–80% of a population must be immune for this to happen, depending on the country.
Unfortunately, early surveys suggest there is a long way to go. Estimates from antibody testing — which reveals whether someone has been exposed to the virus and made antibodies against it — indicate that only a small proportion of people have been infected, and disease modelling backs this up. A study of 11 European countries calculated an infection rate of 3–4% up to 4 May, inferred from data on the ratio of infections to deaths, and how many deaths there had been. In the United States, where there have been more than 150,000 COVID-19 deaths, a survey of thousands of serum samples, coordinated by the US Centers for Disease Control and Prevention, found that antibody prevalence ranged from 1% to 6.9%, depending on the location. - The pandemic’s course next year will depend greatly on the arrival of a vaccine, and on how long the immune system stays protective after vaccination or recovery from infection. Many vaccines provide protection for decades — such as those against measles or polio — whereas others, including whooping cough and influenza, wear off over time. Likewise, some viral infections prompt lasting immunity, others a more transient response. “The total incidence of SARS-CoV-2 through 2025 will depend crucially on this duration of immunity,” wrote Grad, Harvard epidemiologist Marc Lipsitch and colleagues in a May paper exploring possible scenarios (see ‘What happens next?’).
- Researchers know little so far about how long SARS-CoV-2 immunity lasts. One study of recovering patients found that neutralizing antibodies persisted for up to 40 days after the start of infection; several other studies suggest that antibody levels dwindle after weeks or months. If COVID-19 follows a similar pattern to SARS, antibodies could persist at a high level for 5 months, with a slow decline over 2–3 years. Still, antibody production is not the only form of immune protection; memory B and T cells also defend against future encounters with the virus, and little is known so far about their role in SARS-CoV-2 infection. For a clear answer on immunity, researchers will need to follow a large number of people over a long time, says Michael Osterholm, director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota, Minneapolis. “We’re just going to have to wait.”
If infections continue to rise rapidly without a vaccine or lasting immunity, “we will see regular, extensive circulation of the virus”, says Grad. In that case, the virus would become endemic, says Pulliam. “That would be really painful.” And it is not unimaginable: malaria, a preventable and treatable disease, kills more than 400,000 people each year. “These worst-case scenarios are happening in many countries with preventable diseases, causing huge losses of life already,” says Bhatt.
If the virus induces short-term immunity — similar to two other human coronaviruses, OC43 and HKU1, for which immunity lasts about 40 weeks — then people can become reinfected and there could be annual outbreaks, the Harvard team suggests. A complementary CIDRAP report, based on trends from eight global influenza pandemics, points to significant COVID-19 activity for at least the next 18–24 months, either in a series of gradually diminishing peaks and valleys, or as a “slow burn” of continuing transmission without a clear wave pattern. Yet these scenarios remain only guesses, because this pandemic has so far not followed the pattern of pandemic flu, says Osterholm. “We’re in a coronavirus pandemic for which we have no precedents.”
Accountability related to the virus outbreak
[edit]
- "If you were to create a petri dish and say, how can we spread this the most? It would be cruise ships, jails and prisons, factories, and it would be bars," Alozie says. He was a member of the Texas Medical Association committee that created a COVID-19 risk scale for common activities such as shopping at the grocery store.
- Ogechika Alozie, as quoted by Will Stone, "How Bars Are Fueling COVID-19 Outbreaks”, Health-Shots, NPR, (August 18, 2020)
- Back in February, at what has been dubbed “Game Zero,” nearly 2,500 Spanish soccer fans of the club Valencia CF traveled to Milan, Italy, to attend a Champions League match, joining a crowd of 40,000 in San Siro Stadium. No masking, distancing or screening protocols were in place at the time. The result was described as a “biological bomb”—a superspreading event that led to infection both locally and in Spain. According to a Wall Street Journal report, “The military drove the dead away by the truckload” from hospitals in Bergamo, Italy.
- Carolyn Barber, “When Will Football Stadiums Look Normal Again?“, Scientific American, (October 21, 2020)
- “Military settings, including bases with many civilian employees, can be very vulnerable from an infectious disease perspective,” said Lindsey Leininger, a health policy researcher and a clinical professor at the Tuck School of Business at Dartmouth. “Better late than never for the mandate.”
- Helene Cooper and Jennifer Steinhauer “The U.S. military will mandate Covid-19 vaccines for troops.”, “New York Times”, (Aug. 9, 2021)
- With some exceptions, governments have made great efforts to put the well-being of their people first, acting decisively to protect health and to save lives. The exceptions have been some governments that shrugged off the painful evidence of mounting deaths, with inevitable, grievous consequences. But most governments acted responsibly, imposing strict measures to contain the outbreak.
Yet some groups protested, refusing to keep their distance, marching against travel restrictions — as if measures that governments must impose for the good of their people constitute some kind of political assault on autonomy or personal freedom! Looking to the common good is much more than the sum of what is good for individuals. It means having a regard for all citizens and seeking to respond effectively to the needs of the least fortunate.
It is all too easy for some to take an idea — in this case, for example, personal freedom — and turn it into an ideology, creating a prism through which they judge everything.- Pope Francis, “Pope Francis: A Crisis Reveals What Is in Our Hearts”, (Nov. 26, 2020); “Let Us Dream: The Path to a Better Future,” written with Austen Ivereigh.
- The pandemic has exposed the paradox that while we are more connected, we are also more divided. Feverish consumerism breaks the bonds of belonging. It causes us to focus on our self-preservation and makes us anxious. Our fears are exacerbated and exploited by a certain kind of populist politics that seeks power over society. It is hard to build a culture of encounter, in which we meet as people with a shared dignity, within a throwaway culture that regards the well-being of the elderly, the unemployed, the disabled and the unborn as peripheral to our own well-being.
To come out of this crisis better, we have to recover the knowledge that as a people we have a shared destination. The pandemic has reminded us that no one is saved alone. What ties us to one another is what we commonly call solidarity. Solidarity is more than acts of generosity, important as they are; it is the call to embrace the reality that we are bound by bonds of reciprocity. On this solid foundation we can build a better, different, human future.- Pope Francis, “Pope Francis: A Crisis Reveals What Is in Our Hearts”, (Nov. 26, 2020); “Let Us Dream: The Path to a Better Future,” written with Austen Ivereigh.
- The COVID-19 pandemic has disproportionately affected nursing home residents. According to a New York Times database, nursing homes account for 8 percent of cases and 41 percent of COVID-19-related deaths nationwide. While the clinical status of these patients is the major determinant of risk, debate continues on the relative importance of locale, the race and socioeconomic status of patients, facility size state regulations, payer mix, and ownership status. Nonetheless, there is agreement that, in general, America’s nursing homes are not designed, operated, or funded to deal effectively with infectious disease epidemics, and their staff are often too few in number and inadequately paid, protected, and trained.
- Terry T. Fulmer, Christopher F. Koller, and John W. Rowe; ”Reimagining Nursing Homes in the Wake of COVID-19”, National Academy of Medicine, (September 21, 2020)
- “Current recommendations worldwide are not to have large crowds mingle,” says Monica Gandhi, an infectious disease expert at the University of California, San Francisco. In an e-mail exchange, Gandhi tells me she could envision fans returning to stadiums under strict safety protocols (masking, distancing, employing good hand hygiene) and at perhaps 10 percent to 20 percent of capacity. “COVID-19 is not radioactive,” Gandhi said, “and there are ways to keep fans and the college community safe.”
- Monica Gandhi as quoted by Carolyn Barber, “When Will Football Stadiums Look Normal Again?“, “Scientific American”, (October 21, 2020)
- Part of the reason Gershon and Morse feel more confident about the subway: Transit agencies around the world are taking impressive efforts to get squeaky clean.
Gershon gives the example of New York's MTA: "They started a very extensive and exhaustive program of deep cleaning — those subways have been more clean than, like, forever," she says. "They shut them down every day from 2 to 5 a.m. to clean."
In addition, the New York subway system uses HVAC systems in each individual car, which turn over air quickly and filter out viral particles, Gershon says. That may aid in mitigating some of the risk associated with a respiratory disease.
These protective efforts are going on around the world. In Ethiopia, authorities have begun disinfecting public buses to reinstill confidence in transit. Hong Kong has successfully used a disinfection robot to spray bleach in train waiting areas. In Prague, authorities disinfect 10 to 12 trams a day with a deep cleaning. And Seoul has set up isolation rooms in case transit workers develop symptoms.- Robyn Gershon, as quoted in “Coronavirus FAQ: Is It Safe To Get On The Bus (Or Subway)?”, by Pranav Baskar, Goats and Soda, NPR, (August 28, 2020)
- There are several ways to improve air flow and quality, but many virus-fighting technologies are relatively new and difficult to research, experts say.
Costly changes to HVAC systems also can create a false sense of security, said Raj Gupta, executive chairman of ESD, a Chicago-based engineering firm.
Gupta said companies first should focus on three primary goals before addressing air quality: keeping sick people out of their space; enforcing distancing and mask-wearing; and emphasizing cleaning and hygiene.
“It’s important to realize that if we want to throw money at filters and everything, it’s not going to matter if we don’t do those first three things,” Gupta said. “People should not rely on it as a quick fix.”- Raj Gupta, as quoted in “Worries about COVID-19 spreading through the vents send Chicago building owners in search of cleaner air. ‘You can’t put a force field around your property.’”, by Ryan Ori, Chicago Tribune, (July 27, 2020)
- Outdoor workouts are a safer option than exercising inside a gym during the COVID-19 pandemic, according to I-Min Lee, professor in the Department of Epidemiology at Harvard T.H. Chan School of Public Health.
Outside, it’s more likely that any potential virus in the air will disperse, she said in an August 20, 2020 story on the website Popsugar. But Lee said that those exercising outdoors should still heed safety guidelines such as wearing a mask, distancing from others, and frequently washing their hands.
- Preliminary findings also suggest that around one-third of restaurant customers and around 40% of the hotel customers are willing to pay more for increased safety precautions. While customers expect hospitality businesses to implement more rigorous safety/cleaning procedures, a portion of them are willing to pay for those added safety measures (Gursoy et al., 2020). Further research is needed to determine the importance of each of these safety precautions, how such measures will influence customers’ attitudes and behaviors and whether customers are indeed willing to pay for them and by how much more.
Preliminary findings also indicate that a large proportion of restaurant customers (64.71%) and the majority of hotel customers (70.42%) believe that the use of various technologies in service delivery will be necessary in the COVID-19 environment in order to minimize human-to-human contact (examples: service robots, contactless payment such as Apply pay or contactless bank cards, digital menus that can be viewed on personal mobile devices via QR codes, contactless digital payments, keyless entry, touchless elevators, etc.) (Gursoy et al., 2020). These findings strongly suggest that technology integration and adoption into hospitality operations will likely be integral in the near future.- Dogan Gursoy & Christina G. Chi; “Effects of COVID-19 pandemic on hospitality industry: review of the current situations and a research agenda”, Journal of Hospitality Marketing & Management, Volume 29, 2020 - Issue 5 pp.527-529, (05 Jul 2020)
- The movement of cruise ships has the potential to be a major trigger of coronavirus disease (COVID-19) outbreaks. In Australia, the cruise ship Ruby Princess became the largest COVID-19 epicenter. When the Ruby Princess arrived at the Port of Sydney in New South Wales on March 19, 2020, approximately 2700 passengers disembarked. By March 24, about 130 had tested positive for COVID-19, and by March 27, the number had increased to 162. The purpose of this study is to analyze the relationship between the cruise industry and the COVID-19 outbreak. We take two perspectives: the first analysis focuses on the relationship between the estimated number of cruise passengers landing and the number of COVID-19 cases. We tracked the movement of all ocean cruise ships around the world using automatic identification system data from January to March 2020. We found that countries with arrival and departure ports and with ports that continued to accept cruise ships until March have a higher COVID-19 infection rate than countries that did not.
- Hirohito Ito, Shinya Hanaoka, and Tomoya Kawasaki; “The cruise industry and the COVID-19 outbreak”, Transportation Research Interdisciplinary Perspectives, 2020 May; 5: (Published online 2020)
- At one time, said Muller, the cruise industry treated onboard diseases as if they didn’t exist. “They just pretended it didn’t happen. Then in 2013, to their credit, they got smart and at first indication of a disease like norovirus, they’d pull up at the nearest harbor, get everybody off and do a deep clean.” (Norovirus, a contagious virus, causes vomiting and diarrhea.)
But the ships infected with the coronavirus earlier this year were not allowed to dock; they were forced to sail aimlessly as they sought an open port that would accept them. Meanwhile, the disease spread onboard. “That was the worst thing that could have happened,” Muller said.- Christopher Muller as quoted by Rosemary McClure, “To cruise or not to cruise. Loyalists face a dilemma”, Los Angeles Times, (Sep. 10, 2020)
- One much-publicized study on flying, conducted by the Defense Department, found that “overall exposure risk from aerosolized pathogens, like coronavirus, is very low” and concluded that a person would have to be sitting next to an infectious passenger for at least 54 hours to get an infectious dose of the virus through the air. But the “54-hour” number has since been removed from the report at the request of the authors, who worried it was being misinterpreted.
- Tariro Mzezewa, “Is It Safe to Fly During the Pandemic? Answers From the Experts”, New York Times, (11/25/2020)
- “Up-to-date information is crucial for the nation to effectively respond to this pandemic,” said Jean Ross, RN and a president of NNU. “Nurses know that we need detailed, consistent data to understand how and where the virus is spreading, who is most vulnerable to infection, and whether interventions are effective. We can use this information to learn how to prevent the spread of future pandemics. Unfortunately, instead of tracking and reporting Covid-19 data, federal and state governments have ignored, hidden, and manipulated Covid-19 data.”
There is widespread resistance on the part of health care employers to transparently provide information on nurse and other health care worker Covid-19 infection rates and fatalities. Meanwhile, federal, state, and local governments have failed to compel health care facilities to provide this data. If hospitals are not widely required to publicly disclose their deaths and infection rates, they have no incentive to avoid becoming zones of infection.- National Nurses United, “New report reveals widespread government failure to track and report data on Covid-19 deaths, testing, and infections”, (September 28, 2020)
- Most states report only a limited subset of Covid-19 data. But comprehensive reporting is necessary to fully grasp the scope of the Covid-19 pandemic and respond effectively. Only 15 states are providing infection numbers for all health care workers on a daily, semiweekly, or weekly basis. In May, the Centers for Medicare & Medicaid Services (CMS) began requiring nursing homes to provide Covid-related health care worker infection and mortality data, which is publicly available from CMS. For the hospital industry, however, data collection on health care worker infections and deaths has been woefully inadequate.
At the federal level, the U.S. Centers for Disease Control and Prevention (CDC) has been primarily responsible for tracking and reporting Covid-19 data, including information on testing, cases, hospitalizations, and deaths. But the Trump administration has moved hospital Covid-19 data reporting from the CDC to the U.S. Department of Health and Human Services (HHS), which has hired private companies under nondisclosure agreements, keeping the majority of the data collected hidden from public view. Trump appointees within HHS’ communications staff have reviewed and edited the CDC’s weekly scientific reports to downplay risks.- National Nurses United, “New report reveals widespread government failure to track and report data on Covid-19 deaths, testing, and infections”, (September 28, 2020)
- Benjamin, an internal medicine specialist and Maryland’s former secretary of health, said, “Just like in a restaurant, you take a mask off to eat popcorn or drink, etc. And of course, when you do that, if you’re infected, you will expel virus.” Especially, he noted, if you laugh or scream at the movie.
De St. Maurice, a physician who specializes in pediatrics and infectious disease and is the co-chief infection prevention officer for UCLA Health, agreed: “How often are they going to pull the mask back up? And movies make you laugh and shout.”
The health experts expressed concern that even proper social distancing might not be enough protection for a long period of exposure (say an average visit of two hours) to people who are not wearing masks.- Georges Benjamin & Annabelle De St. Maurice; as quoted in “How safe is it to go to indoor movie theaters during the COVID-19 pandemic?”, by Michael Ordono, Los Angeles Times, (Nov 23, 2020)
- Mandates for beauty services, especially hair and nails, are going to continue to change. But be sure to reach out to your hairstylists before you go to ensure they're wearing a mask — at the very least. "Clients should be asking if the hairstylists always wear protective gear including gloves and masks, and if everything used in the salon is scrubbed and sanitized after each client," dermatologist, Sapna Palep, founder of Spring Street Dermatology in New York City, tells Allure. "The chairs should also be wiped down thoroughly with antiseptic cloths." She notes that getting your hair done outside is safer, but either way, salons should be taking the temperatures of all staff and clients on a daily basis, and staff and clients should be screened for possible COVID-19 exposure.
- Sapna Palep as quoted in “Hair Salon Owners Are Making It Work During the Pandemic”, by Elizabeth Denton, Allure, (September 30, 2020)
- We asked Scott Pauley, a representative for the CDC, if it’s better to send laundry out to a wash-and-fold service than use a laundromat, and he told us, “[It] would really boil down to social distancing, and whether you could limit close contact with other individuals.” If you choose to use a laundering service, protect the laundry workers handling your dirty stuff: If anyone in your household is sick, don’t send your dirty laundry out immediately. “Bundle it up, let it sit for a few days, and then send it out,” Roberts said. “Viruses don’t survive that long,” she noted. “Certainly not over two days or three days.” An article in the Journal of Hospital Infection agrees, finding that coronaviruses survive a max of two days on hospital gowns at room temperature. Similarly, be careful with the clean bundles of laundry you get back. “If you’re immunocompromised, if you’ve got lung issues, and you’re worried about it, then put them in a closet or something that’s not used, and don’t open them for a few days,” Roberts said. “That should pretty much get rid of the virus.”
- Scott Pauley and Marilyn Roberts as quoted in “You Can Still Use Laundromats Safely During the Coronavirus Pandemic. Just Take a Few Precautions First.”, by Jackie Reeve, New York Times, (Updated April 23, 2020)
- Whether you do your laundry at home, in a laundromat, or in a shared laundry room in your building, public health experts say there are some general safety guidelines everyone can follow. If you’ve purchased or made cloth masks, the CDC recommends cleaning them frequently in a washing machine—they don’t currently offer any guidance for handwashing them. If anyone in your household is sick, or if you’re worried someone has been exposed to COVID-19, the CDC says not to shake your dirty laundry—this could spread the virus. The CDC also recommends wearing disposable gloves while handling laundry and washing your hands thoroughly when you take the gloves off (if you don’t have disposable gloves, wash your hands as often as you can). New York City’s Department of Health recommendations for businesses (PDF) say to avoid “hugging” dirty laundry to your body to reduce contact with possibly contaminated items. And Roberts says you can also leave your dirty laundry untouched and out of the way for a couple of days before washing to allow any pathogens to die off the surface.
- Jackie Reeve quoting CDC and New York City’s Department of Health in “You Can Still Use Laundromats Safely During the Coronavirus Pandemic. Just Take a Few Precautions First.”, New York Times, (Updated April 23, 2020)
- “It’s an ideal setting for transmission,” said Carlos del Rio, an infectious-disease expert at Emory University, referring to church gatherings. “You have a lot of people in a closed space. And they’re speaking loudly, they’re singing. All those things are exactly what you don’t want.”
- Carlos del Rio, as quotedin in “Churches Were Eager to Reopen. Now They Are Confronting Coronavirus Cases”, by Kate Conger, Jack Healy and Lucy Tompkins, New York Times, (Published July 8, 2020; updated July 10, 2020)
- “The idea of just opening a stadium and letting the crowds come back to capacity is clearly really foolish,” says Mark Rupp, chief of infectious disease at the University of Nebraska Medical Center. In an interview, Rupp tells me that while there could be ways of limiting crowds and enforcing safety measures, “I don’t think there is any way of taking the risk out of it completely, quite frankly.”
- Mark Rupp as quoted in “When Will Football Stadiums Look Normal Again?“, by Carolyn Barber, Scientific American, (October 21, 2020)
- The absence of a vaccine and effective treatment for COVID-19 has created public panic and burdened the health systems in most countries. Along with health workers’, sanitation personnel are also working at the frontlines in the war against the disease by keeping cities clean. Sanitation workers are engaged in Drudgery, Dangerous, Dirty and Dehumanising work that makes them vulnerable for developing the chronic respiratory diseases due to the exposure of various hazardous materials and toxic gases that are emitted from the solid waste. The sanitation workers working on a contractual basis are excluded from the labour policies and welfare programs who are playing a vital role in fighting the pandemic. Women sanitation workers are even more vulnerable because most of them are non-literate, poor in financial management and under-represented in the sanitation employee’s union. The local and state governments should protect and safeguard sanitation workers by providing them with adequate protective equipment, ensure payment of paying adequate salaries and provide them with health insurance.
- Pradeep S. Salve & Suresh Jungari ”Sanitation workers at the frontline: work and vulnerability in response to COVID-19”, pp.627-630, (published online: 13 Jul 2020)
- Outbreaks of the coronavirus in meat processing plants appear to play an outsized role in a handful of states with new infection rates far higher than the rest of the country. Or, as economist Ian Shepherdson put its: "The U.S. meat industry is the source of most new COVID hotspots."
- Ian Shepherdson as quoted in ”U.S. meat industry seen as source of most new COVID-19 hotspots”, by Kate Gibson, CBS News, (First published April 30, 2020; updated on May 1, 2020)
- More than 200 scientists earlier this month signed an open letter warning that public health agencies such as the WHO and U.S. Centers for Disease Control were ignoring the potential risk of the virus spreading through air circulating indoors.
The WHO responded by updating its guidance to acknowledge the possibility of airborne transmission of COVID-19.
“I think improving ventilation and improving air cleaning is one of the few lines of defense that we have,” said Brent Stephens, an engineering professor and chair of Illinois Institute of Technology’s Department of Civil Engineering, who signed the open letter.
“I don’t think we really have a good sense of how important it is,” said Stephens, who specializes in air quality in buildings. “We’re still learning.”- Brent Stephens as quoted in “Worries about COVID-19 spreading through the vents send Chicago building owners in search of cleaner air. ‘You can’t put a force field around your property.’”, by Ryan Ori, Chicago Tribune, (July 27, 2020)
- From the early days of the U.S. coronavirus outbreak, states have wrestled with the best course of action for the nation's imperiled bars and nightclubs. Many of these businesses find their economic prospects tied to a virus that preys on their industry's lifeblood — social gatherings in tight quarters.
Public health experts and top health officials, including the Dr. Tony Fauci, say the evidence is abundantly clear: When bars open, infections tend to follow.- Will Stone, "How Bars Are Fueling COVID-19 Outbreaks”, NPR, (August 18, 2020)
- Characteristics that might have led to transmission from the instructors in Cheonan include large class sizes, small spaces, and intensity of the workouts. The moist, warm atmosphere in a sports facility coupled with turbulent air flow generated by intense physical exercise can cause more dense transmission of isolated droplets (6,7). Classes from which secondary COVID-19 cases were identified included 5–22 students in a room ≈60 m2 during 50 minutes of intense exercise. We did not identify cases among classes with <5 participants in the same space. Of note, instructor C taught Pilates and yoga for classes of 7–8 students in the same facility at the same time as instructor B (Figure; Appendix Table 2), but none of her students tested positive for the virus. We hypothesize that the lower intensity of Pilates and yoga did not cause the same transmission effects as those of the more intense fitness dance classes.
- Sukbin Jang, Si Hyun Han, and Ji-Young Rhee, “Cluster of Coronavirus Disease Associated with Fitness Dance Classes, South Korea”, Research Letter, Volume 26, Number 8—August 2020
- The call from the U.S. came as Australia's Federal Agriculture Minister David Littleproud urged an international scientific investigation into the health risks associated with the wet markets.
"It only makes sense that we go and investigate these wildlife wet markets, to understand the risks that they pose to human health and also to biosecurity," Littleproud told reporters in Toowoomba, a town about 50 miles west of Brisbane, on Thursday, according to The Canberra Times.
"It is the responsibility of all global nations to undertake this work in a scientific manner, in a calm and methodical way, to understand the risks and whether they can be mitigated," he said.
In January, China closed the Huanan Seafood Wholesale Market in Wuhan where the SARS-CoV-2 virus that causes COVID-19 is thought to have emerged. But this month, the stalls at the market began reopening, though as Reuters notes, "their future looks uncertain with few customers as the virus stigma persists."- Scott Neuman, quoting David Littleproud in “U.S. Pressures China To Close Wet Markets Thought To Be Source Of COVID-19”, NPR, (April 23, 2020)
- “Seafood involves water and frozen products – the low temperature and high humidity is suitable for the virus to survive,” Wu Zunyou, chief epidemiologist at the Chinese Centre for Disease Control and Prevention, said at the time.
But while temperature, humidity and a few other factors are similar, most experts said the comparisons with the two Hong Kong markets ended there.
Infectious disease expert Dr Leung Chi-chiu noted the two mainland hotspots were massive wholesale markets spanning more than 100 hectares each, boasting thousands of stalls with huge refrigerators and other frozen cabinets for seafood storage.
“There are many more people going in and out of those places every day, enabling human-to-human transmission in places perfect for the survival of the virus,” he said.- Victor Ting, quoting Wu Zunyou and Leung Chichiu in “Should you be worried about Hong Kong’s wet market Covid-19 clusters, and do they compare to Wuhan or Beijing?”, South China Morning Post, (Aug 6, 2020)
- If people want to pursue accountability (about the lockdown of Wuhan City due to the COVID-19 outbreak and Wuhan City Government below-standard handling of the outbreak) and the public has a strong opinion, we (Zhou Xianwang and Wuhan Communist Party Chief Ma Guoqiang) are willing to step down.
- Zhou Xianwang (2020) cited in "Mayor of Wuhan, epicenter city of coronavirus, offers to resign over outbreak" on New York Post, 27 January 2019.
“Grocery workers died feeding the nation. Now, their families are left to pick up the pieces.” (April 13, 2021)
[edit]
Leticia Miranda, “Grocery workers died feeding the nation. Now, their families are left to pick up the pieces.”, NBC News, (April 13, 2021)
- More than one year after the pandemic first swept across the country, the plight of grocery workers who risked death to keep the country fed has raised questions about retail labor conditions and the responsibility of corporations in worker deaths from the coronavirus. At least 158 grocery workers have died from the virus, with at least 35,100 workers infected or exposed, according to data from the United Food and Commercial Workers International Union.
Walmart has seen at least 22 store workers die from Covid-19, according to worker-sourced data provided to United For Respect, a nonprofit labor advocacy group. Walmart declined to comment on the number of coronavirus cases among its 1.5 million U.S.-based workers. - For those hundreds of families like McMiller’s who continue on after the loss of a loved one, there is little recourse across companies to seek monetary damages under current labor laws, according to Steven Levin, senior partner with the Chicago-based personal injury law firm Levin & Perconti. States such as Alaska to Connecticut are considering additional immunity laws that would make it harder to sue businesses for civil damages related to coronavirus cases.
“Many of these cases are going to be challenging even if the employer was screwing up and didn’t have the right procedures,” Levin said. “But how do we know how you got Covid? How do we know you didn’t get it at home or at a party? Where the infection came from — that is a factual legal challenge.” - Since the early days of the pandemic, grocery workers have been at the center of the country’s battle against the coronavirus. Like health care workers, they come into close contact with customers, raising their likelihood of becoming infected with the virus. But while Walmart, Kroger and Amazon, which owns Whole Foods Market, all offer paid sick leave, 55 percent of grocery workers say they do not have paid sick leave benefits, according to the Shift Project at the Harvard Kennedy School.
“We started to see retail workers get sick and put themselves on self-quarantine,” said Kim Cordova, president of the UFCW Local 7 in Colorado, which represents more than 17,000 private sector grocery workers in the state. “They had to use personal time to take time off or go to work sick.” - But while sales skyrocketed, many grocers were slow to roll out mask mandates and social distancing guidelines, Cordova said. Costco was the first national grocery chain to require masks, beginning in May last year. It wasn’t until July — four months into the pandemic — that nearly all major grocers required customers to wear a mask. And while Kroger, Walmart and Amazon all offered additional hazard pay to workers, many of those benefits expired in May.
“Workers felt [hazard pay] was just like a carrot to keep you working during this dangerous health crisis,” she said. - Walmart’s coronavirus case disclosures are “nonexistent,” said Bianca Agustin, research director with United For Respect, who has been leading crowdsourced submissions of positive cases and deaths at the company. Walmart did not respond to a request for comment on its coronavirus case disclosures.
“Walmart and, to a larger extent, the Trump administration’s OSHA, was unwilling to admit that these huge retailers could be potential Covid hot spots,” she said, referring to the Occupational Safety and Health Administration. - Under former President Donald Trump, OSHA was slow to hire and replace investigators, even as coronavirus cases rose. Between March 2020 and April 4, OSHA received about 14,000 coronavirus-related complaints in 2020 and opened only about 1,900 for inspection, Jesse Lawder, a spokesperson for the agency, said in an emailed statement. Supermarkets and grocery stores made up about 17 percent of coronavirus-related inspections between March 2020 and April 8.
“All these retail workers filed complaints and OSHA didn’t respond with an inspection,” Berkowitz said. “They told retailers to do what they can. It was a real abdication of responsibility.”
Effects of the virus outbreak
[edit]- CDC recognizes that wearing masks may not be possible in every situation or for some people such as children. Some older adults with cognitive, sensory, or behavioral issues might find wearing a mask difficult. Adaptations and alternatives should be considered whenever possible to increase the feasibility of wearing a mask or to reduce the risk of spreading COVID-19 if it is not possible to wear one. These adults need to take extra precautions when interacting with others. Additionally, some people may rely on reading lips or facial expressions during social interactions. This can be difficult when others are wearing masks that cover large portions of their face.
Who should NOT use masks: Children under age 2 or anyone who has trouble breathing, is unconscious, or is incapacitated or otherwise unable to remove the mask without assistance.- CDC, “People with Certain Medical Conditions”, (Updated Dec. 29, 2020)
- This theme of helping others has stayed with me these past months. In lockdown I’ve often gone in prayer to those who sought all means to save the lives of others. So many of the nurses, doctors and caregivers paid that price of love, together with priests, and religious and ordinary people whose vocations were service. We return their love by grieving for them and honoring them.
Whether or not they were conscious of it, their choice testified to a belief: that it is better to live a shorter life serving others than a longer one resisting that call. That’s why, in many countries, people stood at their windows or on their doorsteps to applaud them in gratitude and awe. They are the saints next door, who have awakened something important in our hearts, making credible once more what we desire to instill by our preaching.
They are the antibodies to the virus of indifference. They remind us that our lives are a gift and we grow by giving of ourselves, not preserving ourselves but losing ourselves in service.- Pope Francis, “Pope Francis: A Crisis Reveals What Is in Our Hearts”, (Nov. 26, 2020); “Let Us Dream: The Path to a Better Future,” written with Austen Ivereigh.
- Honestly, from the experience of SARS (in 2002-2003), if the (COVID-19 outbreak) situation is so serious, no one will go to a casino (in Macau).
- Ho Iat Seng (2020) cited in "Macau casinos could be closed if risk of Wuhan virus rises: Ho Iat Seng" on Inside Asian Gaming, 23 January 2020.
- We (Government of Macau) don't know if this is the peak of the (COVID-19) disease. I think it could be only after Lunar New Year (CNY) because now people are moving a lot. If there is contagion it is now, during these travels, but maybe the most critical time could be registered after the CNY. That's why we took the hard decision to cancel CNY festivities, to prevent further aggravation of the disease.
- Ho Iat Seng (2020) cited in "Chief Executive advises residents to stay home during CNY or at least wear health masks outside" on Macau Business, 23 January 2020.
- It was a hard decision (to close casinos in Macau for two weeks after a hotel worker was infected by COVID-19), but we (Government of Macau) must make it for the health of Macau residents. Macau can still withstand economic losses.
- Ho Iat Seng (2020) cited in "Coronavirus: casinos to close in Macau for at least two weeks after hotel worker infected" on South China Morning Post, 4 February 2020.
- Across the country, as millions open their doors and windows every night to cheer doctors and nurses battling a deadly pandemic, people like Padilla operate in the shadows. They work the same 12-hour shifts, using special training to ensure hospitals stay clean, but for considerably less pay and sometimes without the same protective gear given to doctors and nurses.
Environmental service workers “are such an integral part of the whole health care team,” said Jane Hopkins, executive vice president of Service Employees International Union's Northwest chapter. “In a hospital, they’re just as important as a doctor – they’re just doing a completely different job.”- Lindsay Schnell, [“'We're heroes, too:' Hospital janitors risk lives to stop spread of COVID-19”, USA TODAY, (June 12, 2020)
- We (Japan) may have more information about the risk of infection and the risk of severity of getting the (COVID-19) virus, so we can prepare. So we can have some precautions for infection control ... but I hope we can conduct the Tokyo Olympics as scheduled.
- Koji Wada (2020) cited in "Japan hopefully has time to build virus defences before Olympics - professor" on The Star Online, 30 January 2020.
- The impact on the (China's) economy (by this COVID-19 outbreak) is gaining weight, especially on transport, tourism, hotels, catering and entertainment. But, the impact will be temporary and will not change the positive foundation of China's economy. Many have tried to estimate the impact (of this COVID-19 outbreak) based on the impact of SARS in 2003, but China's economic power and ability to handle such an outbreak is significantly stronger than in those days.
- Lian Weiliang (2020) cited in "Coronavirus will ‘hit China’s economy but not as much as Sars’" on South China Morning Post, 3 February 2020.
- If local (COVID-19) transmission is indeed established, that could be very dangerous, and Hong Kong can become another Wuhan.
- Yuen Kwok-yung (2020) cited in "'Hong Kong in danger of becoming another Wuhan'" on rthk.hk, 2 February 2020.
- COVID-19 has "brought home not only the realities of our vulnerabilities but the potential risk of this kind of a pandemic in man-made context, genetically modified, that is targeted in ways that are intended to undermine, attack our systems and our health," said Zarate, an NBC News contributor who oversaw the creation of infrastructure to combat terrorism financing in the wake of the terrorist attacks of Sept. 11, 2001. "Our homeland security posture and even our counterterrorism approach will be fundamentally altered by this crisis."
- Juan Zarate as quoted in “COVID-19 has shown U.S., U.K. are vulnerable to biological terrorism, experts say” by Willem Marx, NBCNews, (May 18, 2020, 3:00 AM MDT / Updated May 18, 2020)
Crimonology
[edit]- Like other viral pathogens, SARS-CoV-2 is closely dependent on the complexity of human behavior and human interactions. There are many documented outbreaks of respiratory pathogens in jails and prisons in many countries. Custodial institutions have been the epicenter of outbreaks of infections amongst prisoners amplifying infections at rates far exceeding those in nonincarcerated communities. Highly transmissible viral infections such as measles, mumps, and the novel coronavirus disseminates rapidly among inmates and staff and potentially into the larger community. Overcrowding, insufficient sanitation, poor ventilation, and inadequate healthcare in prisons contribute to enabling these institutions as breeding grounds of infectious disease outbreaks. Detention and incarceration of any kind involves large groups of people living in cohorts in confined spaces creating many challenges for curbing the spread of COVID-19. The number of single rooms in jails or prisons are insufficient to adhere to the recommended isolation and quarantine guidelines and limits the ability to implement strict infection prevention protocols.
- Carlos Franco-Paredes, Katherine Jankousky, Jonathan Schultz, Jessica Bernfeld, Kimberly Cullen, Nicolas G. Quan, Shelley Kon, Peter Hotez, Andrés F. Henao-Martínez, and Martin Krsak; “COVID-19 in jails and prisons: A neglected infection in a marginalized population”, PLoS Negl Trop Dis. 2020 Jun; 14(6): e0008409.
- Terrorists – like all criminals – have sought to profit from COVID-19, to make money, strengthen their base and to fuel division.
- Jürgen Stock, “INTERPOL – Terrorist groups using COVID-19 to reinforce power and influence”, "Interpol", (22 December 2020)
- The risk of rapidly increasing transmission of the disease within prisons or other places of detention is likely to have an amplifying effect on the epidemic, swiftly multiplying the number of people affected.
- WHO/Europe, “Preparedness, prevention and control of COVID-19 in prisons and other places of detention”, (15 March 2020)
- COVID-19 provides the clearest illustration yet that prison health is public health. It is more important than ever for our governments and prison administrations to abide by the principle, enshrined in international law, that prisoners have an equal right to health and healthcare. Realistically, the only way that most countries could afford to meet this obligation is by first reducing their use of incarceration. This means ruling out custody for less serious, non-violent offending; and reversing the recent growth in the length of prison sentences.
- World Prisons Brief, “COVID-19 in prisons: a major public health risk“, Prisonstudies.org, (2020 May 29)
“Has COVID-19 Changed Crime? Crime Rates in the United States during the Pandemic” (7/8/2020)
[edit]John H. Boman, IV and Owen Gallupe; “Has COVID-19 Changed Crime? Crime Rates in the United States during the Pandemic”, Am J Crim Justice. 2020 Jul 8 : 1–9.
- In response to the COVID-19 pandemic, state-level governments across the United States issued mandatory stay-at-home orders around the end of March 2020. Though intended to stop the spread of the COVID-19 virus, the lockdowns have had sweeping impacts on life in ways which were not originally planned. This study’s purpose is to investigate the extent to which governmental responses to COVID-19 have impacted crime rates in the U.S. Compared to the pre-pandemic year of 2019, crime – as measured by calls for service to law enforcement – has decreased markedly. However, there are multiple indications that the crime drop is being driven by decreases in minor offenses which are typically committed in peer groups. At the same time, serious crimes which are generally not committed with co-offenders (namely homicide and intimate partner violence) have either remained constant or increased. As such, the crime drop appears to be hiding a very disturbing trend where homicides remain unchanged and intimate partner batteries are increasing. Since many offenders would presumably be committing less serious crimes in a non-pandemic world, we raise attention to the possibility that mandatory lockdown orders may have taken minor offenders and placed them into situations where there is rampant opportunity for intimate partner violence, serious batteries, and homicides. While crime in the U.S. appears to be down overall, this good news should not blind us to a troubling co-occurring reality – a reality that paints a dim picture of unintended consequences to public health and criminal justice finances as a result of COVID-19 lockdowns.
- Worldwide lockdowns and quarantines issued in response to the COVID-19 global pandemic have brought about a number of implications for everyday life. Unfortunately, most of the impacts of COVID-19 and the resulting lockdowns have been alarmingly negative – a gradually increasing death toll, job losses, unemployment, and a looming global financial crisis are among the most commonly reported issues worldwide. However, the pause to everyday life initiated by state governments in response to COVID-19 has resulted in scattered examples of positive changes as well. For instance, a notable drop in carbon-based emissions has reduced air pollution (Bauwens et al., 2020). Partially as a result of this, air quality across the globe has improved, resulting in a decline in the number of air-pollutant-instigated respiratory health problems (Dutheil, Baker, & Navel, 2020).
- Nearly every major news source which has reported on this issue since COVID-19 lockdowns began have found a similar phenomenon: Crime is down across the United States. The most common metric of these reports is police calls for service (911 calls). Probably due to the fact that 911 calls are concrete events which are easily trackable over time, major news outlets like The Washington Post (Jackman, 2020), USA Today (Jacoby, Stucka, & Phillips, 2020), and CNN (Waldrop, 2020) have all used this as the metric for determining that crime is down across the U.S.
In these major news sources, the extent to which crime has decreased since COVID-19 lockdowns began varies dramatically. For example, The Washington Post (Jackman, 2020) reported decreases in calls for service in 29 of 30 jurisdictions including a 25% decline in Chicago and ~ 20% in Washington and Baltimore between March 16 and April 22, 2020 compared to the same period in 2019. USA Today reported that weekly calls for service dropped “at least” 12% between February 2 and March 28, 2020 across 30 police agencies (Jacoby et al., 2020). Although not providing exact numbers, CNN reports that calls for police service are down in New York City. Regarding the crime drop, New York City Police Commissioner Dermot Shea told CNN that “Crime has dropped off – off the face of the map, really” (Waldrop, 2020). - Despite having a well-executed study that points to emerging evidence as to how COVID-19 is impacting crime rates, Ashby (2020) faced the same limitations all criminologists currently do about how crime is fluctuating in response to COVID-19: A lack of sufficient data. The most widely available data source right now on judging how COVID-19 has impacted crime comes from publicly available police data. The limitations of official police data are well documented. Due to police simply not knowing about offenses due to under/non-reporting of crime (MacDonald, 2002), police data do a very poor job at capturing one of Ashby’s variables – serious assaults which occur within the home. This variable is capturing something that is similar to, but not synonymous with, intimate partner violence (IPV; see Ashby’s discussion on p. 14). Evidence dating back over 20 years demonstrates that IPV is most frequently not reported to the police (e.g., Bachman & Saltzman, 1995). While estimates vary, only about half of IPV incidents result in a 911 call (Reaves, 2017). And due to the frequent ambiguity of 911 calls (see New Jersey Division of Criminal Justice, 2003) and the common situation where law enforcement officers cannot substantiate a domestic battery occurring (only about 40% of cases result in arrest; Reaves, 2017), IPV is certainly an underestimated variable with police data (cf. Bachman & Saltzman, 1995; Reaves, 2017; also see Gracia, 2004). Self-report data on perpetration or victimization data would be highly preferential to capture IPV (see Straus & Gelles, 1990).
- During COVID-19 lockdowns, peer dynamics have clearly been altered due to stay-at-home orders and social distancing requirements. We argue that these disruptions to established social patterns are the driving force behind the reduction in offending over the course of the pandemic. Without access to peer groups, the context in which much criminal behavior occurs is removed (Osgood, Wilson, O’Malley, Bachman, & Johnston, 1996). With no school to attend, students cannot congregate afterwards. This is important since a typical day would see a ‘spike’ in crime after school lets out when youthful offenders have little to no supervision (see Gottfredson, Gottfredson, & Weisman, 2001). While the after-school crime spike is a time and context in which substantial amounts of minor offending typically occurs, it cannot occur if adolescents are not attending school.
During the stay-at-home order, the opportunity for underage drinking with friends – and the minor offending that often accompanies it – also largely disappears without the option of attending parties. Since groupy offenses constitute the majority of criminal acts, it is likely that the NIBRS data will eventually show that they carried the bulk of the crime reduction following state government responses to COVID-19. Supporting this anecdotally, Chief Tullis noted that since the start of mandatory lockdowns in Ohio, his officers are seeing very few peer groups coming into conflict with the law. Underage drinking is nearly non-existent since nobody is going out in groups. In fact, nearly everyone getting arrested in his department’s jurisdiction are acting alone. Due to the commonality of arresting people who are committing crime with co-offenders, Chief Tullis stressed that the lockdowns issued in response to COVID-19 have represented a dramatic shift in policing.
”Prisons and custodial settings are part of a comprehensive response to COVID-19” (4/5/2020)
[edit]Stuart A Kinner, Jesse T Young, Kathryn Snow, Louise Southalan, Daniel Lopez-Acuña, Carina Ferreira-Borges, and Éamonn O'Moore; ”Prisons and custodial settings are part of a comprehensive response to COVID-19”, Lancet Public Health. 2020 Apr; 5(4): e188–e189.
- Prisons are epicentres for infectious diseases because of the higher background prevalence of infection, the higher levels of risk factors for infection, the unavoidable close contact in often overcrowded, poorly ventilated, and unsanitary facilities, and the poor access to health-care services relative to that in community settings. Infections can be transmitted between prisoners, staff and visitors, between prisons through transfers and staff cross-deployment, and to and from the community. As such, prisons and other custodial settings are an integral part of the public health response to coronavirus disease 2019 (COVID-19).
- Prisons concentrate individuals who are susceptible to infection and those with a higher risk of complications. COVID-19 has an increased mortality in older people and in those with chronic diseases or immunosuppression. Notably, multimorbidity is normative among people in prison, often with earlier onset and greater severity than in the general population, and prison populations are ageing in many countries.7 Furthermore, inadequate investment in prison health, substantial overcrowding in some prison settings, and rigid security processess have the potential to delay diagnosis and treatment.
As such, COVID-19 outbreaks in custodial settings are of importance for public health, for at least two reasons: first, that explosive outbreaks in these settings have the potential to overwhelm prison health-care services and place additional demands on overburdened specialist facilities in the community; and second, that, with an estimated 30 million people released from custody each year globally, prisons are a vector for community transmission that will disproportionately impact marginalised communities. - Prison health is public health by definition. Despite this and the very porous borders between prisons and communities, prisons are often excluded or treated as separate from public health efforts. The fast spread of COVID-19 will, like most epidemics, disproportionately affect the most disadvantaged people. Therefore, to mitigate the effects of prison outbreaks on tertiary health-care facilities and reduce morbidity and mortality among society's most marginalised, it is crucial that prisons, youth detention centres, and immigration detention centres are embedded within the broader public health response.
Education
[edit]- "We're going to have a mental health epidemic among our children in this country. …The poorest kids, they know people who died, they know people who are sick. The very air you breathe, the people you pass on the street are suddenly dangerous to you. All of that trauma is going to come into our schools and into our classrooms, and we really need to prepare for this.
- Geoffrey Canada, "CNN Coronavirus Townhall", (May 21, 2020); as quoted in Education expert: "We're going to have a mental health epidemic among our children in this country", by Jessie Yeung, Adam Renton and Zamira Rahim, CNN, (May 21, 2020)
- "As a pediatrician, I am really seeing the negative impacts of these school closures on children," Dr. Danielle Dooley, a medical director at Children's National Hospital in Washington, D.C., told NPR. She ticked off mental health problems, hunger, obesity due to inactivity, missing routine medical care and the risk of child abuse — on top of the loss of education. "Going to school is really vital for children. They get their meals in school, their physical activity, their health care, their education, of course."
- Danielle Dooley, as quoted in “Are The Risks Of Reopening Schools Exaggerated?”, by Anya Kamenetz, All Things Considered, NPR, (October 21, 2020)
- A recent study from Yale University could potentially shed some light on these questions. It tracked 57,000 childcare workers, located in all 50 states, Washington, D.C., and Puerto Rico, for the first three months of the pandemic in the United States. About half continued caring for very young children, such as the children of essential workers, while the other half stayed home. The study found no difference in the rate of coronavirus infections between the two groups, after accounting for demographic factors.
Walter Gilliam, lead author of the study and a professor of psychology at the Yale Child Study Center, cautioned that it's difficult to generalize this report to a K-12 schools setting, because the children were mostly under the age of 6 and kept in very small groups — and, he said, the childcare workers were trained in health and safety and reported following strict protocols around disinfection. However, he said, "I think it would be great to do this study with school teachers and see what we can find out."- Walter Gilliam, as quoted in “Are The Risks Of Reopening Schools Exaggerated?”, by Anya Kamenetz, All Things Considered, NPR, (October 21, 2020)
- When you add up what we know and even what we still don't know, some doctors and public health advocates said there are powerful arguments for in-person schooling wherever possible, particularly for younger students and those with special needs.
"Children under the age of 10 generally are at quite low risk of acquiring symptomatic disease," from the coronavirus, said Dr. Rainu Kaushal of Weill Cornell Medicine. And they rarely transmit it either. It's a happy coincidence, Kaushal and others said, that the youngest children face lower risk and are also the ones who have the hardest time with virtual learning.- Rainu Kaushal, as quoted in “Are The Risks Of Reopening Schools Exaggerated?”, by Anya Kamenetz, All Things Considered, NPR, (October 21, 2020)
- “It’s not reasonable to ask adolescents and young adults to take on additional risks for the enjoyment of spectators and the financial gain of their universities,” said Dr. Adam Ratner, the director of pediatric infectious diseases at New York University School of Medicine and Hassenfeld Children’s Hospital at N.Y.U. Langone Health.
There are places where athletes have been exempt from campus shutdowns, he said: “Everyone is used to there being a different set of rules for athletic programs at universities,” and it’s particularly troubling to see that playing out in a pandemic.- Perri Klass, M.D., “After a Covid-19 Semester, College Doctors Reflect on Sports”, New York Times, (Dec. 14, 2020)
- “These schools have reached the conclusion, right or wrong, that because of the risks of the virus, students should be at home with their families, studying on Zoom,” Mr. Edelman said. “But they’re willing to take a small number of students, who are disproportionately minorities, and fly them back and forth across the country to compete in sporting events indoors because it’s revenue-generating. Ethically, that’s appalling, and logically it doesn’t make sense.”
- Perri Klass, M.D., “After a Covid-19 Semester, College Doctors Reflect on Sports”, New York Times, (Dec. 14, 2020)
- Dr. Dean said that in his experience, the students involved in fall sports had been particularly careful to follow the rules about reducing possible Covid exposure. “The fall sport athletes have something to lose, they’re being safe, not going to parties,” he said. “They want to play,” and they know that if they test positive, they can’t.
His colleague Dr. James Nataro, the chairman of pediatrics at the University of Virginia, who is a pediatric infectious diseases expert who studies emerging infections, said that the university, which had students on campus and held in-person classes in the fall, generally did well. “Against almost every prediction, the students complied, the students were just wonderful,” he said.
The school is part of the Atlantic Coast Conference, which modified its schedule to include more in-conference games, Dr. Nataro said, and spectators were kept to a minimum. Still, he said, it was clear, watching football games, that “there were lots of opportunities for transmission,” and some of the good results may have been a matter of luck. And though he himself loves football, he said, he worries about “the lesson it sends if people turn on the TV and watch all these guys without masks standing next to each other — that image isn’t lost.”- Perri Klass, M.D., “After a Covid-19 Semester, College Doctors Reflect on Sports”, New York Times, (Dec. 14, 2020)
- On Oct. 14, the Infectious Diseases Society of America gave a briefing on safe school reopenings. Bottom line? "The data so far are not indicating that schools are a superspreader site," said Dr. Preeti Malani, an infectious disease specialist at the University of Michigan's medical school.
- Preeti Malani in “Are The Risks Of Reopening Schools Exaggerated?”, by Anya Kamenetz, All Things Considered, NPR, (October 21, 2020)
“The virus that shut down the world: Education in crisis” (12//28/2020)
[edit]
Raphael Pouget, “The virus that shut down the world: Education in crisis”, UNICEF, (28 December 2020)
- School closures as a result of health and other crises are not new, at least not in the developing world, and the potentially devastating consequences are well known; loss of learning and higher drop-out rates, increased violence against children, teen pregnancies and early marriages.
What sets the COVID-19 pandemic apart from all other crises is that it has affected children everywhere and at the same time.
It is the poorest, most vulnerable children who are hurt the most when schools close and so the UN was quick to advocate for continuity of learning, and the safe opening of schools, where possible, as countries began to put lockdown measures in place: “unfortunately, the global scale and speed of the current educational disruption is unparalleled and, if prolonged, could threaten the right to education”, Audrey Azoulay, the head of the UN education agency, UNESCO, warned in March. - [F]or millions of children, the idea of an online virtual classroom is an unattainable dream. In April, UNESCO revealed startling divides in digitally based distance learning, with data showing that some 830 million students do not have access to a computer.
The picture is particularly bleak in low-income countries: nearly 90 per cent of students in sub-Saharan Africa do not have household computers while 82 per cent are unable to get online. “A learning crisis already existed before COVID-19 hit”, a UNICEF official said in June.” We are now looking at an even more divisive and deepening education crisis.”
However, in many of the developing countries where online or computer learning are not an option for most students, radio still has the power to reach millions of people and is being used to keep some form of education going. - [T]he UN was warning in August that the long-term impact of disrupted education could create a “lost generation” of children in Africa. A World Health Organization (WHO) survey of 39 sub-Saharan African countries revealed that schools were open in only six nations and partially open in 19.
By the end of the year, 320 million children were still locked out of schools worldwide, and UNICEF felt compelled to issue a call for governments to prioritize school reopening and make classrooms as safe as possible.
“What we have learned about schooling during the time of COVID is clear: the benefits of keeping schools open, far outweigh the costs of closing them, and nationwide closures of schools should be avoided at all costs”, said Robert Jenkins, UNICEF Global Chief of Education.
“Missing in School Reopening Plans: Black Families’ Trust” (2/1/2021)
[edit]Eliza Shapiro, Erica L. Green and Juliana Kim; “Missing in School Reopening Plans: Black Families’ Trust”, (Feb. 1, 2021)
- Even as more districts reopen their buildings and President Biden joins the chorus of those saying schools can safely resume in-person education, hundreds of thousands of Black parents say they are not ready to send their children back. That reflects both the disproportionately harsh consequences the virus has visited on nonwhite Americans and the profound lack of trust that Black families have in school districts, a longstanding phenomenon exacerbated by the pandemic.
- Education experts and Black parents say decades of racism, institutionalized segregation and mistreatment of Black children, as well as severe underinvestment in school buildings, have left Black communities to doubt that school districts are being upfront about the risks.
“For generations, thse public schools have failed us and prepared us for prison, and now it’s like they’re preparing us to pass away,” said Sarah Carpenter, the executive director of Memphis Lift, a parent advocacy group in Tennessee. “We know that our kids have lost a lot, but we’d rather our kids to be out of school than dead.” - Though children have largely been spared by the coronavirus, federal data released last fall showed that those who have died or developed life-threatening complications have predominantly been children of color. That trend has continued this year.
- A recent poll from Education Next, a journal published by Harvard, found that low-income Black and Latino students were much more likely to be receiving fully remote instruction than higher-income white children. Black parents were 19 percentage points less likely than white ones to choose in-person learning when the option was available. Latino parents were eight percentage points less likely.
- “Covid-19 has blown the doors off our schools and the walls off our classrooms,” Sonja B. Santelises, the chief executive of Baltimore City Public Schools, which began reopening in November, wrote in a recent opinion article. “No longer are our practices hidden behind doors or buried in the pages of policy and collective bargaining agreements; they are now in full view on a screen.” She added, “And our parents are watching.”
- Thousands of Black students have returned to classrooms in recent months. Remote learning has been disastrous for many children of color in particular, and data has shown that students are falling behind in key subjects. That could undermine decades of work by local school districts and the federal government to narrow the achievement gap between Black and white students.
- In many cities and districts, Latino and Asian-American families are also less likely than white families to send their children back. Asian-Americans have opted out of in-person classes at the highest rates of any ethnic group in New York City. Latino families in Chicago were most likely to say they would keep their children at home when schools reopened.
- Bernita Bradley, a longtime activist for public school families in Detroit, said longstanding issues around schooling did not change during the pandemic. Many Black families still see the education system as punitive — for example, the district has sent threatening emails about parents’ turning on their children’s cameras during virtual classes.
In Detroit, 16 percent of Black children returned to in-person classes in the fall, before schools shuttered again, compared with 27 percent of white children. White students make up only about 2 percent of the district over all. Recent surveys showed that more Detroit parents were willing to consider in-person learning when the city reopens schools this month.
Ms. Bradley, who said she helped the Detroit school system survey parents and connect with families during the pandemic, said those numbers showed the generational trauma suffered by the community.
“We have people who are working 40-50 hours a week to make the bare minimum, and they’re taking care of four to five children,” she said. “All of that stems from education.”
Public health
[edit]Emergency services
[edit]
- "We've had some very challenging situations over the last couple of weeks, where hospitals have had their oxygen deliveries disrupted with hours delay, putting them in a situation where they've had very low oxygen supplies," Mary Mayhew, president and CEO of the Florida Hospital Association, told CNN. "Hospitals are using 3-4 times the amount of oxygen they would normally use," she added.
- Mary Mayhew as quoted by Amanda Sealy and Hollie Silverman in ”This is how to prevent another 100,000 Covid deaths by December, Fauci says”, CNN, (Updated 6:29 AM ET, Mon August 30, 2021)
- Among health-care workers treating patients with COVID-19, a Chinese study reported high rates of depression (50%), anxiety (45%), insomnia (34%), and distress (72%). These findings were supported by a systematic review of 13 studies including more than 33 000 participants. Studies from Italy and France reported a high prevalence of depressive symptoms, post-traumatic stress disorder, and burnout; risk factors for adverse psychological outcomes included younger age, female sex, being a nurse, and working directly with patients with COVID-19. The long-term effect on the health of those working in health care remains to be seen.
- Sangeeta Mehta, Flavia Machado, Arthur Kwizera, Laurent Papazian, Marc Moss, Élie Azoulay, Margaret Herridege; “COVID-19: a heavy toll on health-care workers”, The Lancet, (February 05, 2021), Volume 9, Issue 3, pp.226-228
- You cannot outrun the game clock with this pandemic. This virus will find you and, unfortunately, many of the outcomes are very sad. Look at what's happening right now in the US. We have health care systems around the country, including in my home state of Minnesota, that are hanging on by a thread. We've seen health care systems virtually broken by this pandemic. They just couldn't provide critical care to non-Covid patients.
- Michael Osterholm as quoted by Peter Bergen in “The infectious disease expert who warned us 800,000 Americans would die of Covid-19”, CNN, (Dec 11, 2021)
“In Ambulances, an Unseen, Unwelcome Passenger: COVID-19” (1/25/2021)
[edit]“In Ambulances, an Unseen, Unwelcome Passenger: COVID-19”, “Associated Press”, (Jan 25, 2021)
- For EMTs Thomas Hoang and Joshua Hammond, the coronavirus is constantly close. COVID-19 has become their biggest fear during 24-hour shifts in California's Orange County, riding with them from 911 call to 911 call, from patient to patient.
They and other EMTs, paramedics and 911 dispatch-ers in Southern California have been thrust into the front lines of the national epicenter of the pandem-ic. They are scrambling to help those in need as hospitals burst with a surge of patients after the holi-days, ambulances are stuck waiting outside hospitals for hours until beds become available, oxygen tanks are in alarmingly short supply and the vaccine rollout has been slow. - Statistics on COVID-19 cases and deaths among EMTs and paramedics — especially ones employed by private companies — are hard to find. They are considered essential health care workers but rarely receive the pay and protections given to doctors and nurses.
- Unlike doctors and nurses, first responders must go inside homes. They walk into hot zones where everyone in a household is sick, where the virus is in the air. They lift immobile patients onto gurneys, their masked faces just inches apart.
They race to hospitals already overwhelmed with sick people, sometimes only to wait hours outside before their patient can be admitted. And then they do it all again when the next 911 call comes in. - When an EMT reports a positive COVID-19 test, the dispatchers must find a way to cover the ambulance's calls if the whole crew must quarantine. When one household has multiple coronavirus patients requiring two ambulances, the dispatchers have to plug the hole.
Their greatest fear is what's called a “level zero” — when there are no ambulances left to send to an emergency. In Los Angeles County, one of the nation's hardest-hit counties during the pandemic, the fear becomes a regular reality.
Communicable illness
[edit]- To understand the additive effects of behaviour and immunity, consider that this flu season has been unusually mild. “Influenza is probably not less transmissible than COVID-19,” Scarpino says. “Almost certainly, the reason why flu did not show up this year is because we typically have about 30% of the population immune because they’ve been infected in previous years, and you get vaccination covering maybe another 30%. So you’re probably sitting at 60% or so immune.” Add mask wearing and social distancing, and “the flu just can’t make it”, Scarpino says. This back-of-the-envelope calculation shows how behaviour can change the equation, and why more people would need to be immunized to attain herd immunity as people stop practising behaviours such as social distancing.
- Christie Aschwanden, “Five reasons why COVID herd immunity is probably impossible”, Nature, (18 March 2021), 591, pp. 520-522
- The coronavirus pandemic has dealt measles-control efforts another huge blow. On 26 March, SAGE recommended that countries temporarily suspend all preventive mass-vaccination campaigns, including those for measles. Already, 23 countries have suspended scheduled measles campaigns, and others will probably follow suit, says Linkins. This means that 78 million children will not be vaccinated as planned, he says. The DRC, however, is continuing its outbreak response.
“We must protect vulnerable populations from the spread of COVID-19,” Linkins says, but limiting measles-immunization activities will create “dangerous immunity gaps”. Modellers are just beginning work to estimate the impact of COVID-19 on measles control, but it is clear that countries must be able to resume their campaigns quickly after the pandemic subsides, he says.
With campaigns cancelled and global measles-immunization rates for just one dose of vaccine stalled at 86%, the unrelenting cycle of outbreaks will continue. This DRC outbreak will subside, but Masresha says it will be a “temporary victory”: the virus will rebound.- Leslie Roberts, “Why measles deaths are surging — and coronavirus could make it worse”, Nature, (07 April 2020; clarification 09 April 2020), 580, pp.446-447
- During the 2019 flu season from Sept. 29 to Dec. 28, the CDC reported more than 65,000 cases of influenza nationwide. During the same period this flu season, the agency reported 1,016 cases.
Health experts said that high vaccination rates against the flu – combined with social distancing, mask-wearing and hand-washing employed to stop the spread of the coronavirus – played a huge role in preventing influenza transmission.- Adrianna Rodriguez, “Record low flu cases show how COVID-19 is more contagious and 'less forgiving,' experts say”, USA Today, (January 11, 2020)
- Rehm said Americans were especially motivated to get a flu vaccine last year as health experts warned hospitals could be overwhelmed by flu and COVID-19 patients in a “twindemic” scenario.
“A lot of people in the past haven’t felt that flu was very severe and thus haven’t necessarily felt so motivated to get vaccinated,” she said. “Certainly, COVID has taught us that respiratory illnesses can be extremely severe.”- Adrianna Rodriguez quoting Susan Rehm in “Record low flu cases show how COVID-19 is more contagious and 'less forgiving,' experts say”, by Adrianna Rodriguez, USA TODAY, (January 11, 2020)
Exercise
[edit]- The online poll, conducted in February, included responses from 3,013 adults about life over the past year. A majority — 61 percent — said their weight fluctuated in 2020. Of those, 41 percent said they'd gained more weight than they wanted to: nearly 30 pounds on average. Ten percent reported gains of more than 50 pounds.
"I'm not surprised," said Kara Caruthers, an associate professor in the physician assistant program at The University of Tennessee Health Science Center College of Medicine in Memphis.
Caruthers explained that when the body feels stress, a cascade of physiological changes takes place. The body releases a hormone called cortisol, which increases insulin levels in order to maintain normal blood sugar. Higher insulin levels increase fat deposits along the waistline.
Adding to the problem, more than half of respondents said their exercise levels dropped during pandemic.- Erika Edwards, “'A collective trauma': New report details the effects of stress in America in 2020”, “NBC News”, (March 11, 2021)
- Eighteen percent of respondents actually lost more weight than they'd intended to lose: 26 pounds on average.
"We know we all do maladaptive things to cope" with stress, Evans said. "The issue is the magnitude of the problems we're seeing as a result of those behaviors."
The report also found that a growing number of adults have turned to alcohol as a coping mechanism. Nearly 25 percent of survey respondents cited pandemic stress for drinking more than usual.
But that percentage more than doubled to 52 percent among parents with children in early elementary school — a "stunning" finding, said Scott Bea, a clinical psychologist at the Cleveland Clinic.- Erika Edwards, “'A collective trauma': New report details the effects of stress in America in 2020”, “NBC News”, (March 11, 2021)
- Nearly 47 percent of women with children doing remote learning at home said their mental health had worsened during the pandemic, compared to 30 percent of men in the same position.
"Unfortunately, the way our society is structured, the burden of family life and house life still falls to women," Caruthers said. "They're managing their own careers, many also teaching school and they're not educators. I think it's been hard."- Erika Edwards, “'A collective trauma': New report details the effects of stress in America in 2020”, “NBC News”, (March 11, 2021)
- The global outbreak of COVID-19 has resulted in closure of gyms, stadiums, pools, dance and fitness studios, physiotherapy centres, parks and playgrounds. Many individuals are therefore not able to actively participate in their regular individual or group sporting or physical activities outside of their homes. Under such conditions, many tend to be less physically active, have longer screen time, irregular sleep patterns as well as worse diets, resulting in weight gain and loss of physical fitness. Low-income families are especially vulnerable to negative effects of stay at home rules as they tend to have sub-standard accommodations and more confined spaces, making it difficult to engage in physical exercise.
The WHO recommends 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity per week. The benefits of such periodic exercise are proven very helpful, especially in times of anxiety, crisis and fear. There are concerns therefore that, in the context of the pandemic, lack of access to regular sporting or exercise routines may result in challenges to the immune system, physical health, including by leading to the commencement of or exacerbating existing diseases that have their roots in a sedentary lifestyle.
- The laboratory study to investigate the physiological effect of wearing a facemask found that it significantly elevated heart rate and perceived exertion. Those participating in exercise need to be aware that facemasks increase the physiological burden of the body, especially in those with multiple underlying comorbidities. Elite athletes, especially those training for the upcoming Olympics, need to balance and reschedule their training regime to balance the risk of deconditioning versus the risk of infection. The multiple infection-control measures imposed by the Hong Kong national team training centre was highlighted to help strike this balance. Amidst a global pandemic affecting millions; staying active is good, but staying safe is paramount.
- Ashley Ying-Ying Wong, Samuel Ka-Kin Ling, , Lobo Hung-Tak Louie, , George Ying-Kan Law, ,Raymond Chi-Hung So, Daniel Chi-Wo Lee, Forrest Chung-Fai Yau, Patrick Shu-Hang Yung; “Impact of the COVID-19 pandemic on sports and exercise”, Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology, Volume 22, (October 2020), pp. 39-44
- Although moderate-levels of exercise can boost overall immunity. Intensive and prolonged physical exertion has been linked with an ‘open-window’ of impaired immunity up to 72 h after the exercise Common infections for athletes mostly comprises of dermatological related infections (especially in contact sports), upper respiratory tract infections, and gastrointestinal infections. The coronavirus is a respiratory pathogen and previous studies have shown that the risk of upper respiratory tract infections was almost six times more likely in endurance races. The underlying mechanism is not fully understood, although most studies suggest exercise significantly influences acquired immunity while evidence about the role of exercise on innate immunity is less conclusive. As the virus was also found in stool samples, contaminated environments, such as soil, may pose a threat to outdoor sporting events. There are still unknowns regarding the relationship of immunity and sports, therefore experts are still researching on the role of psychological factors (especially during competitions) as one of the large knowledge gaps.
- Ashley Ying-Ying Wong, Samuel Ka-Kin Ling, , Lobo Hung-Tak Louie, , George Ying-Kan Law, ,Raymond Chi-Hung So, Daniel Chi-Wo Lee, Forrest Chung-Fai Yau, Patrick Shu-Hang Yung; “Impact of the COVID-19 pandemic on sports and exercise”, Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology, Volume 22, (October 2020), pp. 39-44.
- The final impact of the COVID-19 pandemic on sports and exercise cannot be determined at this stage, however, the information that we gathered may provide valuable guidance to athletes and governing committees to move forward safely. COVID-19 is highly transmittable in sporting environments due to its viability, long incubation period, and milder symptoms; especially in contact sports. The essential preventive measures include minimizing human-to-human contact and practising proper personal hygiene. Athletes’ on-field own risky behaviours should be avoided to minimize unnecessary infection as close contact with others is unavoidable during contact sports. The decision to resume sporting events should correlate to the local number of cases and strict infection measures will need to be implemented at the early phases of resumption. Exercise with a facemask definitely has a toll on the human body and it is advised to adjust the exercise intensity when masked. Sports and exercise may be important, especially for competitive athletes, but safety is still paramount. Everyone should practice safe sports with the appropriate measures and prevent the further transmission of the COVID-19 pandemic.
- Ashley Ying-Ying Wong, Samuel Ka-Kin Ling, , Lobo Hung-Tak Louie, , George Ying-Kan Law, ,Raymond Chi-Hung So, Daniel Chi-Wo Lee, Forrest Chung-Fai Yau, Patrick Shu-Hang Yung; “Impact of the COVID-19 pandemic on sports and exercise”, Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology, Volume 22, (October 2020), pp.39-44.
- It is safe to exercise during the coronavirus outbreak. One should not limit the multitude of health benefits that exercise provides us on a daily basis just because there is a new virus in our environment. However, there may be some additional precautions to reduce your risk of infection. If you are a “social exerciser”, you might want to limit your exposure to exercise partners who have exhibited signs and symptoms of illness. The problem, though, is that infected people may be infectious before they exhibit symptoms. In some instances, wearing a mask while exercising may be a way to reduce your exposure. It is very important to make sure that if you are exercising on equipment in fitness facilities or gymnasiums that you make sure to disinfect the equipment before and after you use it. When done exercising, the most effective way to clean hands is to wet them with clean water, then apply soap and scrub for at least 20 s, before rinsing and drying with a clean towel. Hand sanitizers with at least 60% alcohol content may also be used, but the U.S. Centers for Disease Control and Prevention warns they are not effective against all germs. This strategy should be used at all times, not just because there is an acute viral outbreak. Avoiding touching your face and neck with your hands is also advised if you cannot disinfect them until a later time.
- Jeffrey A. Woods, as quoted by Weimo Zhu in “Should, and how can, exercise be done during a coronavirus outbreak? An interview with Dr. Jeffrey A. Woods”, J Sport Health Sci. (2020 Mar Published online 2020 Feb 4); 9(2): 105–107.
- The Coronavirus disease (COVID-19) crisis is now present in China. It started in December, 2019 and has, so far, led 213 individuals died and at least 9066 infected in China by local time 17:26, January 30, 2020. It has also spread to a number of Asian countries, as well as to Canada, France, Germany, and the United States. As a result, the Chinese government has put several major cities in Hubei Province on lockdown and has thrown plans for the Lunar New Year holiday into chaos for millions of people. On January 30, 2020, the World Health Organization also declared the COVID-19 outbreak a global health emergency because it could spread to countries that are not prepared.
Furthermore, to prevent the spread of the new and deadly virus, all cities in China now have shut down most public places and facilities, including parks, leaving many people with no place to exercise. As a result, people may wonder if one should exercise at all during the outbreak and if so, how? These questions made Journal of Sport and Health Science remember some well-known studies done by my colleague, Dr. Jeffrey A. Woods and his team at the University of Illinois at Urbana-Champaign (UIUC), in which they found a protective effect of exercise on mortality due to influenza in mice.- Weimo Zhu, “Should, and how can, exercise be done during a coronavirus outbreak? An interview with Dr. Jeffrey A. Woods”, J Sport Health Sci. (2020 Mar Published online 2020 Feb 4); 9(2): 105–107.
Mental health
[edit]- Children born during the coronavirus pandemic have significantly reduced verbal, motor and overall cognitive performance compared with children born before, a US study suggests.
The first few years of a child’s life are critical to their cognitive development. But with Covid-19 triggering the closure of businesses, nurseries, schools and playgrounds, life for infants changed considerably, with parents stressed and stretched as they tried to balance work and childcare.
With limited stimulation at home and less interaction with the world outside, pandemic-era children appear to have scored shockingly low on tests designed to assess cognitive development, said lead study author Sean Deoni, associate professor of paediatrics (research) at Brown University.
In the decade preceding the pandemic, the mean IQ score on standardised tests for children aged between three months and three years of age hovered around 100, but for children born during the pandemic that number tumbled to 78, according to the analysis, which is yet to be peer-reviewed.
“It’s not subtle by any stretch,” said Deoni. “You don’t typically see things like that, outside of major cognitive disorders.”- Natalie Grover, "Children born during pandemic have lower IQs, US study finds", The Guardian, (8/12/2012)
- Despite the need for distance, social interaction still represents an important part of mental health care for children, clinicians said. Facilities have come up with various ways to do so safely, including creating smaller pods for group therapy. Kids at Cincinnati Children's can play with toys, but only with ones that can be wiped clean afterward. No cards or board games, said Dr. Suzanne Sampang, clinical medical director for child and adolescent psychiatry at the hospital.
"I think what's different about psychiatric treatment is that, really, interaction is the treatment," she said, "just as much as a medication."
The added infection-control precautions pose challenges to forging therapeutic connections. Masks can complicate the ability to read a person's face. Online meetings make it difficult to build trust between a patient and a therapist.
"There's something about the real relationship in person that the best technology can't give to you," said Robb.- Carmen Heredia Rodriguez quoting Suzanne Sampang in “Children’s Hospitals Grapple With Wave of Mental Illness”, US News.com, (Jan 6, 2021)
“Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19” (11/2020)
[edit]Maria Elizabeth Loades, Eleanor Chatburn, Nina Higson-Sweeney, Shirley Reynolds, Roz Shafran, Amberly Brigden, Catherine Linney, Megan Niamh McManus, Catherine Borwick, and Esther Crawley; “Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19”, J Am Acad Child Adolesc Psychiatry. 2020 Nov; 59(11): 1218–1239.e3.
- The COVID-19 pandemic has resulted in governments implementing disease containment measures such as school closures, social distancing, and home quarantine. Children and adolescents are experiencing a prolonged state of physical isolation from their peers, teachers, extended families, and community networks. Quarantine in adults generally has negative psychological effects including confusion, anger, and posttraumatic distress. Duration of quarantine, fear of infection, boredom, frustration, lack of necessary supplies, lack of information, financial loss, and stigma appear to increase the risk of negative psychological outcomes. Social distancing and school closures may therefore increase mental health problems in children and adolescents, already at higher risk of developing mental health problems compared to adults at a time when they are also experiencing anxiety over a health threat and threats to family employment/income.
Social distancing and school closures are likely to result in increased loneliness in children and adolescents whose usual social contacts are curtailed by the disease containment measures. Loneliness is the painful emotional experience of a discrepancy between actual and desired social contact. Although social isolation is not necessarily synonymous with loneliness, early indications in the COVID-19 context indicate that more than one-third of adolescents report high levels of loneliness and almost half of 18- to 24-year olds are lonely during lockdown.7 There are well established links between loneliness and mental health. The purpose of this review was to establish what is known about the relationship between loneliness and mental health problems in healthy children and adolescents, and to determine whether disease containment measures including quarantine and social isolation are predictive of future mental health problems. - This rapid systematic review of 63 studies of 51,576 participants found a clear association between loneliness and mental health problems in children and adolescents. Loneliness was associated with future mental health problems up to 9 years later. The strongest association was with depression. These findings were consistent across studies of children, adolescents, and young adults. There may also be sex differences, with some research indicating that loneliness was more strongly associated with elevated depression symptoms in girls and with elevated social anxiety in boys. The length of loneliness appears to be a predictor of future mental health problems. This is of particular relevance in the COVID-19 context, as politicians in different countries consider the length of time that schools should remain closed, and the implementation of social distancing within schools.
Furthermore, in the one study that examined mental health problems after enforced isolation and quarantine in previous pandemics, children who had experienced enforced isolation or quarantine were five times more likely to require mental health service input and experienced higher levels of posttraumatic stress. This suggests that the current social distancing measures enforced on children because of COVID-19 could lead to an increase in mental health problems, as well as possible posttraumatic stress. These results are consistent with preliminary unpublished data emerging from China during the COVID-19 pandemic, where children and adolescents aged 3 to 18 years are commonly displaying behavioral manifestations of anxiety, including clinginess, distraction, fear of asking questions about the pandemic, and irritability. Furthermore, a large survey of young adult students in China has reported that around one in four are experiencing at least mild anxiety symptoms. In the United Kingdom, early results from the Co-SPACE (COVID-19 Supporting Parents, Adolescents and Children in Epidemics) online survey of more than 1,500 parents suggest high levels of COVID-19−related worries and fears, with younger children (aged 4−10 years) significantly more worried than older children and adolescents (aged 11−16 years). - It is difficult to predict the effect that COVID-19 will have on the mental health of children and young people. The subjective social isolation experienced by study participants did not mirror the current features of social isolation experienced by many children and adolescents worldwide. Social isolation was not enforced upon the participants, nor was social isolation almost ubiquitous across their peer groups and across the communities in which they lived. As loneliness involves social comparison,91 it is possible that the shared experience of social isolation imposed by disease containment measures may mitigate the negative effects. The studies were also not in the context of an uncertain but dangerous threat to health. These features limit the extent to which we can extrapolate from existing evidence to the current context. To make evidence-based decisions on how to mitigate the impact of a second wave, we need further research on the mental health impacts of social isolation in the disease containment context of a global pandemic.
Forestry and land management
[edit]- Disinfection in a cave environment is very different compared to a home or business. Microbes, including many types of viruses, occur naturally in caves. They are harmless and part of the natural ecosystem and natural processes within the cave. These microbes, particularly in some deep and old caves, can be very unusual creatures. Some produce chemicals or may have genetics that can be of benefit to people for advances in medicine, agriculture and other fields. In our National Parks caves we want to kill the Covid-19, but not impact our natural, original microbe community.
Disinfectant sprays are handy and effective since each spray disinfects a relatively large area. But, in caves that is opposite of what you want. Disinfecting a large area means killing natural cave microbes. Right now, Covid-19 comes from people and is spread to other people. So, the key is to only disinfect the areas where people travel through the cave and the facilities they use to do so.- Joel Despain, ”Covid-19 and NPS Caves”, Inside Earth Newsletter, (Fall 2020)
- The global COVID-19 pandemic will pose unique challenges to the management of wildland fire in 2020. Fire camps may provide an ideal setting for the transmission of SARS-CoV-2, the virus that causes COVID-19. However, intervention strategies can help minimize disease spread and reduce the risk to the firefighting community. We developed a COVID-19 epidemic model to highlight the risks posed by the disease during wildland fire incidents. Our model accounts for the transient nature of the population on a wildland fire incident, which poses unique risks to the management of communicable diseases in fire camps. We used the model to assess the impact of two types of interventions: the screening of a firefighter arriving on an incident, and social distancing measures. Our results suggest that both interventions are important to mitigate the risks posed by the SARS-CoV-2 virus. However, screening is relatively more effective on short incidents, whereas social distancing is relatively more effective during extended campaigns.
- Matthew P Thompson, Jude Bayham, Erin Belval; ”Potential COVID-19 Outbreak in Fire Camp: Modeling Scenarios and Interventions”, Fire, 3(3), 38; (1 August 2020)
Media
[edit]- Wikipedia's main article for Wikipedia, one of the most important (as well as most edited) articles on the project, explains that the ability to lock pages and prevent anonymous public editing on the encyclopedia that anyone can edit was the key to Wikipedia's success in weeding out disinformation on the coronavirus.
- "From Anarchy to Wikiality, Glaring Bias to Good Cop: Press Coverage of Wikipedia's First Two Decades"" (January 31, 2021) by Omer Benjakob (Haaretz) and Stephen Harrison (Slate )
“The epic battle against coronavirus misinformation and conspiracy theories” (5/21/2020)
[edit]Philip Ball & Amy Maxmen; “The epic battle against coronavirus misinformation and conspiracy theories”, Nature, (27 May 2020), 581, pp. 371-374



- On 19 March, the website Biohackinfo.com falsely claimed that Gates planned to use a coronavirus vaccine as a ploy to monitor people through an injected microchip or quantum-dot spy software. Two days later, traffic started flowing to a YouTube video on the idea. It’s been viewed nearly two million times. The idea reached Roger Stone — a former adviser to US President Donald Trump — who in April discussed the theory on a radio show, adding that he’d never trust a coronavirus vaccine that Gates had funded. The interview was covered by the newspaper the New York Post, which didn’t debunk the notion. Then that article was liked, shared or commented on by nearly one million people on Facebook. “That’s better performance than most mainstream media news stories,” says Joan Donovan, a sociologist at Harvard University in Cambridge, Massachusetts.
Donovan charts the path of this piece of disinformation like an epidemiologist tracking the transmission of a new virus. As with epidemics, there are ‘superspreader’ moments. After the New York Post story went live, several high-profile figures with nearly one million Facebook followers each posted their own alarming comments, as if the story about Gates devising vaccines to track people were true. - Every major news event comes drenched in rumours and propaganda. But COVID-19 is “the perfect storm for the diffusion of false rumour and fake news”, says data scientist Walter Quattrociocchi at the Ca’Foscari University of Venice, Italy. People are spending more time at home, and searching online for answers to an uncertain and rapidly changing situation. “The topic is polarizing, scary, captivating. And it’s really easy for everyone to get information that is consistent with their system of belief,” Quattrociocchi says. The World Health Organization (WHO) has called the situation an infodemic: “An over-abundance of information — some accurate and some not — rendering it difficult to find trustworthy sources of information and reliable guidance.”
- For researchers who track how information spreads, COVID-19 is an experimental subject like no other. “This is an opportunity to see how the whole world pays attention to a topic,” says Renée diResta at the Stanford Internet Observatory in California. She and many others have been scrambling to track and analyse the disparate falsehoods floating around — both ‘misinformation’, which is wrong but not deliberately misleading, and ‘disinformation’, which refers to organized falsehoods that are intended to deceive. In a global health crisis, inaccurate information doesn’t only mislead, but could be a matter of life and death if people start taking unproven drugs, ignoring public-health advice, or refusing a coronavirus vaccine if one becomes available.
- Researchers have been monitoring the flow of information online for years, and have a good sense of how unreliable rumours start and spread. Over the past 15 years, technology and shifting societal norms have removed many of the filters that were once placed on information, says Amil Khan, director of the communications agency Valent Projects in London, who has worked on analysing misinformation for the UK government. Rumour-mongers who might once have been isolated in their local communities can connect with like-minded sceptics anywhere in the world. The social-media platforms they use are run to maximize user engagement, rather than to favour evidence-based information. As these platforms have exploded in popularity over the past decade and a half, so political partisanship and voices that distrust authority have grown too.
To chart the current infodemic, data scientists and communications researchers are now analysing millions of messages on social media. A team led by Emilio Ferrara, a data scientist at the University of Southern California in Los Angeles, has released a data set of more than 120 million tweets on the coronavirus. Theoretical physicist Manlio De Domenico at the Bruno Kessler Institute, a research institute for artificial intelligence in Trento, Italy, has set up what he calls a COVID-19 “infodemic observatory”, using automated software to watch 4.7 million tweets on COVID-19 streaming past every day. (The actual figure is higher, but that is as many as Twitter will allow the team to track.) De Domenico and his team evaluate the tweets’ emotional content and, where possible, the region they were sent from. They then estimate their reliability by looking at the sources to which a message links. (Like many data scientists, they rely on the work of fact-checking journalists to distinguish reliable news sources or claims from unreliable ones.) Similarly, in March, Quattrociocchi and his co-workers reported a data set of around 1.3 million posts and 7.5 million comments on COVID-19 from several social-media platforms, including Reddit, WhatsApp, Instagram and Gab (known for its right-wing audience), from 1 January to mid-February. - Ferrara says that in the millions of tweets about the coronavirus in January, misinformation didn’t dominate the discussion. Much of the confusion at the start of the pandemic related to fundamental scientific uncertainties about the outbreak. Key features of the virus — its transmissibility, for instance, and its case-fatality rate — could be estimated only with large error margins. Where expert scientists were honest about this, says biologist Carl Bergstrom at the University of Washington in Seattle, it created an “uncertainty vacuum” that allowed superficially reputable sources to jump in without real expertise. These included academics with meagre credentials for pronouncing on epidemiology, he says, or analysts who were good at crunching numbers but lacked a deep understanding of the underlying science.
As the pandemic shifted to the United States and Europe, false information increased, says Donovan. A sizeable part of the problem has been political. A briefing prepared for the European Parliament in April alleged that Russia and China are “driving parallel information campaigns, conveying the overall message that democratic state actors are failing and that European citizens cannot trust their health systems, whereas their authoritarian systems can save the world.” The messages of US President Donald Trump and his administration are sowing their own political chaos. This includes Trump’s insistence on referring to the ‘Chinese’ or ‘Wuhan’ coronavirus and his advocacy of unproven (and even hazardous) ‘cures’, and the allegation by US Secretary of State Mike Pompeo that the virus originated in a laboratory, despite the lack of evidence. - The hate multiverse, the researchers say, “acts like a global funnel that can suck individuals from a mainstream cluster on a platform that invests significant resources in moderation, into less moderated platforms like 4Chan or Telegram”. As a result, Johnson says, racist views are starting to appear in the anti-vaccine communities, too. “The rise of fear and misinformation around COVID-19 has allowed promoters of malicious matter and hate to engage with mainstream audiences around a common topic of interest, and potentially push them toward hateful views,” his team says in the paper.
Donovan has seen odd bedfellows emerge in the trolling of the WHO’s director-general, Tedros Adhanom Ghebreyesus. US-based groups that often post white-nationalist content are circulating racist cartoons of him that are similar to those posted by activists in Taiwan and Hong Kong. The latter groups have long criticized the WHO as colluding with the Chinese Communist Party, because the WHO, like all United Nations agencies, considers the regions as part of mainland China. “We’re seeing some unusual alliances coming together,” Donovan says. - As misinformation grows, it sometimes becomes deadly. On Twitter in early March, technology entrepreneurs and investors shared a document prematurely extolling the benefits of chloroquine, an old malaria drug, as an antiviral against COVID 19. The document, which claimed that the drug had produced favourable outcomes in China and South Korea, was widely passed around even before the results of a small, non-randomized French trial of the related drug hydroxychloroquine were posted online on 17 March. The next day, Fox News aired a segment with one of the authors of the original document. And the following day, Trump called the drugs “very powerful” at a press briefing, despite the lack of evidence. There were small spikes in Google searches for hydroxychloroquine, chloroquine and their key ingredient, quinine, in mid-March — with the largest surge on the day of Trump’s remarks, Donovan found using Google Trends. “Just like toilet paper, masks and hand sanitizer, if there was a product to be had, it would have sold out,” she says. Indeed, it did in some places, worrying people who need the drugs to treat conditions such as lupus. Hospitals have reported poisonings in people who experienced toxic side effects from pills containing chloroquine, and such a large number of people with COVID-19 have been asking for the drug that it has derailed clinical trials of other treatments.
- Social-media platforms often rely on fact-checkers at independent media organizations to flag up misleading content. In January, 88 media organizations around the world joined together to record their fact-checks of COVID-19 claims in a database maintained by the International Fact-checking Network (IFCN), part of the Poynter Institute for Media Studies in St Petersburg, Florida (see ‘A fact-checking frenzy’). The database currently holds more than 6,000 examples, and the IFCN is now inviting academics to dig into the data. (Another site, Google’s fact-check explorer, records more than 2,700 fact-checks about COVID-19.) But some fact-checking organizations, such as Snopes, have admitted to being overwhelmed by the quantity of information they are having to deal with. “The problem with infodemics is its huge scale: collectively, we are producing much more information than what we can really parse and consume,” says De Domenico. “Even having thousands of professional fact-checkers might not be enough.”
- Communication scholar Scott Brennen at the Oxford Internet Institute, UK, and his co-workers have found that social-media companies have done a decent job of removing misleading posts, given the hard task. The team followed up 225 pieces of misinformation about the coronavirus that independent fact-checkers had collated in the IFCN or Google databases as false or misleading. In a 7 April report, the team found that by the end of March, only some 25% of these false claims remained in place without warning labels on YouTube and Facebook, although on Twitter that proportion was 59% (see go.nature.com/2tvhuj5). And Ferrara says that about 5% of the 11 million Twitter users his team has studied so far in its COVID-19 database have been shut down for violating the platform’s policies of use, and that these tended to be unusually active accounts.
But some creators of content have found ways to delay detection by social-media moderators, Donovan notes, in what she calls “hidden virality”. One way is to post content in private groups on Facebook. Because the platform relies largely on its users to flag up bad information, shares of misleading posts in private communities are flagged less often because everyone in the group tends to agree with one another, she says. Donovan used to study white supremacy online, and says a lot of ‘alt-right’ content wasn’t flagged until it leaked into public Facebook domains. Using CrowdTangle, a social-media-tracking tool owned by Facebook, Donovan found that more than 90% of the million or so interactions referring to the New York Post article about the Gates vaccine conspiracy were on private pages. - Donovan agrees, but argues that social-media companies could implement stronger, faster moderation, such as finding when posts that have already been flagged, or deleted, are revived with alternative links. In addition, she says, social-media firms might need to adjust their policies on permitting political discourse when it threatens lives. She says that health misinformation is increasingly being buried in messages that seem strictly political at first glance. A Facebook group urging protests against stay-at-home restrictions — Re-Open Alabama — featured a video (viewed 868,000 times) of a doctor saying that his colleagues have determined that COVID-19 is similar to influenza, and “it shows healthy people don’t need to shelter in place anymore”. Those messages could lead people to ignore public-health guidance and endanger many others, says Donovan. But Facebook has been slow to curb these messages because they seem to be expressing political opinions. “It’s important to demonstrate to platform companies that they aren’t moderating political speech,” Donovan says. “They need to look at what kind of health misinformation backs their claims that restrictions are unjustified.” (Facebook did not reply to a request for comment.)
- Efforts to raise the profile of good information, and slap a warning label on the bad, can only go so far, says DiResta. “If people think the WHO is anti-American, or Anthony Fauci is corrupt, or that Bill Gates is evil, then elevating an alternative source doesn’t do much — it just makes people think that platform is colluding with that source,” she says. “The problem isn’t a lack of facts, it’s about what sources people trust.”
Brennen agrees. “The people in conspiracy communities think that they are doing what they should: being critical consumers of media,” he says. “They think they are doing their own research, and that what the consensus might advocate is itself misinformation.”
That sentiment could grow if public-health authorities don’t inspire confidence when they change their advice from week to week — on facemasks, for example, or on immunity to COVID-19. Some researchers say the authorities could be doing a better job at explaining the evidence, or lack of it, that guided them.
Sexology
[edit]- For the first time in years, rates of chlamydia, gonorrhea and syphilis, which had been on track in 2020 to hit record highs in the United States, have taken an abrupt downturn.
This should be good news. The coronavirus pandemic has certainly kept more people away from bars, night clubs and large parties, reducing opportunities for unsafe sex, studies show.
But the drop is more likely a harbinger of bad news, experts in reproductive and sexual health believe. They say the pandemic has seriously hindered efforts to mitigate sexually transmitted infections that can lead to pelvic inflammatory dis-ease, chronic pain, infertility and even blindness and death in newborns. Rather than showing sexually transmitted diseases are on the run, the upbeat numbers likely signal instead that they are now going largely undetected.
In communities across the country, contact tracers for gonorrhea and syphilis, which had already been severely understaffed, have been diverted to Covid-19 cases. Eighty percent of sexual health screening clinics reported having to reduce hours or shut down altogether sometime during the pandemic, according to a survey by the National Coalition of STD Directors.- Jan Hoffman, “People Are Still Having Sex. So Why Are S.T.D. Rates Dropping?”, New York Times, (Oct. 28, 2020)
- Social scientists are exploring how the coronavirus outbreaks have affected sexual behavior. Justin Lehmiller, a social psychologist at the Kinsey Institute, which has been issuing surveys during the pandemic to about 2,000 people, gay, straight and bisexual, said that even those in continuing relationships reported having less sex in the first months. “Higher levels of stress and anxiety are pushing down de-sire,” he said. “Singles have more challenges to hooking up.”
But when doctors and nurse practitioners who work with teenagers were asked if the pandemic had slowed down their patients’ sexual activity, they replied that, anecdotally speaking, not at all. Dr. Bolan said that one New York pediatrician reported that she’d treated many teenagers for S.T.D.s.- Jan Hoffman, “People Are Still Having Sex. So Why Are S.T.D. Rates Dropping?”, New York Times, (Oct. 28, 2020)
- Even if sex has declined, researchers question how long it can remain suppressed. Dr. Lehmiller noted that online dating apps report record business. Whether that translates into sexual activity rather than virtual meet-ups is unclear, he said. If people are returning to normal levels of encounters, they may not want to admit it.
“There is shaming about traveling, social events and gatherings during the pan-demic, so sex and dating is seen as part of that,” he said.- Jan Hoffman, “People Are Still Having Sex. So Why Are S.T.D. Rates Dropping?”, New York Times, (Oct. 28, 2020)
- Dating is a complicated and often clumsy dance even in the best of times. Add in mask-wearing directives, social distancing and fear of a highly contagious virus for which there is no cure, and you get… well, an awful lot of people going out and doing some version of it anyway. A survey conducted by Everlywell — a company that makes at-home health tests — found that nearly one in four Americans ages 20 to 31 broke quarantine to have sexual contact with someone in April, when stay-at-home orders were at their peak.
- Courtney Rubin, “The New Rules of Dating”, New York Times, (July 18, 2020)
- “My best advice is to tell the date beforehand that you intend to wear a mask and would like the date to do so as well,” Dr. Helweg-Larsen wrote. “You can also practice what to say if the date is resisting (something simple like, ‘please put on your mask’ or, ‘you are protecting me with your mask’) or you can use non-verbal communication like stepping or turning away from someone.”
- Courtney Rubin, “The New Rules of Dating”, New York Times, (July 18, 2020)
- Across the globe, the coronavirus pandemic is affecting almost all aspects of daily life. To limit the spread of COVID-19 pandemic, lockdowns have been instituted in major cities and countries around the world. For this reason, people stayed isolated or self-quarantined at homes to prevent the spread of the virus and to avoid becoming infected. According to our analyses, we showed that people are finding creative ways to spend the time like watching porn at home. A sharp increase in porn searches was seen in nations where coronavirus is widespread. One of the most popular porn website reported that their traffic has steadily increased in March as the pandemic has spread, which confirms our findings. Interestingly, there was no different WRSV in nations like USA and Sweden, where regulations were never as restrictive as the ones adopted in Italy, Spain, and France.
- Fabio Zattoni, Murat Gül, Matteo Soligo, Alessandro Morlacco, Giovanni Motterle, Jeanlou Collavino, Andrea Celeste Barneschi, Marco Moschini & Fabrizio Dal Moro; “The impact of COVID-19 pandemic on pornography habits: a global analysis of Google Trends”, International Journal of Impotence Research, (28 November 2020)
- To the extent that the COVID-19 pandemic is making mortality more salient, it would make sense that a person would feel a rise in lust, which could partly explain why more porn is being consumed. Interestingly, some survey studies investigated sexual function during restrictive social distancing and found how risk perception of COVID-19 was negatively associated with frequencies of sexual activities. In particular, a higher general anxiety during COVID-19 was showed to have a negative impact on sex life and frequencies of sexual intercourse, decreased satisfaction with sex life and frequencies of sexual activity. These results could explain the use of pornography as an escape from the reality and sexual life crisis.
- Fabio Zattoni, Murat Gül, Matteo Soligo, Alessandro Morlacco, Giovanni Motterle, Jeanlou Collavino, Andrea Celeste Barneschi, Marco Moschini & Fabrizio Dal Moro; “The impact of COVID-19 pandemic on pornography habits: a global analysis of Google Trends”, International Journal of Impotence Research, (28 November 2020)
“Why the coronavirus might change dating forever” (5/25/2020)
[edit]MacKenzie Sigalos, “Why the coronavirus might change dating forever”, CNBC, (May 25 2020)
- In New York, the epicenter of the COVID-19 outbreak in the U.S., the city’s health department put out a set of guidelines entitled, “Sex and coronavirus disease.” One piece of official advice: “You are your safest sex partner.”
Dating is hard enough in the best of times. Throw in government directives like this, plus nationwide social distancing mandates, and a highly contagious virus for which there’s no cure or vaccine, and you would expect the search for love to be the last thing on everyone’s mind. But dating is thriving. - Before the pandemic, online dating fatigue was taking hold. Dating app downloads for the top 15 apps was shrinking globally, and research showed that all that swiping just made people lonelier.
The pandemic, at least by some metrics, has been great for business. Dating.com reported that global online dating was up 82% during early March, for example.
As states across the country began rolling out stay-at-home orders in March 2020, Bumble saw a 26% increase in the number of messages sent on its platform, a company spokesperson told CNBC. Tinder saw the length of conversations rise by 10-30%, and elite dating app Inner Circle saw messages rise 116% over that same time period. - Turns out, dating during a global pandemic and being a contestant on “Love is Blind” aren’t too dissimilar. Both scenarios beg the obvious question: Can you truly gauge physical chemistry in a virtual setting?
- Fisher thinks COVID-19 has given way to a new stage in the courtship process.
“You know, years ago, marriage used to be the beginning of a partnership. Now it’s the finale,” says Fisher. “All of my data show that the longer the courtship process is, the more likely people are to remain together and create a stable partnership.”
“Coronavirus has changed online dating. Here’s why some say that’s a good thing” (5/15/2020)
[edit]Courtney Vinopal, “Coronavirus has changed online dating. Here’s why some say that’s a good thing”, Nation, (May 15, 2020)
- “It’s an excellent time for singles to date,” said Helen Fisher, the chief scientific adviser to Match.com and a senior research fellow at The Kinsey Institute. “People have time. They’re not getting dressed up to go to work. And most importantly, they have something to talk about.”
Not everyone, though, is keen to get into online dating, even if spending more time than usual alone at home has made some otherwise happily single people reconsider their feelings about finding a long-term companion. Not to mention that the pandemic has ushered in mass unemployment, higher levels of stress, greater strain for single parents and worries about fatal risks from stepping outside your door — factors not necessarily conducive to romance. - Fifty years ago, a global pandemic might have hindered single people from connecting with prospects through their family, friends or faith communities. But these days, most people are connecting virtually to start anyway. “The influence of technology on our romantic and sexual lives has been so enormous,” said Justin Garcia, an evolutionary biologist and sex researcher at The Kinsey Institute. “From online dating, to texting, video chatting, sexting, etc., we have already been in the midst of a digital revolution for human courtship,” he added, so it’s not a huge surprise that singles would continue dating this way in the midst of a pandemic.
- The stay-at-home orders issued across the country have been a boon for some of the major online dating apps. “As a city goes into lockdown, engagement on OKCupid goes up,” the app’s global chief marketing officer, Melissa Hobley, said. Since March, the company has seen a whopping 700 percent increase in the amount of OKCupid users going on a virtual date. The app Hornet, which caters to the gay male community, has seen a 30-percent increase in social feed engagement since social distancing measures began in mid-March, according to CEO Christ of Wittig. And the dating app Tinder reported that it saw more engagement on March 29 than on any other day in its history, with more than 3 billion users swiping to connect with people, according to an April 1 press release.
- A study conducted by Match found that while only 6 percent of singles were using a video platform to meet a potential date before the COVID-19 outbreak, 69 percent of singles said they’d be open to chatting over video with someone they met on a dating app during quarantine as of mid-April. Twenty-two percent of these respondents even said they’d consider entering an exclusive relationship with someone they hadn’t met in person, indicating an openness to cultivating relationships mostly online. As of the end of April 23, 51 percent of users on the dating app Coffee Meets Bagel said they planned to video chat more, and 18 percent had had at least one video call with a match.
- Before the novel coronavirus hit, U.S. couples were already getting married later in life than ever be-fore. Helen Fisher said what’s happening now is increasing the amount of time people spend in a “courtship” stage even more.
“We’re seeing the emergence of a new phase in the courtship trajectory, which is meet online, talk online, then talk in person,” Fisher added. “Yes, we’re moving forward to the past. We’re getting to know somebody before the sex.” - “When your daily habits change, it’s novel. And novelty drives up dopamine in the brain,” the biological anthropologist said. “The novelty is setting up the brain, priming the brain for love. It’s a very good time for romance.”
“I truly believe this is how you need to get to know people, anyway,” Price said. “This kind of slowed us both down and made us calculate how and when we wanted to do things. It’s been fun.”
Vaccines
[edit]As Omicron Spreads, 100+ Firms in Africa, Asia & Latin America Can Make mRNA Vaccine If Tech Shared, Democracy Now!, (16 December 2021)
[edit](full interview video, sound file, & transcript)
- As the coronavirus variant Omicron spreads across the world at an unprecedented rate, a group of vaccine experts has just released a list of over 100 companies in Africa, Asia and Latin America with the potential to produce mRNA vaccine. They say it is the one of the most viable solutions to fight vaccine inequity around the world and combat the spread of coronavirus variants, including Omicron. Democracy Now!
- The new coronavirus variant Omicron is spreading across the world at an unprecedented rate. The World Health Organization warns cases of the heavily mutated variant have been confirmed in 77 countries, and likely many others that have yet to detect it.
With international infections climbing, the Biden administration is facing renewed demands to follow through on his now seven-month-old pledge to ensure companies waive intellectual property protections on coronavirus vaccines and share them with the world.
Now a group of vaccine experts has just released a list of over a hundred companies in Africa, Asia and Latin America with the potential to produce mRNA vaccines to fight COVID-19. They say it’s one of the most viable solutions to fight vaccine inequity around the world and combat the spread of coronavirus variants, including Omicron. ~ (Amy Goodman)
- The backdrop to our report is Omicron. And what Omicron means, as we still figure out how infectious it is, how severe the infection that it causes is, what we know already are a few things. We know that all existing double-dose vaccines work less well against Omicron, which means that those who’ve had two doses of a Pfizer or Moderna vaccine in the United States need a booster.
What we also know is that it’s highly transmissible and that it’s inevitably going to lead to a surge in cases, regardless of how severe they are.
What that in turn means for existing vaccine inequity, which is pretty deep — Nigeria has less than 2% of its population vaccinated as compared to countries in southern Europe, where the percentage is in the eighties — what it means is that vaccine inequity suddenly becomes worse. Why? Because everyone now needs more vaccines.
- Our report is on mRNA vaccines, because they are a remarkable technology that we haven’t yet fully understood, meaning that they are not biology-based. They don’t require cells to be grown. And it means, therefore, that they can be made faster, more easily, and, therefore, by more companies than could make the previous vaccines we used to use before 2020.
We worked on finding companies that have the facilities and the quality standards and meet the technical requirements to make mRNA vaccines. And we found, to our astonishment, that there are at least 120 companies across Africa, Asia and Latin America who could be producing millions of doses of these vaccines, which, unfortunately, in the situation that we’re in — at a precipice — is really the only way by which we can get billions more vaccines into the world in the next three to six months.
- These vaccines were created through public money — nearly $500 million of German public money from taxpayers to BioNTech, nearly a billion dollars in money from U.S. taxpayers through the government to Moderna, several billions of dollars after that in exchange for buying back vaccines at high prices. So these are very much the people’s vaccines. It’s just that they are private property.... when the Moderna CEO says, “Oh, anyone can make the Moderna vaccine,” he’s being a bit disingenuous... It’s not really possible to do that. The way vaccines work and the way regulation around vaccines work is that they need to be made with authorization and a license. Moderna and Pfizer or BioNTech... need to authorize companies to make their vaccine... to share an instruction manual as to how to do it... The problem is... it loosens Moderna and Pfizer and BioNTech’s stranglehold on these vaccines... It undercuts the massive tens of billions of dollars of profit and revenue that they can earn off selling to poor countries in the next couple of years, once they’re done with rich countries... which is why... ~ Achal Prabhala
- We’re asking the U.S. and German governments instead to say, “Look, in the face of this intransigence, it’s time to use emergency laws... that you can use, that you have the moral and legal power to put into effect, and end this pandemic for us and bring us out of this incredible cycle of hell. ~ Achal Prabhala
War
[edit]- Ten days ago, I issued an appeal for an immediate ceasefire in all corners of the globe to reinforce diplomatic action, help create conditions for the delivery of lifesaving aid and bring hope to places that are among the most vulnerable to the COVID-19 pandemic. This call was rooted in a fundamental recognition: There should be only one fight in our world today, our shared battle against COVID-19.
We know the pandemic is having profound social, economic and political consequences, including relating to international peace and security. We see it, for example, in postponement of elections or limitations on the ability to vote, sustained restrictions on movement, spiralling unemployment and other factors that could contribute to rising discontent and political tensions. In addition, terrorist or extremist groups may take profit from the uncertainty created by the spread of the pandemic.
- “In many countries, conflict has made it more difficult to control the spread of the virus and care for infected people,” Mark Lowcock, the top U.N. relief official, told the Security Council on Tuesday as it met to discuss the protection of civilians in armed conflicts.
- Mark Lowcock as quoted by Rick Gladstone in “Armed conflicts have helped the virus spread, a U.N. official says.”, New York Times, (May 26, 2021)
Women's studies
[edit]- Women comprise 70% of the global health and social care workforce, putting them at risk of infection and the range of physical and mental health problems associated with their role as health professionals and carers in the context of a pandemic. The pandemic exacerbated gender inequities in formal and informal work, and in the distribution of home responsibilities, and increased the risk of unemployment and domestic violence. While trying to fulfil their professional responsibilities, women had to meet their families' needs, including childcare, home schooling, care for older people, and home care. Burdened by these obligations, women had reduced academic productivity relative to men, as evidenced by fewer women being part of the cohort producing new knowledge about the pandemic. There was a disconnect between the demands of parenting and the expectations of the scientific community, as shown by ultra-short timelines for COVID-19-related grant proposals, which further deepened the divide between women and men.
- Sangeeta Mehta, Flavia Machado, Arthur Kwizera, Laurent Papazian, Marc Moss, Élie Azoulay, Margaret Herridege; “COVID-19: a heavy toll on health-care workers”, The Lancet, (February 05, 2021), Volume 9, Issue 3, pp.226-228
Lockdowns/self-isolation
[edit]- Without the mitigation effects offered through quarantine and isolation, the actual progress of the disease in the rest of the world will certainly be much more devastating than the harrowing scenes witnessed to date in China, Europe, and the United States. Moreover, workers involved in informal and precarious labor often live in slums and overcrowded housing — ideal conditions for the explosive spread of the virus.
- Adam Hanieh, This is a Global Pandemic – Let’s Treat it as Such, 27 March 2020, Verso Books
- Social distancing has become the primary strategy to contain the coronavirus outbreak, with countries such as Italy enforcing complete restrictions, and others like India issuing a range of advisories on avoiding non-essential contact, and restricting large gatherings and events. Social media is also abuzz about how to avoid boredom at home. However, there are a variety of occupations, mostly informal, which involve acute social contact and are still running full swing around us.
- Neethi P., How the Coronavirus Outbreak Is Also a Socio-Economic Inequality Issue, 23 March 2020, co-written with Anant Kamath, The Wire
- Radical containment measures have been used to curb the pandemic in some affected countries. The approach taken in South Korea was especially effective, done by rapidly applying extensive testing, quarantine, and contact tracing of individuals from a large church group in the early stages of the outbreak. Also, schools were closed, and all international arrivals were quarantined for 2 weeks. China, South Korea, and Singapore show that mitigation using a combination of contact tracing and rigorous social distancing measures is possible. However, new outbreaks have started to occur in each of these countries and renewed control measures have been implemented
Countries such as Denmark, Italy, Spain, and Germany have relied mostly on social distancing and hygiene measures, in population lockdowns of various magnitudes of intensity. Such draconic measures were used when the epidemics were progressing too fast and capacity for effective case identification, contact tracing, and containment became impossible. The consensus is that rigorous mitigation measures are needed early to slow down SARS-CoV-2 transmission. Drastic measures of quarantine and mobility restrictions put in place by China, Europe, and the USA are no different than those used for plague in the 14th century. The COVID-19 pandemic so far has shown that such measures could possibly halt the pandemic if individuals follow the specific country guidelines.- Eskild Petersen, Marion Koopmans, Unyeong Go, Davidson H Hamer, Nicola Petrosillo, Francesco Castelli, Merete Storgaard, Sulien Al Khalili, Lone Simonsen; “Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics”, The Lancet, Volume 20, ISSUE 9, e238-e244, (September 01, 2020)
- Pandemics don’t always trigger social unrest, but they can do, by throwing into relief the very inequalities that caused them. That’s because they hit the poor hardest – those in low-paid or unstable employment, who live in crowded accommodation, have underlying health issues, and for whom healthcare is less affordable or less accessible. This was true in the past and remains so today. During the 2009 flu pandemic the death rate was three times higher in the poorest fifth of England’s population than in the richest. Covid-19 is showing no signs of departing from the pattern, which, because of the way the socioeconomic dice fall, also has a racial dimension. But there is something brand new about this pandemic, which has never been seen before in the history of humanity – and that is our unprecedented global experiment in lockdown. These lockdown measures are designed to slow the spread of the disease, relieve the burden on health systems and ultimately save lives – and it looks as if they may be doing that. But they may also be exacerbating social inequalities themselves.
- In India there have been reports of deaths among unemployed migrant workers returning home in search of food; many countries, including the US, have seen workers taking industrial action, and anger has been expressed in rural communities over wealthy city-dwellers retreating to their second homes for the duration. Governments should keep an eye on these developments, in weighing up when and how to lift the lockdown, because even if it’s difficult to argue today that the cure is worse than the disease, the cure might provoke an entirely different malaise – and history teaches us that no society is immune to that. That’s the symptomatic treatment. In the long term, of course, they – and we – should address the dreadful inequality in our societies, which this pandemic is picking apart with a lethal scalpel.
- Enough is enough. go home and stay home.
- Justin Trudeau, himself in self-isolation since his wife had tested positive, scolded Canadians who did not stay home
“Inferring the effectiveness of government interventions against COVID-19” (12/15/2020)
[edit]Jan M. Brauner, Sören Mindermann, Mrinank Sharma, David Johnston, John Salvatier, Tomáš Gavenčiak, Anna B. Stephenson, Gavin Leech, George Altman, Vladimir Mikulik, Alexander John Norman, Joshua Teperowski Monrad, Tamay Besiroglu, Hong Ge, Meghan A. Hartwick, Yee Whye Teh, Leonid Chindelevitch, Yarin Gal, Jan Kulveit; “Inferring the effectiveness of government interventions against COVID-19”, Science, (15 Dec 2020)
- Worldwide, governments have mobilized resources to fight the COVID-19 pandemic. A wide range of nonpharmaceutical interventions (NPIs) has been deployed, including stay-at-home orders and the closure of all nonessential businesses. Recent analyses show that these large-scale NPIs were jointly effective at reducing the virus’ effective reproduction number, but it is still largely unknown how effective individual NPIs were. As more data become available, we can move beyond estimating the combined effect of a bundle of NPIs and begin to understand the effects of individual interventions. This can help governments efficiently control the epidemic, by focusing on the most effective NPIs to ease the burden put on the population.
- Our model enabled us to estimate the individual effectiveness of each NPI, expressed as a percentage reduction in Rt. We quantified uncertainty with Bayesian prediction intervals, which are wider than standard credible intervals. These reflect differences in NPI effectiveness across countries among several other sources of uncertainty. Bayesian prediction intervals are analogous to the standard deviation of the effectiveness across countries, rather than the standard error of the mean effectiveness. Under the default model settings, the percentage reduction in Rt (with 95% prediction interval) associated with each NPI was: limiting gatherings to 1000 people or less: 23% (0 to 40%); to 100 people or less: 34% (12 to 52%); to 10 people or less: 42% (17 to 60%); closing some high-risk face-to-face businesses: 18% (−8 to 40%); closing most nonessential face-to-face businesses: 27% (−3 to 49%); closing both schools and universities in conjunction: 38% (16 to 54%); and issuing stay-at-home orders (additional effect on top of all other NPIs): 13% (−5 to 31%). Note that we were not able to robustly disentangle the individual effects of closing schools and closing universities since these NPIs were implemented on the same day or in close succession in most countries [except Iceland and Sweden, where only universities were closed]. We thus reported “schools and universities closed in conjunction” as one NPI.
- We categorized NPI effects into small, moderate, and large, which we define as a posterior median reduction in Rt of less than 17.5%, between 17.5 and 35%, and more than 35% (vertical lines in Fig. 4). Four of the NPIs fell into the same category across a large fraction of experimental conditions: closing both schools and universities was associated with a large effect in 96% of experimental conditions, and limiting gatherings to 10 people or less had a large effect in 99% of conditions. Closing most nonessential businesses had a moderate effect in 98% of conditions. Issuing stay-at-home orders (i.e., in addition to the other NPIs) fell into the “small effect” category in 96% of experimental conditions. Three NPIs fell less clearly into one category: Limiting gatherings to 1000 people or less had a moderate-to-small effect (moderate in 81% of conditions) while limiting gatherings to 100 people or less had a moderate-to-large effect (moderate in 66% of conditions). Finally, closing some high-risk businesses, including bars, restaurants, and nightclubs had a moderate-to-small effect (moderate in 58% of conditions). Limiting gatherings to 1000 people or less was the NPI with the highest variation in median effectiveness across the experimental conditions, which may reflect the NPI’s partial collinearity with limiting gatherings to 100 people or less.
- Business closures and gathering bans both seem to have been effective at reducing COVID-19 transmission. Closing most nonessential face-to-face businesses was only somewhat more effective than targeted closures, which only affected businesses with high infection risk, such as bars, restaurants, and nightclubs. Therefore, targeted business closures can be a promising policy option in some circumstances. Limiting gatherings to 10 people or less was more effective than limits of up to 100 or 1000 people and had a more robust effect estimate. Note that our estimates are derived from data between January and May 2020, a period when most gatherings were likely indoors due to weather.
Whenever countries in our dataset introduced stay-at-home orders, they essentially always also implemented, or already had in place, all other NPIs in this study. We accounted for these other NPIs separately and isolated the effect of ordering the population to stay at home, in addition to the effect of all other NPIs. In accordance with other studies that took this approach, we found that issuing a stay-at-home order had a small effect when a country had already closed educational institutions, closed nonessential businesses, and banned gatherings. In contrast, Flaxman et al. and Hsiang et al. included the effect of several NPIs in the effectiveness of their stay-at-home order (or “lockdown”) NPIs and accordingly found a large effect for this NPI. Our finding suggests that some countries may have been able to reduce Rt to below 1 without a stay-at-home order by issuing other NPIs. - We found a large effect for closing schools and universities in conjunction, which was remarkably robust across different model structures, variations in the data, and epidemiological assumptions. It remained robust when controlling for NPIs excluded from our study. Our approach cannot distinguish direct effects on transmission in schools and universities from indirect effects, such as the general population behaving more cautiously after school closures signaled the gravity of the pandemic. Additionally, since school and university closures were implemented on the same day, or in close succession in most of the countries we study, our approach cannot distinguish their individual effects. This limitation likely also holds for other observational studies that do not include data on university closures and estimate only the effect of school closures. Furthermore, our study does not provide evidence on the effect of closing preschools and nurseries.
Previous evidence on the role of pupils and students in transmission is mixed. Although infected young people (aged ca. 12 to 25) are often asymptomatic, they appear to shed similar amounts of virus as older people, and might therefore infect higher-risk individuals. Early data suggested that children and young adults had a notably lower observed incidence rate than older adults—whether this was due to school and university closures remains unknown. In contrast, the recent resurgence of cases in European countries has been concentrated in the age group corresponding to secondary school and higher education (especially the latter), and is now spreading to older age groups as well as primary-school-aged children. Primary schools may be generally less affected than secondary schools, perhaps partly because children under the age of 12 are less susceptible to SARS-CoV-2. - [C]losing schools and universities in conjunction seems to have greatly reduced transmission, but this does not mean that reopening them will necessarily cause infections to soar. Educational institutions can implement safety measures such as reduced class sizes as they reopen. However, the nearly 40,000 confirmed cases associated with universities in the UK since they reopened in September 2020 show that educational institutions may still play a large role in transmission, despite safety measures.
See also
[edit]- Coronavirus recession
- COVID-19 pandemic deaths
- COVID-19 vaccine
- Disease X
- Evacuations related to the COVID-19 pandemic
- Hydroxychloroquine
- Immune system
- Management of COVID-19
- Shortages related to the COVID-19 pandemic
- Travel restrictions related to the COVID-19 pandemic
- Vaccines
